-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2019; 8(1): 9-13
doi:10.5923/j.otolaryn.20190801.03

Bondy Procedure: Our Experience
Karthik Shamanna1, Ashwini Godse2, Madhuri Gudikote3
1Associate Professor, Department of Otorhinolaryngology, Bangalore Medical College & RI, Bangalore, India
2Senior Resident, Department of Otorhinolaryngology, Bangalore Medical College & RI, Bangalore, India
3Senior Resident, Department of Otorhinolaryngology, Bowring and Lady Curzon Medical College & RI, Bangalore, India
Correspondence to: Ashwini Godse, Senior Resident, Department of Otorhinolaryngology, Bangalore Medical College & RI, Bangalore, India.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Bondy procedure is modification of the radical mastoidectomy, where the mastoid and epitympanum are exteriorized with preservation of pars tensa and ossicular chain. A prospective study was conducted between January 2014 and January 2018 for a period of 4 years. 30 patients, who had cholesteatoma limited to the mastoid and epitympanum, lateral to the ossicles with intact pars tensa and ossicular chain underwent modified bondy procedure. Post operative follow up was done at 3 months, 6 months and 1 year. Mastoid cavity was inspected for residual disease, recurrence of cholesteatoma, discharge and meatal stenosis. Post operative hearing assessment was done at 3 months. During follow up, no recurrence and residual disease were observed and no significant changes were seen in hearing level and air bone gap. This prospective study concludes that bondy procedure is a very effective surgical procedure with good outcome and preservation of residual hearing.
Keywords: Cholesteatoma, Bondy procedure, Hearing preservation
Cite this paper: Karthik Shamanna, Ashwini Godse, Madhuri Gudikote, Bondy Procedure: Our Experience, Research in Otolaryngology, Vol. 8 No. 1, 2019, pp. 9-13. doi: 10.5923/j.otolaryn.20190801.03.
1. Introduction
- Chronic otitis media is a disease that is known worldwide and it is more common in developing countries. Chronic otitis media is classified as mucosal type and squamosal type. Cholesteatoma is found in squamosal type of chronic otitis media. Cholesteatoma is a benign disease histologically; however, its behavior may be aggressive locally, and its invasive properties are associated with significant morbidity and occasional mortality [1]. Earlier, treatment for cholesteatoma involved radical procedures, where the ossicular chain except footplate of stapes were removed and clearing the disease from the middle ear cleft and converting EAC, middle ear and mastoid into one large cavity and plugging the Eustachian tube orifice. This resulted in troublesome cavity problems and significant hearing loss postoperatively. Various authors have tried to overcome these problems by modifying the radical procedures with the aim of eradicating the disease, at the same time preserving the hearing mechanism and minimizing the cavity problems. For many years there has been an effort to develop surgical procedures, that eradicate cholesteatoma matrix with preservation of uninvolved structures and reconstruction of those structures and functions that have already been destroyed by the cholesteatoma. This procedure is commonly known as modified radical mastoidectomy (MRM). Bondy procedure is one such surgical procedure, which can be performed in cases of limited cholesteatoma involving the mastoid and epitympanum, lateral to the ossicles, with intact pars tensa. Previously, the principle of surgical procedures used to treat chronic middle-ear disease was to make the ear safe, with no attempt to preserve the pre-operative hearing level. In 1910, Bondy used this technique for epitympanic cholesteatoma in the presence of a defective pars flaccida, but with an intact pars tensa. The purpose of the Bondy procedure was to obtain a ‘safe ear’, while at the same time preserving the preoperative hearing level [2].
2. Materials and Methods
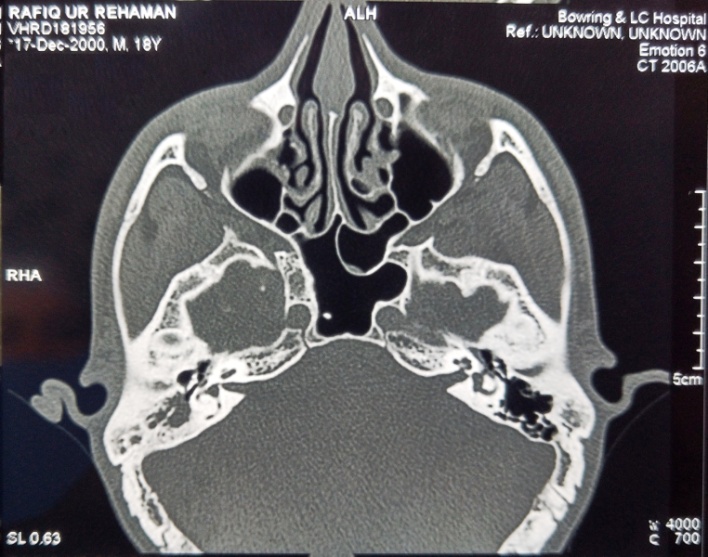
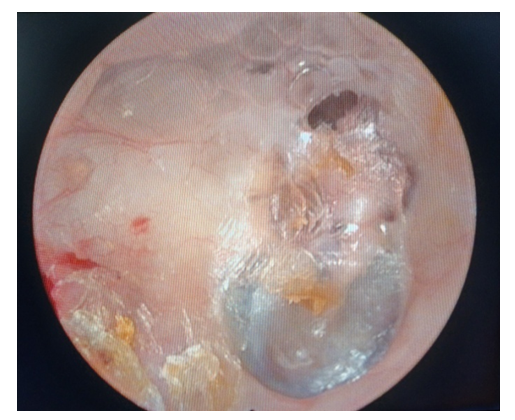
- This prospective study was done between Jan 2014 and Jan 2018 for a period of 4 years. During this period 30 patients of all age group were enrolled in the study. Detailed clinical examination, HRCT Temporal bone and PTA was done for all patients. Patients fulfilling the following criteria were included in this study.a. On otoscopic examination, there should be presence of cholesteatoma flakes in the attic region and erosion of scutum with intact pars tensa. b. In HRCT Temporal bone, the cholesteatoma sac arising from the epitympanum should extend into the mastoid antrum with intact ossicular chain. The mesotympanum and hypotympanum should be free of disease.c. Pure tone audiogram (PTA) showing fairly good hearing reserve.Patients who had cholesteatoma involving the mesotympanum and destruction of ossicular chain were excluded from the study.Patients who were included in the study underwent Bondy procedure under general anaesthesia. All surgeries were performed by the same surgeon.
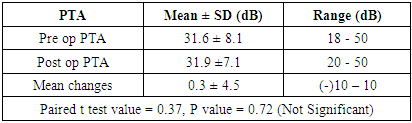
 | Figure 1. Preoperative Otoendoscopic view of right ear cholesteatoma involving the pars flassida (Arrow) with intact pars tensa |
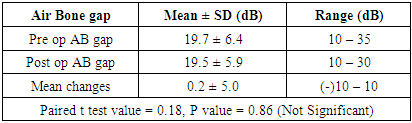
 | Figure 2. Preoperative HRCT of Temporal Bone (coronal view) showing scutum erosion with intact ossicular chain |
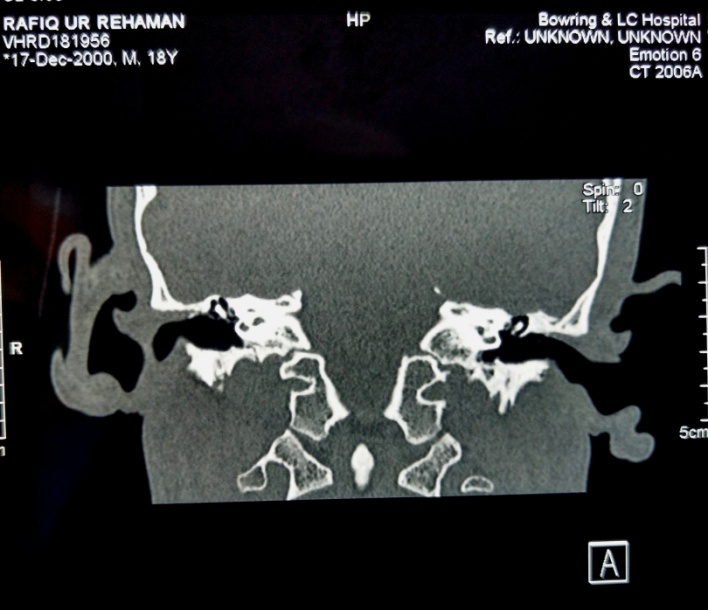
 | Figure 3. Preoperative HRCT Temporal Bone (axial view) showing cholesteatoma sac in the mastoid |
3. Results
- Results are expressed as Mean ± SD for continuous data and frequency as number and percentages. Unpaired t test was used for comparisons of means of two groups. Categorical data was analysed by chi-square test. P value of 0.05 or less was considered as statistical significance. SPSS (version 17) software was used for data analysis.Adequate follow up for 1 year was done for all the 30 patients who underwent modified bondy procedure. Out of 30 patients 20 (67%) patients were male and 10 (33%) patients were female. Age of the patients ranged from 7 years to 58 years.Intra operatively lateral semicircular canal erosion was seen in 5 (17%) patients and fallopian canal erosion was seen in 2 (7%) patients. At one year post operative follow up, there was no recurrence/ residual cholesteatoma, 8 (26%) patients had discharging mastoid cavity, which was managed conservatively, 3 (10%) patients had meatal stenosis, who underwent revision meatoplasty subsequently, 19 (64%) patients had healthy mastoid cavity (figure 4).
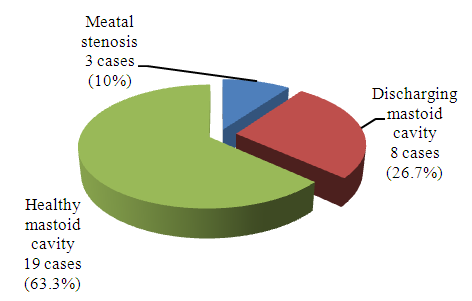 | Figure 4. Post operative outcome at 1 year follow up |
 | Figure 5. Post operative follow up at 1 year showing healthy mastoid cavity (Right) |
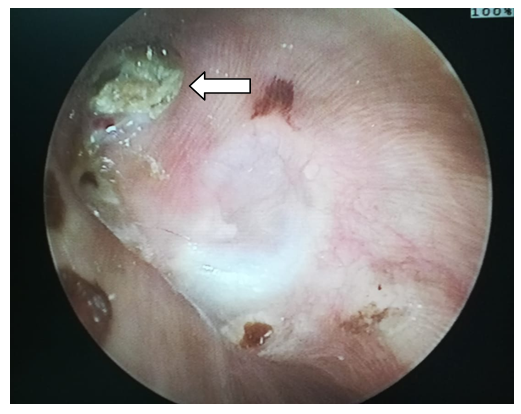
|
|
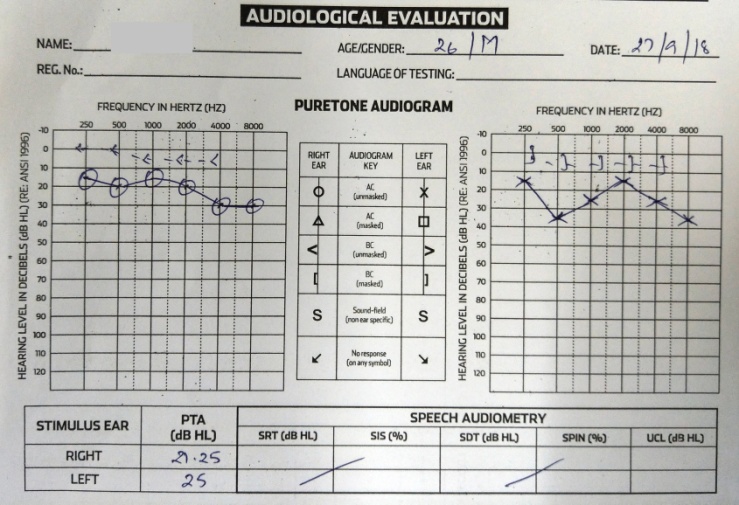 | Figure 6. Pre operative audiological evaluation (Right ear cholesteatoma |
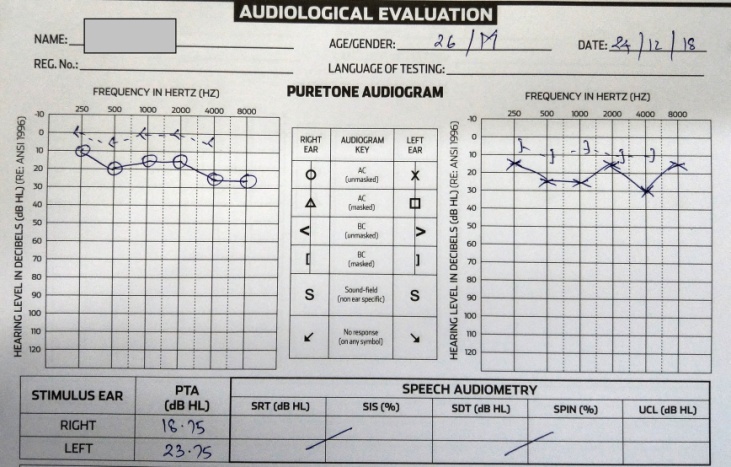 | Figure 7. Post operative audiological evaluation at 3 months following right ear Bondy procedure |
4. Discussion
- The primary goal of cholesteatoma surgery is to eradicate the disease completely and to restore hearing without any complications. The surgeries for chronic otitis media proposed by the American Society of Otolaryngology in 1964 included (and remain to the present day) radical mastoidectomy, modified radical mastoidectomy, mastoid obliteration, myringoplasty, tympanoplasty, and tympanoplasty with mastoidectomy. Radical mastoidectomy procedures have many disadvantages; the middle ear mucosa is often exposed, there by resulting in frequent bacterial and fungal infection and collection of debris leading to chronic otorrhea, which necessitate frequent aural toilet of the mastoid cavity. Most of these problems can be overcome by reconstructing the middle ear and tympanic membrane with temporalis fascia graft thus walling off the middle ear from the rest of mastoid cavity, there by facilitating the drainage of the middle ear through the patent eustachian tube. Radical mastoidectomy procedures are also accompanied by hearing loss which could be attributed to removal of the ossicles, shallow middle ear cavity with reduction of middle ear volume and air cushions. This can be overcome by preserving/ reconstructing the ossicular chain integrity and maintaining the depth of the middle ear cavity.Bondy procedure is a modified radical mastoidectomy surgery which is done in selected cases of cholesteatoma involving the mastoid and epitympanum, lateral to the ossicles with intact pars tensa and ossicular chain. The basic principle to conserve preoperative hearing level in Bondy procedure is by preserving ossicular chain and also the middle ear cavity, which has a major role in impedance matching and maintaining phase difference. To date, there have been only a few studies on Bondy procedure. The results are encouraging; they have reported good functional outcome and low recurrence in cases where pre-operative hearing is good and when the cholesteatoma is confined to the epitympanum, lateral to the ossicles. The present study was undertaken to discuss our experience with Bondy procedure in the management of cholesteatoma and its outcome.A study conducted on Chinese patients having chronic otitis media showed ossicular chain damage to occur in 54% of patients with cholesteatoma and in 11% of patients without cholesteatoma [3]. Incus is the most frequently affected ossicle [4-5]. The pathophysiological process of ossicular chain destruction is thought to be multifactorial and might result from a combination of ostietis, pressure necrosis, and enzyme-mediated lysis [6]. These patients are not ideal cases for the bondy procedure. Selection of cases for the bondy procedure is important; it should serve both the purposes such as safe ear and preservation of the preoperative hearing level. Study done by Stefano Berrettini, M.D et al on Modified Bondy radical mastoidectomy: long-term personal experience between September 1986 and July 1996, concluded that Bondy procedure should always be considered in cases of epitympanic cholesteatoma with normal or near normal hearing, even though the precise choice of surgical technique can only be made intra-operatively. They focused on the advantages of Bondy procedure over closed techniques, such as lower incidence of residual cholesteatoma, absence of recurrent cholesteatoma, ability to perform the procedure in one stage, fewer surgical revisions and preservation of preoperative hearing level. The strict criteria that must be observed in selecting candidates for this technique is; cholesteatoma confined to mastoid and epitympanum not involving medial attic with intact tympanic cavity, pars tensa and ossicular chain. [7]Eun Hwang, Hye Jin Lim, et al conducted a study on Bondy procedure, and its clinical usefulness on 15 patients who had cholesteatoma with relatively preserved middle ear. This study was a retrospective chart review of 15 patients who had undergone the modified Bondy operation between 1996 and 2010. They concluded that Modified Bondy operation is a good option to preserve hearing and prevent recurrence [8].Mario Sanna et.al evaluated the short term and long term outcomes of modified Bondy technique with reference to hearing level and refinements in surgical techniques to obtain a safe ear as well as functional results. 230 cases underwent the surgical procedure between January 1983 and December 2005. In their study there were no recurrent cholesteatoma, 7% of patients had residual cholesteatoma, 0.8% of patients had meatal stenosis, 3% of patients had discharging cavity, 1.3% patients had perforation, 1.3% of patients had retraction pockets, 5% patients had effusion. They concluded that modified bondy procedure is indicated in selected cases of localized epitympanic cholesteatoma with intact ossicular chain and pars tensa. [9]In a study conducted by Shaan M et al in 1995 on Bondy operation, concluded that this procedure is indicated in cases of epitympanic cholesteatoma with intact ossicular chain, normal pars tensa, and good hearing. The advantage of this technique is that it is a single stage surgery with preservation of preoperative hearing levels, which is not possible with any other procedure. [10]Maged b. Naguib MD et.al conducted a retrospective study on modified Bondy procedure on 37 patients between July 1986 and July 1992. They concluded that Bondy procedure achieves the objectives of cholesteatoma surgery that is; making the ear safe and also preserving hearing. The average postoperative air-bone gap improved by 5 to 15 dB in 11 cases (30%), remained unchanged in 16 cases (43%), and became worse in 10 cases (27%). [11] The outcome of our study parallels the results obtained by previous authors. Selection of cases plays an important role in the outcome of Bondy procedure. 30 patients who had cholesteatoma limited to the mastoid and epitympanum, lateral to the ossicles with intact pars tensa and ossicular chain were enrolled in the study. Preoperative high resolution computed tomography (HRCT) of temporal bone plays a vital role in assessment of ossicular chain integrity and extent of disease. All selected patients underwent modified Bondy procedure. At one year Post operative follow up, no residual/ recurrent cholesteatoma was noted, 64% of the patients had healthy mastoid cavity with good epithelialization. This could be attributed to good ventilation by wide Portman’s meatoplasty, well saucerized mastoid cavity and walling of the middle ear mucosa by keeping tympanic membrane intact. Soiling of the mastoid cavity by the middle ear secretions is prevented by intact tympanic membrane, thus reducing the incidence of otorrhea and recurrent infection. 26% of the patients had discharge from mastoid cavity due to incomplete epithelialization which was managed conservatively with regular aural toilet and diluted vinegar wash. 10% of the patients had meatal stenosis, they subsequently underwent revision meatoplasty. Pre operatively most of the patients had mild conductive hearing loss with mean air bone gap of 15 – 20 dB, this level remained unchanged post operatively as the ossicles and tympanic cavity was undisturbed during surgery.
5. Conclusions
- This study concludes that Modified Bondy procedure is a very effective surgical procedure with good outcome in the management of cholesteatoma limited to the mastoid and epitympanum, lateral to the ossicles with intact pars tensa and ossicular chain. The advantages of this procedure are it is a single stage surgical procedure, good preservation of hearing, low incidence of residual/recurrent cholesteatoma and minimal mastoid cavity problems.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML