Priya Badkar, Borligegowda Viswanatha
Otorhinolaryngology Department, Bangalore Medical College & Research Institute, Bangalore, India
Correspondence to: Borligegowda Viswanatha, Otorhinolaryngology Department, Bangalore Medical College & Research Institute, Bangalore, India.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
AIM: To evaluate the effect of mastoid drilling on hearing in the contralateral normal ear and to determine the type and duration of hearing loss. METHODS: 110 patients with chronic otitis media undergoing mastoidectomy were included in the study. Preoperative pure tone audiometry and bone conduction thresholds were compared with those done on day 1, day 3, day 7, 1 month and 3 months postoperatively. RESULTS: Statistically significant increase in pure tone audiometry and bone conduction thresholds were seen on post operative days 1, 3 and 7. They were seen to come back to normal at 1 month and 3 months. CONCLUSION: Tympanomastoid surgery and drilling during ear surgery can cause significant acoustic trauma and transient sensory hearing loss to the contralateral ear. Drill generated noise cannot be lowered to a great extent. Routine mastoidectomy in patients with dry ear should be discouraged unless necessary.
Keywords:
Mastoid drilling, Sensorineural hearing loss, Contralateral normal ear
Cite this paper: Priya Badkar, Borligegowda Viswanatha, Effect of Mastoid Drilling on Sensory Neural Hearing Component of Normally Functioning Contralateral Ear, Research in Otolaryngology, Vol. 8 No. 2, 2019, pp. 15-19. doi: 10.5923/j.otolaryn.20190802.01.
1. Introduction
Bone drilling is an essential procedure during mastoid surgery and it exposes both the cochlea to acoustic trauma. Acoustic trauma is a well known factor which can lead to sensorineural hearing loss (SNHL). During otological surgeries acoustic trauma can result because of exposure to loud noise. [1] Noise induced hearing loss may result when drill and surgical tools are used on or adjacent to ossicular chain and stapes footplate and during mastoid drilling. [2]Noise exposure results in dysfunction of the outer hair cells, which may produce a temporary hearing loss on surgery applied or opposite ear. In mastoid surgery, higher levels of noise induced hearing loss are expected due to longer drilling time. This study aims at determining the effect of drilling on the contralateral normal ear and if any, to determine if it is temporary or permanent.
2. Materials and Methods
The study was conducted on patients undergoing mastoidectomy at Sri Venkateshwara ENT Institute, Victoria hospital, Bangalore Medical College and Research Institute, Bangalore during the period from November 2016 to October 2018.Patients more than 15 years of age, having unilateral chronic otitis media with opposite ear being normal were included in the study.Exclusion criteria was considered in the patients with less than 15 yrs of age, patients having bilateral ear disease and patients with existing sensorineural hearing loss.
3. Methodology
After obtaining clearance and approval from the institutional ethics committee and informed written consent, the patients with chronic otitis media undergoing mastoidectomy who fulfill the inclusion criteria were enrolled in the study.Detailed history, systemic and otological examination was done. Patients were subjected to pure tone audiometry. Micromotor unit for drilling was used in all cases. It consists of a console with power supply, the micromotor portion and the foot switch. An adjustable knob is used to increase or decrease the rotation speed (30,000-40,000rpm). It can go up to 80,000rpm. Cutting and diamond burrs of various sizes were used.All patients who were willing to undergo unilateral mastoidectomy who fulfil the inclusion criteria were followed up with pure tone audiometry on day 1, 3, 7 post operatively. Intaoperatively, status of mastoid pneumatisation was noted. Time duration for drilling was recorded. Patients with hearing loss were followed up on 1 and 3 months to assess the progression of hearing loss.Interpretation of Audiogram: In this study the degree of sensorineural hearing loss is based on the difference in pure tone averages (in decibels) of bone conduction thresholds at 500, 1000, 2000 Hz between diseased and normal ear.
4. Results
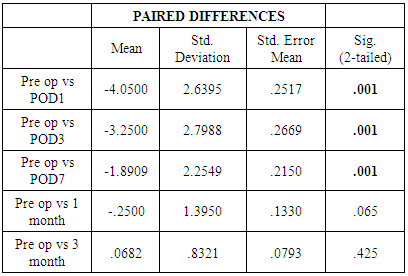
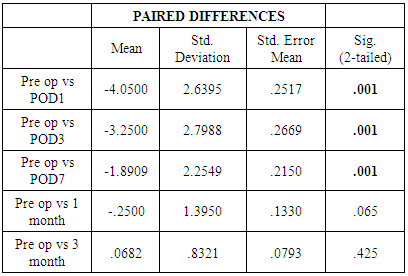
Our study included 110 patients with unilateral chronic otitis media who presented to our outpatient department and underwent mastoid exploration and tympanoplasty during the study period.In this study Paired-Samples T Test procedure is used to test the significance difference between the effect of drilling preoperative and postoperative on the same patient. Here p value is the probability of t-statistic.(1) AGE DISTRIBUTION: In our study mean age of patients in was 31.74±10.65 years (range 15-59) with majority of patients in age group of 15-30 years [figure 1]. | Figure 1. Pie chart showing age distribution of patients |
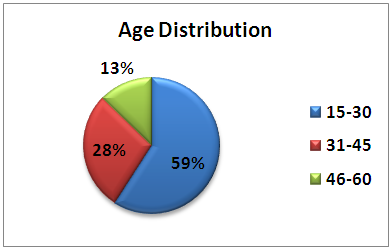
(2) GENDER DISTRIBUTION: In our study, both genders had equal distribution (Male: Female=1:1) [figure 2].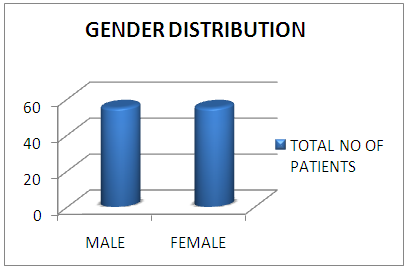 | Figure 2. Bar graph showing gender distribution of patients |
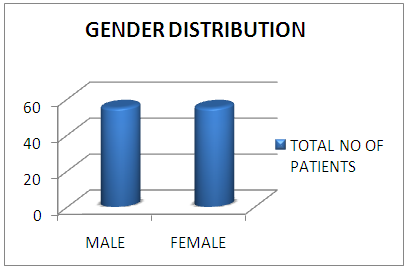
(3) SIDE AFFECTED: In our study, Left ear was affected by chronic otitis media in 58% of patients and Right ear in 42% [figure 3].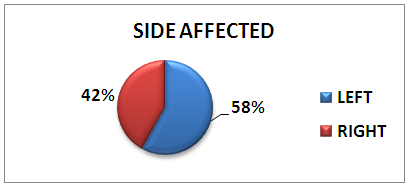 | Figure 3. Pie chart showing affected side |
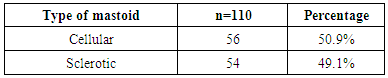
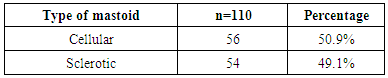
(4) TYPE OF MASTOID PNEUMATISATION:Intra operatively, 56 (50.9%) patients had well pneumatised mastoid and sclerotic mastoid in 54 patients (49.1%) [Table 1].Table 1. Type of mastoid pneumatisation
 |
| |
|
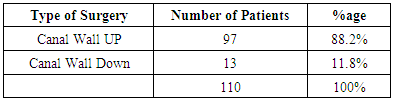
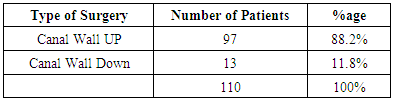
(5) TYPE OF SURGERY:In our study, 97 patients underwent canal wall up mastoidectomy (88.2%) and 13 patients underwent canal wall down mastoidectomy [Table 2].Table 2. Type of surgery
 |
| |
|
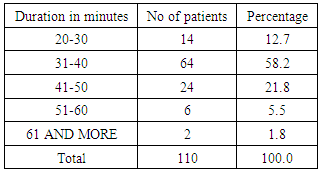
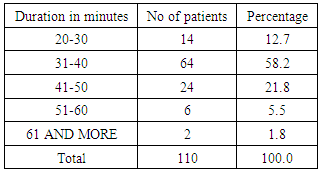
(6) DURATION OF DRILLINGDuration of the drilling was recorded. Mean drilling duration was 38.51±8.08 minutes (range 20-65 minutes) [Table 3].Table 3. Duration of drilling
 |
| |
|
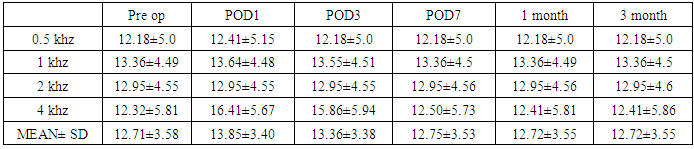
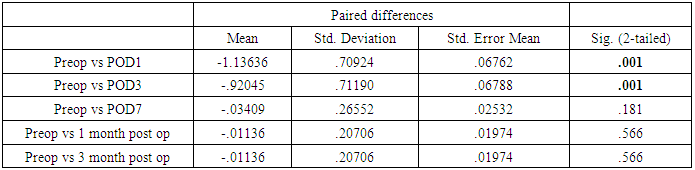
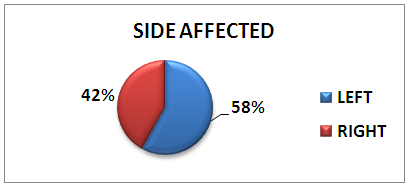
(7) BONE CONDUCTION THRESHOLDPaired T Test is used to measure the significance between preoperative bone conduction threshold and post operative bone conduction threshold values which are measured on postoperative day 1, post operative day 3, post operative day7, 1 month and 3 month. There was statistical significant changes observed between preoperative bone conduction threshold and bone conduction threshold on POD1, POD3 (p <0.05) [Table 4 & 5].Table 4. Pre operative and Post operative Bone Conduction Threshold
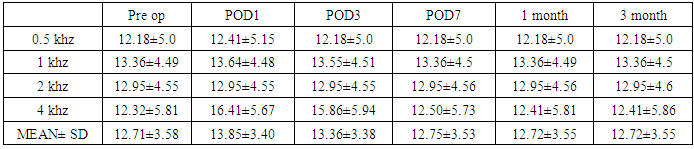 |
| |
|
Table 5. Paired Sample T Test for Bone Conduction Threshold
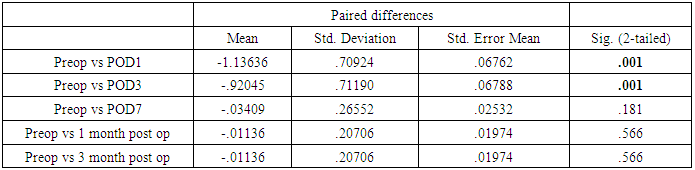 |
| |
|
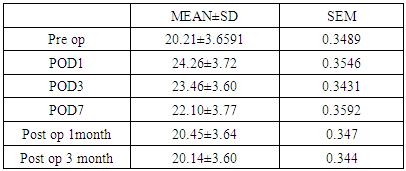
(8) Pure Tone AudiometryStatistically significant changes are seen in preoperative pure tone audiometric values compared to postoperative values measured on POD1, POD3, POD7 (p<0.05). These changes were seen to be normalized at 1 month and 3 months postoperatively [Table 6 & 7].Table 6. Preoperative and post operative Pure Tone Audiometry
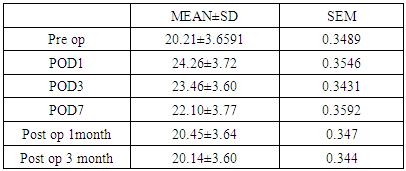 |
| |
|
Table 7. Paired Sample T Test for Pure Tone Audiometry
 |
| |
|
Hence the increase in pure tone audiometry and bone conduction thresholds was seen to be a transient change.
5. Discussion
The main aim of this study was to determine the effect of drill noise on the contralateral ear in patients undergoing tympanomastoid surgery.There are some studies specifying that the incidence of sensorineural hearing loss varies between 1.2% and 4.5% in the ear where drilling has been done. [3] The manner in which the variables like type of burr, burr size, rotation speed and site of drilling influence bone-conducted, drill-generated noise levels in ear surgery has been investigated [4]. When a drill is used during a mastoid surgery, the noise level in the cochlea is calculated from vibration measurements on intact skulls of human cadavers and temporal bones. [5] Everytime a drill is used, the ipsilateral cochlea is exposed to noise levels of about 100 dB and the contralateral cochlea to levels of 5 to 10 dB lower. [6]Total 110 patients were included in our study. In our study mean age of patients in was 31.74±10.65 years (range 15-59) with majority of patients in age group of 15-30 years. It is similar to study by Pal [7] which included patients with age ranging 13-62 years with a mean age 31.36 years. Both male and female had equal (50%) distribution in our study (M : F = 1:1) which is comparable to study by Chandregowda et al. wherein male to female ratio is 1:1. [8]Depending on the pathology involved, patients underwent canal wall up or canal wall down procedure with tympanoplasty. Out of 110 patients, 97 patients underwent canal wall up and tympanoplasty procedure (88.2%), the rest 13 patients canal wall down and tympanoplasty (11.8%).Intra operatively type of pneumatisation of mastoid was noted. 56 (50.9%) patients had well pneumatised mastoid and 54 patients (49.1%) had sclerotic mastoid. Duration of the drilling was recorded. Mean drilling duration was 38.51±8.08 minutes (range 20-65 minutes).Palva and Sorri reported that they found SNHL on the contralateral side during first week post-operatively and concluded that it increased with increased duration of surgery. [9] This is similar to our study in which statistically significant changes were seen post operative day1, day3 and day7. Our study showed statistically significant correlation between preoperative and postoperative bone conduction thresholds.Schick et al. conducted a retrospective analysis of temporary sensory hearing deficits after ear surgery. In this study, thresholds at 500 Hz, 1000 Hz, 2000 Hz and 4000 Hz were analysed in 393 patients before, the first 4 days and 3 weeks after ear surgery to evaluate possible temporary threshold shifts. They concluded that slight temporary threshold shifts could be observed at 2000 Hz and 4000 Hz after ear surgery. Use of the drill and manipulation at the ossicular chain usually results in no significant sensory hearing deficit. [10]Biswas et al. concluded that sensory neural hearing loss after mastoid surgery is not due to noise generated by the drill. In the event of any hearing loss during this period, other causes should be sought. [11]Holmquist et al. presented a simple technique for measuring sound intensities during surgery. They stressed that drill-generated noise must be regarded as a risk to the cochlea during ear surgery. They suggested that real sound levels in the air close to the drill were not appreciably higher than the equivalent noise levels reaching the cochlea through the skull by bone conduction. [12] Spencer et al. conducted a study on 5 patients who underwent mastoidectomy. Postoperative pure tone audiometry was carried out on each patient 48 hours after surgery. No evidence of a bone conduction threshold shift was detected in any of the patients in either the operated or the contralateral ear. [13]Exposure to high levels of noise is known to be harmful to the ear. Cochlear injury may be sustained acutely from sudden-impact noise or may develop gradually over time if noise is prolonged over time.Kylen et al. stated that drill induced noise during ear surgery may result in postoperative high-tone sensory neural hearing loss. They measured a noise level of 100 dB in the ipsilateral cochlea and 90-95 dB in contralateral side. The noise level was highest using large burrs and it was higher with cutting than with diamond burrs. The noise level was lowest, about 70-80 dB, using a 2 mm diamond burr. Variations in rotation speed and site of drilling did not appear to influence the noise level. They supported the view that manipulation of the ossicular chain may result in a predominantly lower-frequency threshold shift and bone conducted noise trauma may cause high tone loss in some cases. [6]Domanech et al. conducted a study to demonstrate sensorineural high frequency hearing loss after drill generated acoustic trauma in tympanoplasty. 24 patients with normal bone conduction audiometric thresholds scheduled for tympanoplasty were assessed with an electro-stimulation, bone conduction high-frequency audiometer which can measure hearing frequencies up to 20 kHz before and after surgery. It was concluded that drilling of the temporal bone could impair the hearing level in the high frequencies in a significant number of patients. It was suggested in these studies that drill generated noise transmitted via the bone, and not via the ossicles, in some cases might be responsible for the high-tone loss, especially since the frequency of 4000 Hz was involved in all cases. [14]Singh et al. studied the inherent risk of inner ear damage with middle ear surgeries in 60 patients. Bone conduction thresholds in different frequencies were recorded by a pure-tone audiometer both pre-operatively and post-operatively. The over-all results showed one case (1.67%) with significant or severe SNHL of more than 25 dB and ten cases (16.66%) with mild to moderate SNHL including three cases of temporary threshold shift. In majority of the cases (11.67%) 2000 and 4000 frequencies were involved. [15]Paksoy et al. in their study state that drill induced sensorineural hearing loss is one of the causes of hearing loss. [16]Alharbi et al. in their study state that one should avoid touching ossicular chain during ear surgery as a high focused acoustic energy is transmitted to inner ear causing damage in structure and deterioration of function. Spontaneous recovery could occur after acoustic trauma but may be incomplete with permanent scar formation in outer hair cells. [17]Migrov [18] et al. conducted a study to determine possible changes in the outer hair cell (OHC) function related to drill noise exposure. Drill-induced noise during mastoidectomy can cause reversible changes in DPOAE in the non-operated ear. OHC function may be diminished during the period after mastoid surgery and last for more than 1 month. Five fresh cadaveric temporal bones were used. Stapes displacement was measured using laser doppler vibrometry during short drilling episodes. Diamond and cutting burrs of different diameters were used. The effect of the drilling on stapes footplate displacement was compared with that generated by an acoustic signal. The equivalent noise level (dB sound pressure level equivalent [SPL eq]) was thus calculated. This study suggests that drilling on the ossicular chain can produce vibratory force that is analogous with noise levels known to produce acoustic trauma. For the same type of burr, the larger the diameter, the greater the vibratory force, and for the same size of burr, the cutting burr creates more vibratory force than the diamond burr. The cutting burr produces greater high frequency than lower-frequency vibratory energy.In a study done by Man A et al. the pre and postoperative bone conduction thresholds for the frequencies 0.25 through 16 kHz was compared in 46 ears in which a high-speed ear drill was used. In 15 of these, thresholds were also obtained in the contralateral ear. There was no statistically significant postoperative threshold change at any single frequency in either the operated or the contralateral ear. [2]Smyth et al, set criteria as worsening of bone conduction thresholds by 10 dB through the frequencies 500 to 4000 cps, or a 10% reduction in speech discrimination scores were considered significant. [19]Desai et al, state that the incidence of mild sensory hearing loss after middle ear surgery in immediate post-operative period is quite high and may go undetected and has tendency to recover spontaneously. The cause of hearing loss can be attributed to trauma due to noise and vibration produced by drills and suction irrigation. [20]Parkin et al, studied variables including diamond burrs, cutting burrs, two different air drills (Hall and Stryker), an electric drill (Emesco), and drilling with and without suction irrigation. The results show that the single factor contributing the highest noise level is suction irrigation. [21]Most studies confirmed that drill noise induced trauma can cause sensorineural hearing loss in different frequencies. The differences between the various studies are due to their different methods and limitations.
6. Conclusions
Tympanomastoid surgery and drilling during ear surgery can cause significant acoustic trauma and transient sensory hearing loss to the contralateral ear. The incidence of mild sensorineural hearing loss after middle ear surgery in the immediate postoperative period is quite high and may not be detected and can recover spontaneously. In majority of the cases, the cause of the hearing loss can be attributed to trauma because of noise and vibration produced by the drills. Drill generated noise cannot be lowered to a great extent. Otological surgeons must minimise drilling time during surgical management of chronic otitis media. Routine mastoidectomy in patients with dry ear should be discouraged unless necessary. Drill induced noise as a cause of hearing loss should be considered during mastoid surgery.
References
| [1] | Stromberg AK, Yin X, Olofsson A, Duan M. Evaluation of the usefulness of a silicone tube connected to a microphone in monitoring noise levels induced by drilling during mastoidectomy and cochleostomy. Acta Otolaryngol 2010 Oct; 130(10): 1163-68. |
| [2] | Man A, Winerman I. Does drill noise during mastoid surgery affect the contralateral ear? Am J Otol 1985 Jul; 6 (4): 334-35. |
| [3] | Tos M, Lau T, Plate S. Sensorineural hearing loss following chronic ear surgery. Ann Otol Rhinol Laryngol 1984; 93: 403-9. |
| [4] | Kylén P, Stjernvall JE, Arlinger S. Variables affecting the drillgenerated noise levels in ear surgery. Acta Otolaryngol 1977 Sep-Oct; 84(3-4):252-9. |
| [5] | Farzanegan G, Ghasemi M, Panahi F, Raza M, Alghasi M. Does drill-induced noise have an impact on sensorineural hearing during craniotomy procedure? Br J Neurosurg 2010 Feb; 24(1): 40-45. |
| [6] | Kylén P, Arlinger S. Drill-generated noise levels in ear surgery. Acta Otolaryngol 1976 Nov-Dec; 82(5-6): 402-09. |
| [7] | Pal S. Evaluation of the effect of Drilling on hearing in Ear Surgery. Bengal Journal of Otolaryngology and Head and Neck Surgery. 2014; 22(2). |
| [8] | Chandregowda BV, Mathew AS. Evaluation of Drill Generated Acoustic Trauma on the Non-Operated Ear Following Mastoid Surgery. International Journal of Scientific Research.2015; 4(6): 603-606. |
| [9] | Palva A, Sorri M. Can an Operation On a Deaf Ear Be Dangerous For Hearing? ActaOtolaryngol. 1979; 360:155-7. |
| [10] | Schick B, Schick BT, Kochannek S, Starlinger V, Iro H. Temporary sensory hearing deficits after ear surgery: a retrospective analysis. Laryngorhiootologie. 2007; 86(3): 200-5. |
| [11] | Biswas AC, Joarder AH, Siddiquee BH. Prevalence of CSOM among rural school going children. MMJ. 2005; 14(2): 152-5. |
| [12] | Holmquist J, Oleander R, Hallen O. Perioperative Drill Generated Noise Levels in Ear Surgery. ActaOtolaryngol. 1979; 87: 458-60. |
| [13] | Spencer MG. Suction tube noise and myringotomy. J Laryngol Otol. 1980; 94:383-6. |
| [14] | Domanech J, Carulla M, Traserra J. Sensorineural high-frequency hearing loss after drill-generated acoustic trauma in tympanoplasty. Arch Otorhinolaryngol. 1989; 246(5): 280-2. |
| [15] | Khurana AS, Verma SK, Singh S, Sohal BS. Incidence of sensorineural hearing loss following ear surgery. Indian J Otolaryngol Head Neck Surg. 1996; 48(2):130-4. |
| [16] | Paksoy M, Sanli A, Hardal U, Kibar S, Altin G, Atalay B. How drill generated acoustic trauma effects hearing functions in an ear surgery? Int J Head Neck Surg. 2013;3:127–133. |
| [17] | Alharbi F, Ahmed MR. Changes in inner ear structure and function after drill induced acoustic trauma. Am J Clin Exp Med. 2014; 2(5):90-6. |
| [18] | Migrov L, Wolf M. Influence of Drilling on the Distortion Product Otoacoustic Emissions in the Non-Operated Ear. J Otolaryngol Head Neck Surg. 2009; 71:153-6. |
| [19] | Smyth GDL. Sensoryneural Hearing Loss in Chronic Ear Surgery. Ann Otol Rhinol Laryngol. 1977; 86:1-6. |
| [20] | Desai AA, Aiyer RG, Pandya VK, Nair U. Postoperative sensorineural hearing loss after middle ear surgery. Indian J of Otolaryngol Head Neck Surg. 2004; 56: 240-242. |
| [21] | Parkin JL, Wood GS, Wood RD, Mccandless GA. Drill and suction-generated noise in mastoid surgery. Arch Otolaryngol. 1980; 106: 92-6. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML