-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2018; 7(3): 55-59
doi:10.5923/j.otolaryn.20180703.02

Comparative Study on Outcome of Septoplasty with or without Turbinoplasty Based on NOSE Score
Karthik Shamanna1, Ashwini Godse2
1Associate Professor, Department of Otorhinolaryngology, Bangalore Medical College & RI, Bangalore, India
2Senior Resident, Department of Otorhinolaryngology, Bangalore Medical College & RI, Bangalore, India
Correspondence to: Ashwini Godse, Senior Resident, Department of Otorhinolaryngology, Bangalore Medical College & RI, Bangalore, India.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

A prospective comparative study was conducted on 60 patients who had symptomatic deviated nasal septum along with compensatory contra-lateral hypertrophy of inferior turbinate. 30 patients underwent septoplasty alone and 30 patients underwent septoplasty combined with inferior turbinoplasty. Patients were randomly selected for the procedures. Pre-operative and Postoperative symptom scores were compared in both the study groups using Nasal Obstruction Symptom Evaluation Scale (NOSE). Postoperative improvement in symptom scores was seen in both the study groups following surgery, but when comparing the NOSE symptom score between the two groups, those undergoing septoplasty combined with inferior turbinoplasty had lower NOSE scores (with p< 0.05) which is statistically significant. This comparative study concludes that septoplasty combined with turbinoplasty provides better symptomatic relief of nasal obstruction than patients undergoing septoplasty alone.
Keywords: Deviated nasal septum, Inferior turbinate Hypertrophy, Septoplasty, Turbinoplasty, NOSE score
Cite this paper: Karthik Shamanna, Ashwini Godse, Comparative Study on Outcome of Septoplasty with or without Turbinoplasty Based on NOSE Score, Research in Otolaryngology, Vol. 7 No. 3, 2018, pp. 55-59. doi: 10.5923/j.otolaryn.20180703.02.
1. Introduction
- Nasal obstruction is a common presentation in Otorhinolaryngology practice. Deviated nasal septum (DNS) is the most common cause for nasal obstruction. Deviated nasal septum with compensatory hypertrophy of the inferior turbinate on the opposite side is often found. [1] Failure to reduce the size of the hypertrophied inferior turbinate at the time of septal surgery may result in persistent nasal obstruction. The most accepted theory for inferior turbinate hypertrophy is thought to be compensatory mechanism, which protects the more patent passage from excess airflow, drying and crust formation. [2, 3] An alternate theory being that unilateral growth of the inferior turbinate bone can be genetic or can be caused by trauma in early life. [4] This primary unilateral growth of the turbinate bone may exert pressure on the growing nasal septum during childhood and adolescence causing septum to deviate to the opposite side. Mucosal hypertrophy of the inferior turbinate is thought to be due to chronic inflammatory diseases of nose and paranasal sinuses such as allergic rhinitis, and rhinosinusitis which can be medically managed. Conversely osseous hypertrophy of the inferior turbinate secondary to septal deviations refractory to medical management needs to be surgically corrected along with septoplasty. [5, 6]Various methods are available for assessing the nasal obstruction in clinical practice; they could be either subjective or objective. Objective tests being rhinomanometry and rhinometry, however it is difficult to carry out these procedures in daily practice hence, subjective evaluation was introduced which is a simple method to assess the nasal obstruction. NOSE score is a subjective method for assessment of nasal obstruction based on questionnaires which gives better assessment of patient’s symptom severity and quality of life. [7]Although turbinoplasty with septoplasty is a relatively common surgical procedure, studies regarding comparison between septoplasty alone and septoplasty combined with inferior turbinoplasty are limited. Hence this study was undertaken to evaluate the postoperative subjective improvement of nasal obstruction in patients undergoing septoplasty with or without turbinoplasty using NOSE (Nasal Obstruction Symptom Evaluation Scale) Score.
2. Materials and Methods
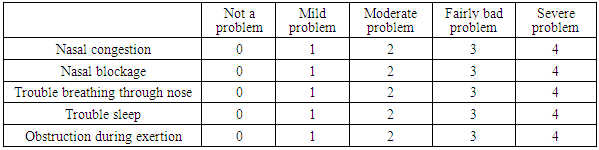
- This prospective comparative study was done between January 2015 and December 2017. During this period 60 patients of age 17 years and above, who had symptomatic nasal septal deviation along with contralateral inferior turbinate hypertrophy, were enrolled in this study. Patients whose age was less than 17 years, those who had undergone previous surgeries like septoplasty or submucous resection, and patient who had acute and chronic rhino sinusitis, perforated nasal septum, granulomatous condition of nose and sinuses, craniofacial malformation and pregnant woman were excluded from the study. Detailed history and clinical examination was done. Nasal Obstruction Symptom Evaluation (NOSE) scale was used preoperatively to know the severity of their symptom. In this assessment scale, a questionnaire consisting of 5 symptoms was used. The patients were informed to grade the severity of symptoms, and each symptom was given points ranging from 0 to 4 depending on the severity. 0 point being minimum and 4 points being maximum. (Table 1) Total points = Q1+Q2+Q3+Q4+Q5. This is divided by 20 & multiplied by 100, to obtain a NOSE score which is expressed as percentage.Total NOSE Score = {(Q1+Q2+Q3+Q4+Q5) / 20 * 100} %.Higher percentage score indicates more problematic nasal obstruction.
|
|
 | Figure 1. Preoperative CT scan of nose and paranasal sinuses showing DNS to right with left inferior turbinate hypertrophy |
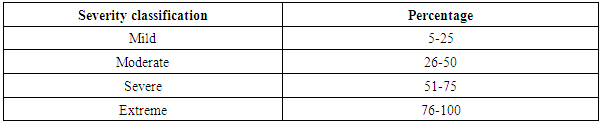
 | Figure 2. Preoperative diagnostic nasal endoscopy showing left inferior turbinate hypertrophy |
3. Results
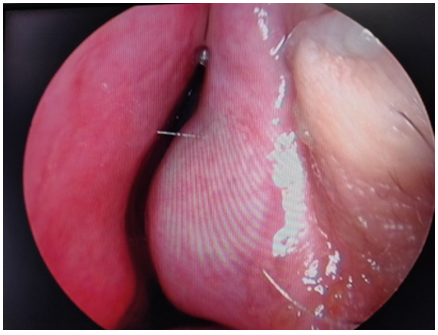
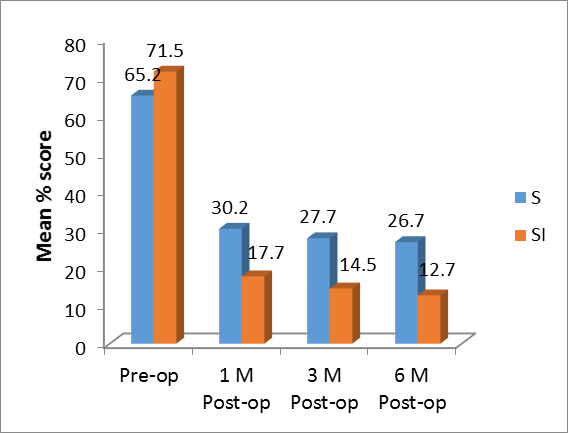
- Results are expressed as Mean ± SD for continuous data and frequency as number and percentages. Unpaired t test was used for intergroup comparisons of means of two groups. Categorical data was analysed by chi-square test. A P value of 0.05 or less was considered as statistical significance. SPSS (version 17) software was used for data analysis.Preoperative analyses of NOSE score showed a high value in all the patients in both the study groups and their severity classification ranged from moderate to extreme. At 6 months postoperative follow up, NOSE score in both the study groups showed significant reduction (P value <0.05) and their severity classification ranged between mild to moderate.But when NOSE Score was compared between the two groups, patients who underwent septoplasty combined with turbinoplasty had significantly lower NOSE score than the study group who underwent septoplasty alone (Figure 3).
 | Figure 3. Inter group comparison of changes in NOSE scores preperatively and postoperatively. (S – Septoplasty alone, SI – Septoplasty combined with turbinoplasty) |
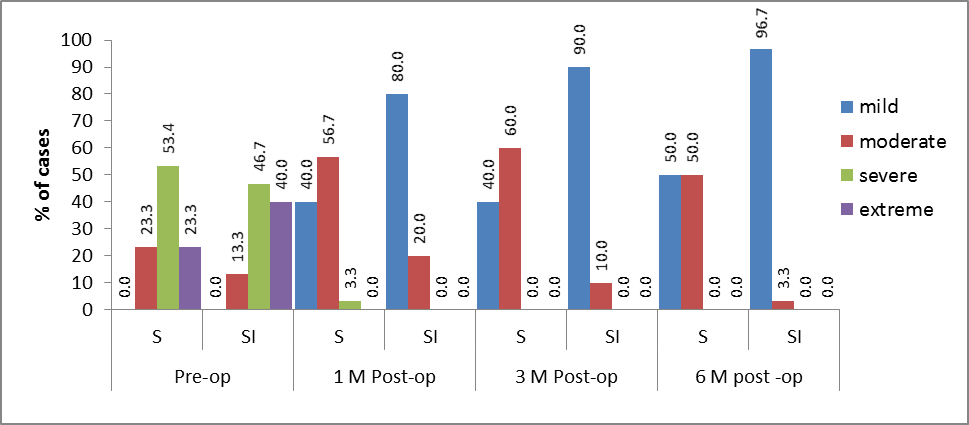 | Figure 4. Distribution of cases with corresponding severity in study groups |
4. Discussion
- This present study was undertaken with the objective of comparing the outcome of septoplasty with or without turbinoplasty in relieving the nasal obstruction based on NOSE Score. Our study showed that patients who underwent septoplasty combined with the turbinoplasty (group B) had lower NOSE score compared to patients who underwent septoplasty alone (group A). Quality of life in these patients improved as a result of improved breathing and better sleep. Poiseuille’s law states that air flow through a tube is proportional to the fourth power of the radius or to the square of the cross sectional area of the tube. [8] This means that slight variation in the size of soft tissue and/or bone of the inferior turbinate can have a large effect on nasal airflow. So reducing the inferior turbinate hypertrophy at the time of septal surgery improves the nasal passage and gives better relief of nasal obstruction post operatively. While performing the surgery on inferior turbinate care should be taken not to remove the inferior turbinate excessively, which hampers the physiological functions of the nose leading to excessive drying, crust formation and on long term probably may lead to atrophic changes. [9] Failure to reduce the size of the turbinate at the time of septal surgery may result in persistent nasal obstruction. There are two schools of thought regarding the role of inferior turbinoplasty, one group of authors postulated that once septoplasty is done, compensatory hypertrophy of the inferior turbinate regresses on its own, while the other group of authors argued that these hypertrophic changes are not spontaneously reversible and should be corrected in conjunction with septoplasty. The work of Kim et al. was based on studying the effects of septoplasty on the thicknesses and cross-sectional areas of mucosa and conchal bone using computed tomography of nose and paranasal sinus preoperatively and at least one year post operatively. They found that the thickening of the mucosa of the inferior turbinate (especially the medial mucosa) on the concave aspect and the thinning of mucosa on the convex aspect, reverses after septoplasty. However further follow up was required to see if there are any bony changes in the longer term. [10]A randomized clinical study was done in Dokuz Eylul University Turkey in 2010-11 by N. Devseren et al on 42 patients with septum deviation and compensatory contralateral turbinate hypertrophy. Patients were divided into two groups. Group A underwent submucous resection of contralateral hypertrophied turbinate together with septoplasty. Group B underwent only septoplasty. The post operative resolution of subjective symptoms was better in group A when compared to group B. [11]In a Study conducted by Jun BCJ, Kim SW, Cho JH, Park YJ, Yoon HR at St.Mary’s hospital, South Korea, computed tomography of nose and paranasal sinuses of 20 patients with deviated nasal septum and inferior turbinate hypertrophy was done, the volume of the inferior turbinate was measured from the three-dimensional reconstruction of the scans. It was concluded that, the inferior turbinate on the concave side had a significantly greater volume and hence septoplasty and concomitant inferior turbinate surgery to manipulate conchal bone and soft tissues are necessary for treatment of those patients with unilateral nasal septal deviation and compensatory hypertrophy of the contralateral inferior turbinate. [12]Gilead Berger et al, studied the histopathological changes in hypertrophied inferior turbinate in patients having symptomatic deviated nasal septum who underwent surgery for nasal obstruction and compared it with cadaveric normal inferior turbinate specimens. It was found that, the hypertrophied inferior turbinate bone had a two fold increase in thickness. This study supported the decision to excise the hypertrophied inferior turbinate bone at the time of septoplasty because of significant bony expansion & relative minor role of mucosal hypertrophy. [4]Study by Wight, Jones and Clegg showed that anterior trimming of the inferior turbinate, whilst being an objective success in decreasing nasal resistance, frequently failed to produce a significant fall in subjective nasal obstruction postoperatively. [13]Leandro Castro Velasco et al study was focused on post operative evaluation of relief from nasal symptoms, including nasal obstruction. It was found that septoplasty, with or without turbinectomy, resulted in improvement of all symptoms. They found no additional significant advantages in patients undergoing septoplasty combined with turbinectomy. Removing the nasal splint and avoiding contact between the mucosa of the nasal septum and the turbinates were the main improvement factors in the first evaluation. [14]Berger G, Gass S, Ophir Dhat study focused on reduction of the medial and inferior mucosal layers of the hypertrophied inferior turbinate. In their study, the medial mucosa of the inferior turbinate had the greatest thickness causing nasal airway obstruction and recommended its reduction. They feel the lateral mucosal layer should be left intact as it does not encroach on the airway and has an important role in humidifying the inspired air and maintaining mucociliary clearance. [15]
5. Conclusions
- This comparative study concludes that in patients with symptomatic nasal septal deviation with hypertrophy of the contralateral inferior turbinate, combining septoplasty with turbinoplasty provides better symptomatic relief of nasal obstruction than patients undergoing septoplasty alone. Quality of life was better in those patients who underwent septoplasty combined with inferior turbinoplasty. Post operative follow up NOSE score was significantly lower in patients who underwent inferior turbinoplasty at the time of septoplasty.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML