-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2018; 7(2): 28-35
doi:10.5923/j.otolaryn.20180702.02

The Impact of Local Anesthesia on Tympanostomy Tube Insertion for the Treatment of Chronic Otitis Media with Middle Ear Effusion in Adult Age Patients: A Prospective, Randomised, Controlled Study
Randa A. Abdallah1, Tamim Al Ali2, Abla Saab3
1Lecturer of Otolaryngology and Head and Neck Surgery, AL Azhar University Hospitals, Cairo, Egypt
2Head of Audiology and Speech Department at Zain and Salim Al Ali Hospitals, Kuwait
3Lecturer of Anesthesia and Intensive Care Unit, Ain Shams University Hospitals, Cairo, Egypt
Correspondence to: Randa A. Abdallah, Lecturer of Otolaryngology and Head and Neck Surgery, AL Azhar University Hospitals, Cairo, Egypt.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

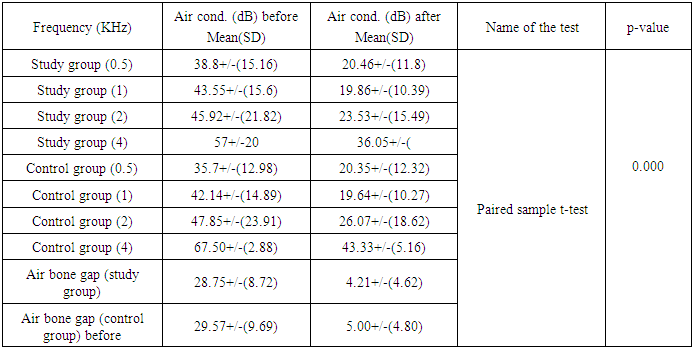
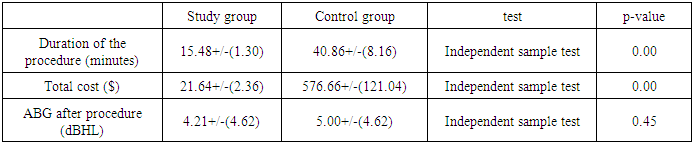
Objective: To conduct the important role of local anaesthesia in myringotomy and ventilation tube insertion for the treatment of otitis media with effusion (OME) in adult patients and improving hearing outcomes and limiting the use of general anaesthesia for this procedure. Patients and Methods: Ninety one adult patients aged between 20 and 69 years diagnosed with persistent chronic non supurtive otitis media with effusion lasting at least 1 month. The patients were randomly arranged either as a treatment group (71) or control group (15). Results: one week post operatively, the mean improvement in air conduction across 0.5, 1, 2, 4 KH were frequencies (20.46, 19.86, 23.53 and 36.05) post operatively comparing the pre operatively values (38.8, 43.55, 45.92 and 57 dB) and air bone gap (4.2) post operatively while (28.75) pre operatively for the study group patients with significant (p-value<0.001). While the air conduction values for the control group patients at the same frequencies were (20.35, 19.64, 26.07 and 43.33Db) post operatively and (35.7, 42.14, 47.85 and 67.50 Db) and Air bone gap (5.00) post operatively and (29.57) pre operatively with significant p-value<0.001). The mean procedure duration for study group was (15.48 minute) and (40.86 minutes) for the control group, also the procedure duration time cost was (21.64$) for study group compared with the control group (576.66$) for control group with significant p-value <0.001 on the same time of insignificant difference p-value=0.45 regarding to ABG mean (4.21) in the study group and (5.00) in the control group. Conclusion: our study have conducted that the use of topical anaesthesia for the purpose of myringotomy with ventilation tube insertion in the outpatient clinic is safe, fast, effective with less duration and less procedure time cost compared with the use of general anaesthesia inside the operation theatre for the same purpose.
Keywords: Topical, Randomised, Air conduction, Air bone gap, Duration and cost
Cite this paper: Randa A. Abdallah, Tamim Al Ali, Abla Saab, The Impact of Local Anesthesia on Tympanostomy Tube Insertion for the Treatment of Chronic Otitis Media with Middle Ear Effusion in Adult Age Patients: A Prospective, Randomised, Controlled Study, Research in Otolaryngology, Vol. 7 No. 2, 2018, pp. 28-35. doi: 10.5923/j.otolaryn.20180702.02.
Article Outline
1. Introduction
- Middle ear effusion (MEE) is a very common disease in children and adult, it may reach about 20% incidence in the young school-aged children [1], but it is less common in adult age group .The pathogenesis of middle ear effusion is complex with several factors thought to play a role in its aetiology, however the most common cause is the poor ability of the Eustachian tube to equalise negative pressure in the middle ear [2]. Although, it may be not clear whether the impairment of the Eustachian tube function is a cause or a result of the middle ear effusion. Several previous studies [2] proved that adult patients with poor mastoid pneumatisation were considered to be a high risk group for the development of secretory otitis media (SOM) which was studied with previously published findings regarding the correlation between the degree of mastoid pneumatisation and the risk of development of chronic otitis media and SOM.Negative pressure was considered as a general feature of the various forms of otitis media, and also its buffering action could not be properly regulated in absence of adequate mastoid pneumatisation. The actual cause of such negative pressure is not completely clear, but it could be result from an inflammatory condition such as SOM which triggered a process of middle deficiency or increased diffusion [3]. Regardless, the idea of improving the Eustachian tube function in a noninvasive manner via Valsalva or Politzer manoeuvres offers another potential treatment modality for OME. It is important to note that the Valsalva and Politzer manoeuvres have a small but key difference; the Valsalva manoeuvre is performed by an uncontrolled forceful attempt at expiration against a closed airway, whereas the Politzer manoeuvre is a controlled delivery of air into the nostril against a closed airway. The standardised controlled delivery of air provided by the Politzer manoeuvre makes it much more reliable and reproducible, and a preferred method for non-surgical intervention. The Otovent balloon is an autoinflation Valsalva device, and a review showed no significant changes in pure tone audiometry [4].The financial impact of otitis media on health care is enormous. Otitis media–related Medicaid expenditures in the United States were $555 million for the 12.5 million covered children younger than 14 years in 1992. [5] Concurrently, national expenditures for treatment and disability associated with otitis media exceeded $4 billion. Direct costs associated with childhood otitis media include office visits, diagnostic tests, medical treatment, and surgical procedures. Indirect costs for AOM are substantial, estimated at 61% to 83% of the total expense, (and include child school absence, caregiver absence from work or school, and cancelled family activities because of child illness [6]. With nearly 670,000 tympanostomy tube insertions annually in children in the United States [7] an average cost of $2700 per procedure, the contribution to health care costs is approximately $1.8 billion. This does not include additional costs related to follow-up care (which continues until after the tube extrudes), treatment of otorrhea, and management of any other sequele or complications. A cost analysis based on chart review from one managed care organization showed that tympanostomy tube insertion is cost-effective for otitis media in children, but no large-scale studies or formal cost-effectiveness analyses are available to assess the generalbility of this claim [6].Study design:A comparative randomised controlled trial was carried out in our hospital between December 2017 and April 2018.Setting: ENT Department, Taiba Hospital Kuwait.Inclusion and exclusion criteria:Patients aged from 19 to 76 years with hearing loss from persistent otitis media with middle ear effusion over a one-month period and an average air conduction of 25 dBHL or worse across 0.5, 1.0, 2.0 and 4 kHz were considered eligible for the trial. Any patient with nasopharyngeal mass, chronic sinusitis was excluded. All four frequencies were tested (if the patient was compliant) by our blinded audiologists (T.A) 4 weeks after treatment and recorded as before tympanostomy audiograms and repeated by the same audiologist one week post procedure.
2. Materials and Methods
- Patients attended our ENT department Taiba hospital Kuwait, including 76 consecutive patients (39 male and 37 female) whose age was 20 to 75 years (mean of 50.92 ± 14.83years) for the study group and 15 consecutive patients (7 male and 8 female) whose age was 21 to 75 years (mean of 55.92 ± 14.01years) and planned to undergo myringotomy with grommet tube insertion for treatment of otiits media with middle ear effusion (OME). They were complaining of symptoms suspected OME including decrease hearing, ear blockage, tinnitus, ringing of ear, ear ache and dizziness. All patient were gone a full history, ENT examination, pure tone audiogram, Tympanometry and CT nasopharynx with nose and para-nasal sinuses were done for all patients to exclude any nasopharyngeal masses. After a 1-month period of failed medical treatment and follow up, patients with persistent OME were advised for Myringotomy with ventilation tube insertion by the same otolaryngologist (R.A.) either under local or general anaesthesia. An informed consent for the procedure was taken from all patients as our Ministry of health roles in all Kuwait hospitals. At the time of entry into the ENT clinic, all patients were randomly allocated to a study group containing 76 patients and a control group involving 15 patients after failure of conservative medical treatment and both of otologist and audiologist were blinded about the arrangement of the patients from which group before the procedure and in the follow up visit. For each patient in the study group, the procedure started by application of emla cream (5%) {(one gram contains: Lidocaine 25mg, Prilocaine 25mg, Carbomer, Polyxyethelene hydrate costor oil, Soduim hydroxid and water)} inside the external auditory canal and the drum using an insulin syringe connected to cannula applied to its tip after removal of the needle we put about one ml EMLA cream in side this syringe to make the cream reach the drum and the deep part of the external auditory canal more easy. Then we inform the patient to wait for ten minutes to start the procedure and then we would call the patient again and do suction for all EMLA cream then by the use of microscope, Myringotomy knife we did an incision in the antro-inferior portion of the tympanic membrane then we did suction by the use of a small suction tip cannula and then we inserted the Grommet ventilation tube in the incised drum and fixed it by the use of small crocodile and needle. After that we used 0 degree telescope and camera we showed the tube in place to the patient to be aware about what was the procedure and what was the result to be sure about his satisfaction. For the control group patients who were randomly booked for Myringotomy and Grommet tube insertion under general anaesthesia.EMLA is composed of mixture of two well known local aesthetics agent prilocaine and lidocaine. It is considered as an oil-in-water emulsion mixture. The oil phase composed of an eutectic mixture of the lidocaine and prilocaine. These constituents melt at room temperature so it is present in liquid form in the room temperature. This effect is best produced when the drugs were mixed in 1:1 ratio. In EMLA, the concentration of lidocaine and prilocaine achieved in the oil droplet is 80% though the overall concentration of both the active drugs is kept as low as 5% in the mixture. This is secondary to the emulsifiers present in the mixture. This reduction in concentration is responsible for decreased systemic toxicity (8).Anaesthetic techniques:For the patients of control group the same anaesthesia doctor (A.S) is the one giving general anaesthesia for all patient.Premedication injection of midazolam 0.03 mg/kg intravenous for all patients. For all patients Attachement of basic monitoring (SpO2, ECG and NIBP) and Pre-oxygenation with 100% oxygen wee done. All the patients received injection fentanyl 1.mcg/kg intravenously and bolus dose of intravenous induction of propofol 0.75 mg/kg Injection. Maintenance of Anesthesia Was done with Oxygen/Nitrous Oxide sevoflorane face mask spontaneous ventilation. All the patients were monitored, End tidal co2, continuous pulse oximetry and ECG monitoring, intermittent recordings of blood pressure and respiratory (respiratory rate, SpO2), parameters were noted. Undesirable events like desaturation, hypoventilation (respiratory rate <8), inappropriate movements, were monitored. Patients were placed supine on the operating table with the head turned opposite to the ear to be operated. Appropriate head positioning is critical to maintain an open airway necessitating good communication with the surgeon allthrough the procedure. Emergence from Anesthesia with 100 o2, Patients then transferred to the recovery room for continuity care monitoring. Postoperative pain was managed by IM / IV Pethidine or IV paracetamol. A digital stopwatch was used by the circulating nurse to record the duration of procedure starting from shifting the patient to the theatre till he was shifted outside the recovery room. The procedure itself is very quick and often takes less than 5 minutes to complete. A small hole is made in the tympanic membrane, and any fluid in the middle ear was sucked by the use of a small suction device. The tube is then carefully placed into the newly created hole. Then of all procedure including starting from shifting the patient to the operating theatre till shifting the patient from the recovery room the average time was calculated and the time cost for operation room also was calculated to compare the cost of average cost for both study and control groups.Ethical considerations:Ethical approval was obtained from Taiba hospital committee and an informed consent was taken from each patient.
3. Statistical Analysis
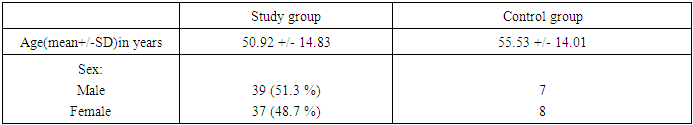
- Statistical method:The data were analyzed using SPSS program (version 22) SPSS_ software SPSS Inc. PASW Statistics for Windows, Chicago, Illinois, USA. The threshold of air conduction frequencies and air bone gap were before and after the tympanostomy with Grommets tube insertion were compared using parametric paired sample t-test. It was considered significant at p-value <0.05. Non paired t-test was used to compare the mean air conduction threshold for both study and control groups after the procedure. Mean and standard deviation (SD) were estimated to describe the central tendency and the dispersion of parametric data and Student’s t-test was used to compare between the two means. The level of significance was taken as p-value ≤ 0.05 and the results are presented in tables.Result:Ninety one patients satisfied the inclusion criteria and were recruited prospectively. Seventy six of them were randomly allocated as a study group, and the remaining fifteen were included in the control group. The pure tone audiometry results for all study and control groups were available. Baseline data for these patients are shown in Table 1. Mean age in treatment groups is (50.92) years (range 20-75) (39) male and (37) female and (55.53) years (range 21-75) (7) male and (8) female for the control group showing no statistical difference for both groups. All of them were complaining of persistent otitis media with middle ear effusion over one month. Random grouping to do tympanostomy with grommet tube under local anaesthesia (study group) and tympanostomy with grommet tube insertion under general anaesthesia (control group). Follow-up by doing pure tone audiometry 1 week after the procedure for all patients showing no significant difference in demographic data for patients in both groups.
|
|
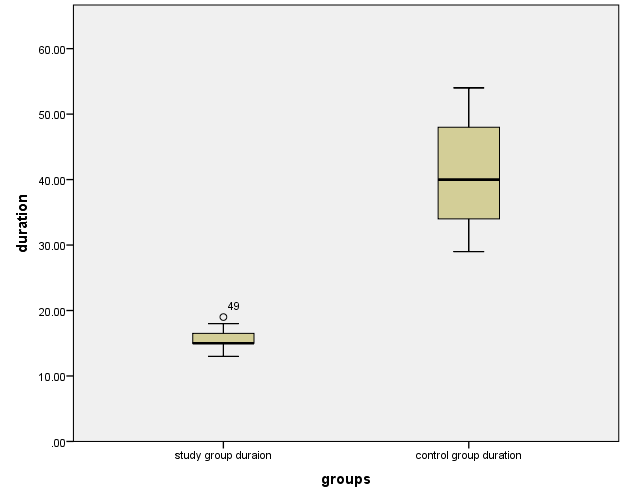 | Figure 1. Pox plots showing a comparison between the duration of both groups |
|
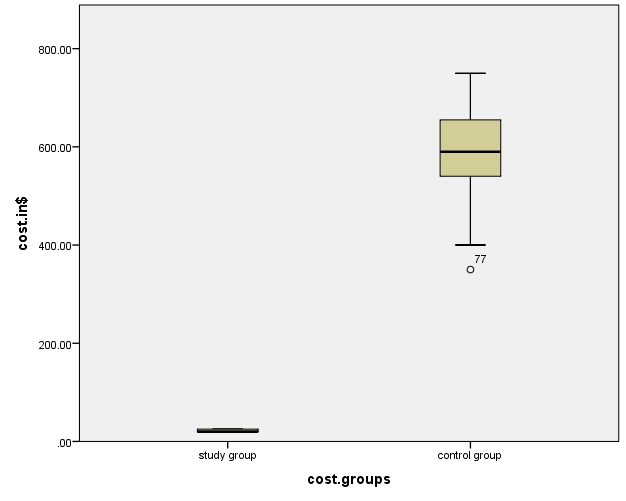 | Figure 2. Pox plots showing a comparison between the duration cost of both groups |
4. Discussion
- Our study found that all patient for the study group and the control group showed significant improvement in all symptoms including improvement of hearing level, tinnitus, ear blockage sensation and no patient complained of any adverse effect after EMLA cream. The strengths of the study:The randomised blinded controlled trial design of this study reduced any potential bias. Also Sample size was calculated as 91 SOM adult patients randomly divided into two groups one group was (76 patients) study group and the other was (15 patients) control group (as shown in fig.3), in each, the otologist, audiologist and anaesthesiologist were un aware that the patient belonged to which group from the start give the study a power of 80% at the 5% level of significance.
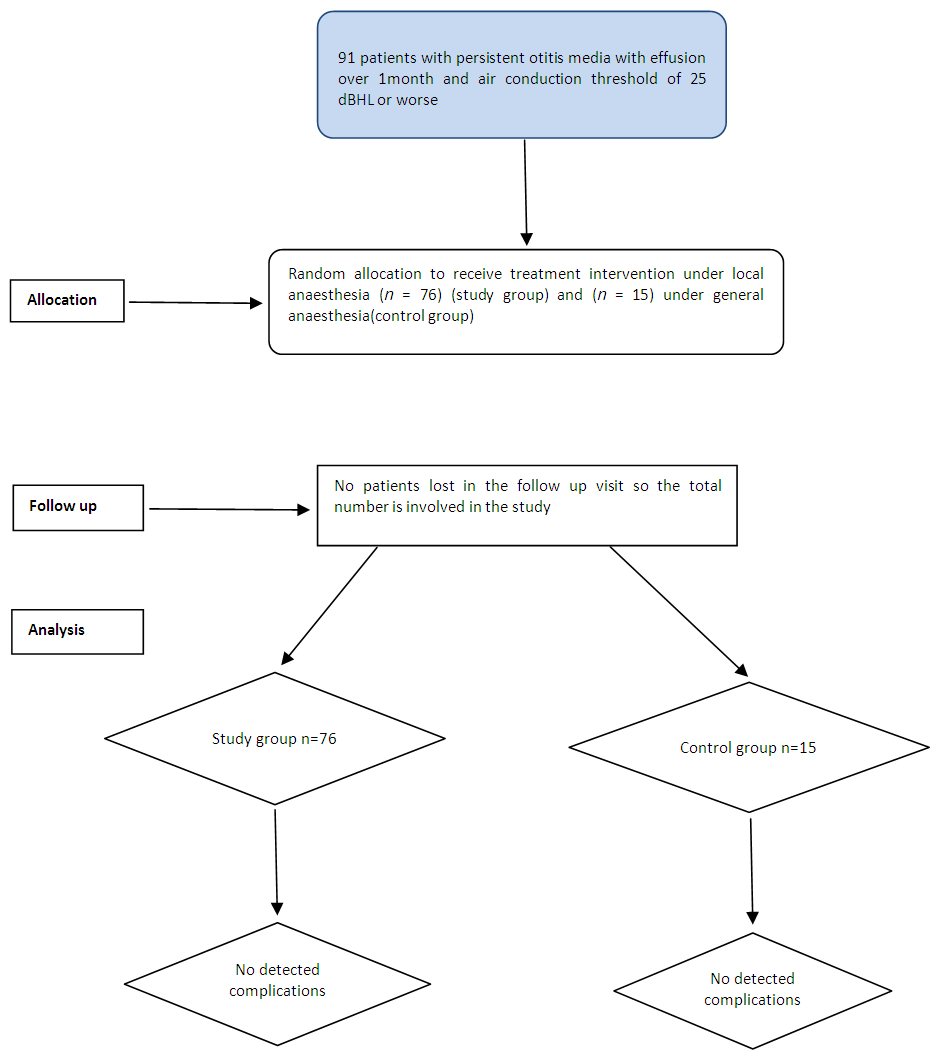 | Figure 3. CONSORT flow diagram |
5. Conclusions
- We have conducted the use of topical anaesthesia with EMLA cream for the purpose of myringotomy with ventilation tube insertion in the outpatient clinic is safe, fast, effective with less duration and less procedure time cost compared with the use of general anaesthesia inside the operation theatre for the same purpose and also giving the same result if using the general anaesthesia also it is very useful for intra tympanic injection of corticosteroid in case of sudden sensory neural hearing loss or intra tympanic injection of oto-toxic material in case of tinnitus.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML