-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2018; 7(2): 21-27
doi:10.5923/j.otolaryn.20180702.01

Full Thickness versus Partial Thickness Tragal Cartilage Graft Compared with Temporalis Muscle Fascia Graft in Myringoplasty
Sayed M. S. Kadah1, Fatma M. Abd-Elgaber2, Ayat Abu-Elnasr3, Walaa Abu-Mossalem4
1Professor of Otorhinolaryngology Department, ENT, Faculty of Medicine, Al-Azhar University, Cairo, Eygypt
2Associative Professor Otorhinolaryngology Department,E NT, Faculty of Medicine, AL-Azhar University, Cairo, Eygypt
3Assistant Professor Otorhinolaryngology Department, ENT, Faculty of Medicine, AL-Azhar University, Cairo, Eygypt
4Resident of Otorhinolaryngology Department, ENT, Faculty of Medicine, AL-Azhar University, Cairo, Eygypt
Correspondence to: Ayat Abu-Elnasr, Assistant Professor Otorhinolaryngology Department, ENT, Faculty of Medicine, AL-Azhar University, Cairo, Eygypt.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

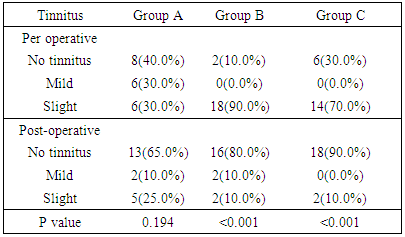
Background: tympanoplasty aims to create an intact tympanic membrane and to improve hearing. Temporalis fascia is commonly used but may undergo atrophy and re-perforation. Cartilage is a good graft due to its stability and resistance to negative pressure but may interfere with sound transmission. Thinning of cartilage counteracts the disadvantage effect of the full thickness graft on sound transmission. We aimed to present our experience in comparing full thickness, partial thickness tragal cartilage and temporalis fascia as grafting materials in myringoplasty type 1 concentrating on graft uptake, hearing gain and tinnitus improvement. Patients & Methods: Sixty patients presented with chronic supportive otitis media with perforation of tubo-tympanic type were subjected to prospective study. (Group A) and (Group B) underwent full thickness and partial thickness tragal cartilage tympanoplasty respectively while (Group C) underwent temporalis fascia. The three groups were evaluated after 3 months from surgery as regarding to graft take, hearing improvement and tinnitus. Results: There were statistically significant increase in post-operative hearing gain in all groups. P value were <0.001. There were statistically insignificant difference between the 3 groups as regarding to the successful graft take up (P value = 0.791). THI questionnaire showed statistically insignificant difference (p= 0.194) between pre and postoperative results in group A while in group B and C showed statistically significant difference (P <0.001). Conclusion: Partial thickness cartilage counteracts the disadvantage effect of temporalis fascia and full thickness cartilage as graft material.
Keywords: Tympanoplasty, Tragal cartilage, Temporalis fascia, Hearing, THI
Cite this paper: Sayed M. S. Kadah, Fatma M. Abd-Elgaber, Ayat Abu-Elnasr, Walaa Abu-Mossalem, Full Thickness versus Partial Thickness Tragal Cartilage Graft Compared with Temporalis Muscle Fascia Graft in Myringoplasty, Research in Otolaryngology, Vol. 7 No. 2, 2018, pp. 21-27. doi: 10.5923/j.otolaryn.20180702.01.
Article Outline
1. Introduction
- Chronic Suppurative Otitis Media (CSOM) is chronic inflammation characterized by a persistent otorrhea; usually with perforated tympanic membrane [1]. Tympanic membrane (TM) perforation is one of common consequence of otitis media, trauma, and complicated ear surgery [2]. Many materials are used for TM perforations closure as temporalis fascia, perichondrium, skin, vein, Dura, and cartilage [3]. The ideal grafting material should characterized by low rejection rate, similar to that of tympanic membrane in conductive properties, sufficient size, good tensile strength and easy availability [4]. Underlay grafting of temporalis fascia is the most widely used technique for the repair of tympanic membrane perforations [5].The fascia and perichondrium are flexible and has more or less the same thickness as a tympanic membrane. However, they may undergo atrophy and result in graft perforation [4].Tragal cartilage is also similar nature of the tympanic membrane and composed of collagen type II fibroelastic cartilage, temporalis muscle fascia consists primarily of collagen type I. Collagen type II has higher tensile strength than other types [4]. The tragus cartilage is ideal because it is thin, flat, and in sufficient quantities to permit reconstruction of the entire TM. [6]. However; with full thickness graft maximum hearing improvement may be sacrificed due to interfering with the sound transmission [7].Thinning cartilage plates are used for the reconstruction of tympanic membrane defects, and to protect total or partial the disadvantage effect of the full thickness graft interfering with the sound transmission [7]. However; good hearing results have shown by various authors, regardless of the thickness of the grafts [8].
2. Patient and Method
- Randomized prospective study conducted at Otorhinolaryngology Department of Al-Zahraa Hospital, Al-Azhar University, Egypt, between September 2016 and September 2017. Sixty patients with chronic otitis media with perforation (safe type) were included in the study. Forty-one were females and 19 were males. The age ranged from 12 to 47 years. The study protocol was approved by the hospital's ethics board.Inclusion criteria include unilateral or bilateral CSOM with central perforation, dry ear with intact ossicular chain, patients of either sex, with conductive hearing loss proved by audiometry. A written informed pre-operatively consents were taken from all patients after explaining the procedure. Exclusion criteria included unsafe CSOM with perforation (cholesteatoma), active ear discharge, unhealthy middle ear mucosa, cases requiring ossicular reconstruction, cases with sensorineural or mixed hearing loss, congenital hearing disorder, previous history of ear surgery, patients who refuse to participate in the study, patients with any systemic diseases, pregnancy or contraindicated for surgery.Patients were divided by systemic random sampling method into three groups each including 20 patients. All patients underwent an underlay myringoplasty (type I), using the tragal cartilage and temporalis fascia as the grafting material.• Group A patients underwent a full thickness tragal cartilage graft.• Group B patients underwent a partial thickness tragal cartilage graft.• Group C patients underwent temporalis fascia graft.All patients were subjected to2.1. Preoperative assessment included taking history from the patient or his/her parents, clinical examination of ENT, Head and Neck, Preoperative audiometry and tympanometry, preoperative tinnitus handicap inventory questionnaire (THI) and all routine investigation. The audiometry was done, comprising the following frequencies: 250, 500, 1000, 2000, 3000, 4000, 6000 and 8000 Hz in all the patients with controlled otorrhea. For calculation of average of hearing loss (air conduction threshold) the following frequencies were selected: 500, 1000, 2000 and 4000 Hz [9].The patients responded to a specific tinnitus questionnaire (THI) [10] in which 25-item questionnaire that is scored on a three-point scale (no = 0, sometimes = 2, and yes = 4). On the basis of the total THI score, patients can be classified into five categories denoting handicap severity: slight handicap (0-16), mild handicap (18-36), moderate handicap (38-56), severe handicap (58-76), or catastrophic (78-100) [11].2.2. Surgical technique: All patients underwent an underlay myringoplasty under general anesthesia, using the tragal cartilage and temporalis fascia as the grafting material Using Leica M525 F40 surgical microscope. Local injection was done by the subcutaneous injection of 1% or 2% local anesthetic with 1:200,000 adrenaline using syringe. Then, subperiostal injection of ear canal at the 6, 9 and 12 o’clock positions [12]. End aural approach was used; a small incision was made between the tragus and the helix. The canal was then opened with self-retaining aural retractors. Tympanic perforation is exposed and margins of TM perforation are excised before lifting the tympanomeatal flap. The skin incisions for the tympanomeatal flap are carried from the tympanic annulus at 7 o'clock and 1 o'clock in an ascending spiral fashion to meet the endaural incision [12]. Graft is placed in contact with mucosal surface in underlay technique. The tympanomeatal flap was then repositioned, and an antibiotic meatal pack was added [13]. The incision then sutured, and a mastoid bandage was used [14].In group A: full thickness tragal cartilage was used as graft material. Tragal cartilage was harvested by skin incision on the medial side of the tragus leaving 2 millimeter of outer edge cartilage in a dome of tragus for cosmetics then the donor site was closed with silk 3-0 cutting needle. The perichondrium was removed from convex surface of the tragal cartilage graft (which will face the promontory) and kept attached on other side. [15] A small incision was made in the skin of external canal wall 2-3 mm lateral to the annulus by angled knife. Subsequent limited lifting of the annulus to the middle ear [4].In group B: A partial thickness tragal cartilage graft was used by thinning the cartilage using cartilage forceps which had two rectangular jaws to hold the cartilage enabling reliable and precise cutting with the aid of a blade. A piece of cartilage is held between the enlarged, rectangular jaws of the forceps while using a scalpel to divide it. The result is two thin slices of cartilage, which can be further divided if required [7].In group C: Temporalis fascia was harvested by further retraction of the upper most part of the incision by a double hook retractor. Blunt dissection was carried out until temporalis fascia was reached. The small amount of saline injected to balloon the fascia away from the muscle. The fascia of adequate size was removed using scissors and the fascia was spread out "fascia down" on a small metal plate and left to dry through placing the graft over small bowl inverted over other bowel filled with boiled water. The graft is introduced under the anterior margin of the perforation. Support is provided by the tympanic sulcus (inferior and posterior) and by the bare tip of the malleus handle.2.3. Postoperative Care: The patient was given systemic IV antibiotics, Oral analgesics, and oral decongestants for 2 weeks. A Mastoid band was removed after 24 hours. Daily dressing of external wound with betadine solution, Stitches are removed after 6-7 days, Ear pack is removed after 7 to 10 days, Topical antibiotic and steroid ear drop were given for 2 weeks in the operated ear. Patients were advised to avoid lifting heavy things, blowing of nose, and devised to open mouth with sneezing [16].2.4. Follow up: The1st and 2nd follow up were after 3weeks and 6weeks respectively to evaluate healing of perforation and any defects or infections. In the 3rd follow up after 3 months, The following parameters were evaluated: Graft survival and perforation closure, postoperative otorrhea, residual perforation, improvement in the audiometric air-bone gap and THI and post-operative complications (wound dehiscence, sensorineural hearing loss, perichondritis, facial palsy and any other complication).2.5. Statistical analysis: Data were analyzed using Statistical Program for Social Science (SPSS) version 20.0. Quantitative data were expressed as mean± standard deviation (SD). Qualitative data were expressed as frequency and percentage. The following tests were done:A one-way analysis of variance (F=ANOVA) when comparing between more than two means.• Paired sample t-test of significance was used when comparing between related samples.• Chi-square (X2) test of significance was used to compare proportions between two qualitative parameters.• The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the p-value was considered significant as the following:• Probability (P-value)- P-value ≤0.05 was considered significant.- P-value ≤0.001 was considered as highly significant.- P-value >0.05 was considered insignificant.
3. Results
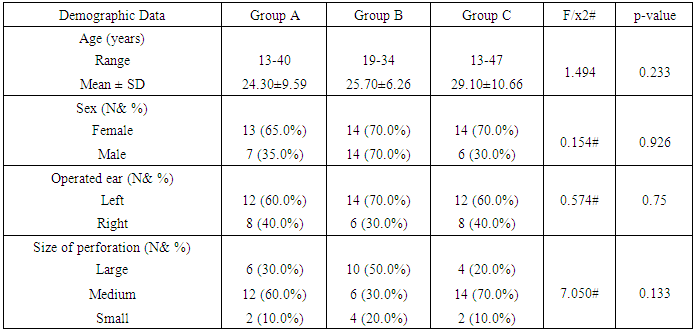
- Of the sixty patients were included in this study, 20 patients underwent full thickness tragal cartilage myringoplasty (group A) and 20 patients underwent partial thickness tragal cartilage myringoplasty (group B), and 20 patients underwent temporalis fascia myringoplasty (group C). The demographic data, including age, gender, side of surgery and the size of perforation of the three groups were summarized in Table (1). There were no statistically significant difference among the three groups.
|
|
|
|
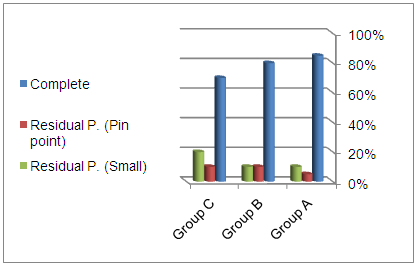 | Figure 1. Comparison between A, B and C groups according to graft take up |
|
4. Discussion
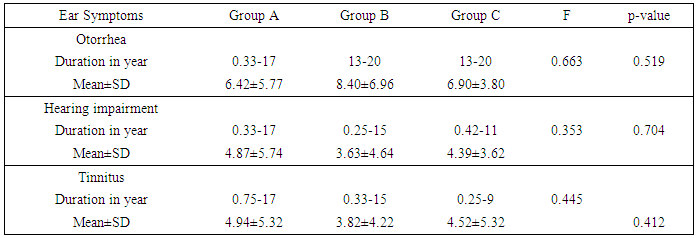
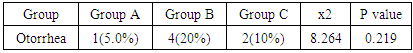
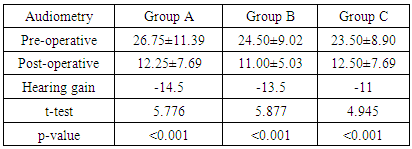
- Restoration of hearing is the main aim of functional reconstruction of the perforations of tympanic membrane by tympanoplasty [17]. Tinnitus is a commonly associated with Chronic otitis media, resulting in marked patient distress [18]. Now, various techniques are used to repair tympanic membrane perforation. [17]. Mass and stiffness of the graft differ significantly from that of the TM, so can alter the vibration pattern of the TM leading to acoustic transmission losses. The temporalis fascia vibrates easily in response to acoustic energy offering little resistance to static pressure while cartilage has excellent stability but may reflect most of the incoming sound [19]. Cartilage has constant, firmer shape than temporalis fascia [20].The aim of this work is to compare the results, in terms of graft uptake, hearing improvement and tinnitus using full thickness tragal cartilage, partial thickness tragal cartilage and temporalis fascia as grafting materials for myringoplasty.In this study, regarding to the age, gender, side of surgery and the size of perforation of the three groups are included in Table 1, there were no statistically significant different between three groups as summarized in (Table 1). This agree with Cavaliere et al., [21] who revealed no impact on post-operative hearing results on analysis of the patient data including sex and age, at the time of surgery. Mani et al., [22] also agree with us as they found no significant difference in graft take rate between male (85.7%) and females (81.8%). Nadol et al., [23] concluded that there is no significant effect of perforation side on the outcome of myringoplasty which also agree with us. Ashfaq et al., [24] also found no influence of perforated side on graft take up and that agree with us. But Samargandy et al., [25] study of the prognostic factor influencing tympanoplasty outcomes showed that males had higher success rate of 93.3% compared to female patients who had a rate of 70%. Therefore, male gender was a good prognostic factor in his study. As regarded to the size of the perforation, Wasson et al., [26] against us as he found that small perforation had better success rate than larger one. However Samargandy et al., [25] stated the contrary and noted a higher success rate of 87% in perforations smaller than 50% and a lower rate of 72.7% in perforations larger than 50% that disagree with us as well.Regarding to ear symptoms, preoperative main symptoms are otorrhea, impaired hearing and tinnitus; there was no statistically significant difference between groups summarized in (Table 2).This agree with Shetty [27] who found that commonest presenting complaints were ear discharge and hearing loss seen in all the (100%) patients.In this study as regarding to post-operative otorrhea, there was no statistically significant difference between the three groups. P value= 0.219. (Table 3) In this study, as regarding to post-operative functional success rate, pure tone audiometry showed statistically significant increase in hearing gain pre and post-operative in all groups .P value in the three groups were <0.001. (Table 4)Onal et al., [28] agreed with us as he reported functional success higher in cartilage group than fascia group, which agree with our results. Also Gamra et al., [29] agree with us, as the results showed good functional hearing results (ABG <20 dB) in 89% with cartilage graft which is higher than temporalis fascia graft of 82.8% with (p =0.005). Thus; post-operative hearing loss may be explained by the post-operative changes in the middle ear structures, regardless the graft type used for reconstruction. Mohamad et al., [30], Yakup et al., [31] and Yung et al., [32] were agreed with us as they concluded that functional results with cartilage were not different than with fascia grafts. Atef et al., [33] also agreed us who compared full thickness tragal cartilage graft (1mm) to partial thickness tragal cartilage graft (0.5mm) in tympanoplasty. They concluded that slicing the cartilage to half of its thickness added more to the technical difficulties without an actual hearing gain. However; Khan and Parab, [7] who worked on 233 ears, concluded that slicing the cartilage will counteract the disadvantage effect of the full thickness graft interfering with the sound transmission. In this study, successful graft takes up rate showing statistically insignificant difference (p value 0.791) between the 3 groups (Figure 1). This is in agreement with the study of Tan et al., [34] as they reported that cartilage (90.80%) has significant closure rate compared with temporalis fascia (88.00%). These results close to Yakup et al., [31] study, the graft success rate was 91.3% in the cartilage group and 68.9% in the fascia group. This in contrast to Jaiswal et al., [16] who showed successful closure of tympanic membrane was achieved in 91.43%, of the temporalis fascia group and 81.82% in cartilage group.In this study, regarding to Tinnitus, THI questionnaire showed statistically insignificant difference (p= 0.194) between pre and postoperative results in group A group while in group B and C showed statistically significant difference (P <0.001) (table 5). This agreed with Lima et al., [35] who evaluated patients with tinnitus who underwent tympanoplasty and found that 83% of the patients had improvement or elimination of tinnitus after surgery. Kim et al., [18] also agreed with us as they noted that tinnitus handicap inventory scores were reduced in 82% of patients following middle ear surgery.There were no cases of cartilage necrosis or resorption and no cases of iatrogenic cholesteatoma during the follow-up period.In full thickness tragal cartilage group(A), there was no graft retraction, but infection and re perforation in 3 cases and no hearing gain in 3 cases in spite of successful graft take up the graft and worsen of already present tinnitus in 3 cases.In partial thickness tragal cartilage group (B), there was no graft retraction but infection and re perforation in 4 cases and worsen of already present tinnitus in 2 cases.In fascia group(C), there was no graft retraction, no development or worsen of tinnitus, infection and re perforation in 6 cases and no hearing gain in 1 case in spite of successful graft take up the graft.
5. Conclusions and Recommendations
- Based on our results, it can be concluded that Grafting with Partial thickness cartilage counteracts the disadvantage effect of temporalis fascia and full thickness cartilage as graft material.The limitation of our study is that number of patients in our study was very small; in addition the follow up period was only 12 weeks. Zhang et al. [36] proposed that long follow up is essential needed as initial re-perforation especially in subtotal or total perforation was common. However, in Yakup et al. [31] showed no significant differences in re perforations, in all of the patients that were followed-up at least 1 year.
ACKNOWLEDGEMENTS
- To all contributors for maintaining and developing this research.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML