-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2018; 7(1): 15-19
doi:10.5923/j.otolaryn.20180701.04

Hyaluronic Acid Temporalis Fascia Graft Myringoplasty Versus Temporalis Fascia Graft Myringoplasty
Sayed M. S. Kadah1, Fatma M. Abd-Elgaber2, Sayed M. Mekhiemar3, Magda A. Mohammed4, Doaa F. S. Nour5
1Otorhinolaryngology Department, Al-Zahraa University Hospital, Cairo, Egypt (Professor of Otolaryngology)
2Otorhinolaryngology Department, Al-Zahraa University Hospital, Cairo, Egypt (Assistant Professor of Otolaryngology)
3Otorhinolaryngology Department, Al-Zahraa University Hospital, Cairo, Egypt (Professor & Head of Otolaryngology Department)
4Otorhinolaryngology Department, Al-Zahraa University Hospital, Cairo, Egypt, (Professor of Otolaryngology)
5Otorhinolaryngology Department, Fayed Hospital Ministry of Health, Cairo, Egypt (Specialist of Otolaryngology)
Correspondence to: Doaa F. S. Nour, Otorhinolaryngology Department, Fayed Hospital Ministry of Health, Cairo, Egypt (Specialist of Otolaryngology).
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The aim of the work: Improving the healing rate in tympanoplasty type 1. Objectives: To Evaluate the efficacy of Esterified Hyaluronic acid in the closure of central tympanic membrane perforation when added to a temporalis fascia and to compare its success rate in term of healing and hearing, with the of the superficial temporalis fascia grafts when used alone in the closure of central tympanic membrane perforations. Material and methods: A prospective non-randomized controlled trial at ENT department, Al-Zahraa University hospital (Tertiary care university hospital) between Oct. 2013 and Oct. 2015. Adult patients presented with small central TMP were operated under general anesthesia. The healed drum was considered when the complete closure was achieved. The patients were assessed by pure tone audiometry and tympanogram pre and postoperatively. Results: Twenty-two patients classified into group A (Hyaluronic acid temporalis fascia graft myringoplasty) and group B (temporalis fascia graft myringoplasty) (11 patients in each group) were included in the study. Healing occurred in 81.82% in group A, vs 72.73% in group B (p=0.61). Conclusion: the Esterified Hyaluronic acid that can be used to improve healing of tympanic membrane perforation. There is a statistically significant difference in the results of tympanic membrane healing and air-bone conduction gap; pre & post-operatively after using Esterified Hyaluronic acid.
Keywords: Hyaluronic acid, Central tympanic membrane perforation, The superficial temporalis fascia, Myringoplasty
Cite this paper: Sayed M. S. Kadah, Fatma M. Abd-Elgaber, Sayed M. Mekhiemar, Magda A. Mohammed, Doaa F. S. Nour, Hyaluronic Acid Temporalis Fascia Graft Myringoplasty Versus Temporalis Fascia Graft Myringoplasty, Research in Otolaryngology, Vol. 7 No. 1, 2018, pp. 15-19. doi: 10.5923/j.otolaryn.20180701.04.
Article Outline
1. Introduction
- Tympanic membrane perforation (TMP) results mainly from infectious and traumatic causes [1]. Perforations result from acute otitis media and trauma heal spontaneously in the majority of cases. But if there is a repeated infection or if the infection is persistent, there is less possibility of spontaneous healing of this perforation [2]. Long-standing tympanic membrane perforation may cause conductive hearing loss and middle ear infection even if it is a small perforation [3].Myringoplasty is a safe and effective technique to improve the quality of life of patients, avoiding continuous infections and allowing them to contact with the environment [4]. Myringoplasty is a beneficial procedure to protect the middle ear and inner ear from future deterioration [5]. Tympanic membrane perforation can be successfully repaired using a variety of graft materials. Commonly used grafts include autologous temporalis fascia, perichondrium, cartilage and adipose tissue [6].Hyaluronic acid has been found to accelerate tympanic membrane perforation closure, shorten the period of healing, and improve hearing; Hyaluronic acid is biodegradable, safe and biocompatible in the ear [7]. Hyaluronic acid improves tympanic membrane wound healing by inducing the production of keratin, which serves as a scaffold for migrating epithelium and preventing dehydration of the perforation margin. Hyaluronic acid also enhances hearing by producing better quality neo-membrane with a well-organized fibrous layer [8].Although there are many studies reporting the use of natural Hyaluronic acid in tympanic membrane repair, there is a lack of research on Hyaluronic acid in the closure of tympanic membrane perforation in Egypt.
2. Patients and Methods
- The study protocol and consent forms were approved by the research review committee. Written informed consent from all patients. A prospective clinical trial conducted at the ENT department at Al-Zahraa university hospital between 2013 and 2015. Twenty- two patients were selected from the ENT clinic; Patients were operated under general anesthesia. The patients were divided into two groups according to the type of graft used.Inclusion criteria were: Adult patients (18 year or older), Central tympanic membrane perforation, Small central perforation, grade 1 (Sizes of the TMP were graded according to Saliba classification) (Saliba, 2014), no evidence of otorrhea or active chronic otitis media, cholesteatoma, or retraction pocket formation, no suspected ossicular pathology on microscopic examination, preoperative air- bone gap of 35db or better, both sexes.Exclusion criteria were: Patients in whom the anterior and posterior rim of the perforation was not identifiable or was hidden by wall bulge of the external auditory canal, in order to avoid a blind surgical operation, perforation of grade 2 or more, associated vertigo, nystagmus, pregnancy, associated diabetes mellitus, recurrent perforation.All of the patients were subjected to the following:Complete history taking in the form of personal history, complaint, present history, past history. Microscopic examination of the ear, examine the external auditory canal, tympanic membrane perforation (site, size) and middle ear, after cleaning the cerumen and the external canal was gently cleaned with sterile cotton swabs which were soaked with alcohol.Capturing the tympanic membrane pre-operative to compare with postoperative healing with a digital otoscope. Audiometry: a pure tone for frequencies of 250, 500, 1000, 2000, and 4000 Hz. An air-bone gap was calculated for each patient, by getting the average of A-B gap differences at these frequencies. Patients with dry ears for a minimum period of 4 to 6 weeks were selected for surgery. All the patients were admitted on the previous day of operation and put on a broad spectrum antibiotic.
2.1. Technique of Grafting
- Freshening of the margin of the perforation is done first.Epithelium and mucosa adhered to the handle of the malleus are removed using sharp curved or straight pick. Classical Rosens incision is put and a posterior tympanomeatal flap is elevated. A 3 mm vertical incision is made on the graft, the graft is placed under the tympanomeatal flap and beneath the handle of the malleus in such a way that the incised part of the graft is taken around the handle of the malleus and spread upon the remaining of the pars flaccida. Esterified Hyaluronic acid pack insertion. Attention is taken to spread the graft properly and that the graft lies flat against the denuded portion of the membrane.
2.2. Statistical Analysis
- Data were collected, revised, coded and entered to the Statistical Package for Social Science (IBM SPSS) version 22.
3. Results
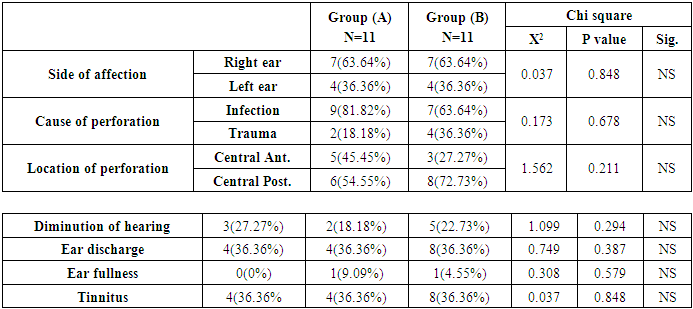
- 22 patients (18 females & 4 males) were enrolled in the study; they were divided into two equal groups, their age ranged between 18-47 years old.Group (A) included 11 patients (2 male & 9 female); with (mean age & SD) (26.09±5.907) ranged between (18-35) years (figure 1), Group (B) included 11 patients (2 male & 9 female); with (mean age & SD) (33.36±7.018) ranged between (22-47) years, “figure 1”. No statistical significance difference between the two groups as regard age, independent t test = 0.186 (p value >.05).
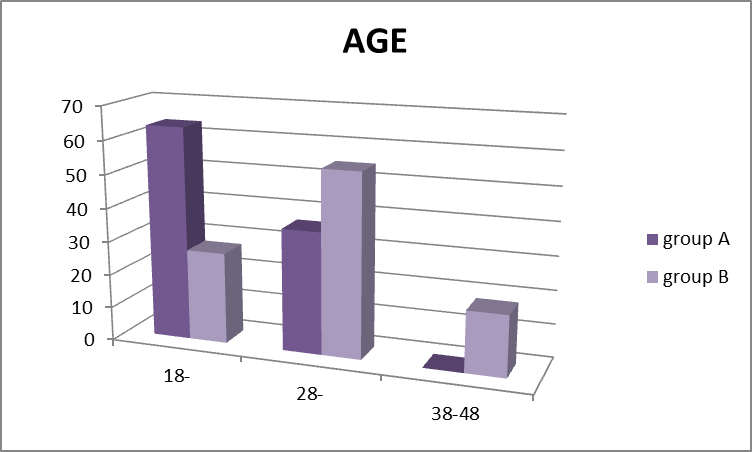 | Figure 1. Frequency distribution of studied patients according to age group |
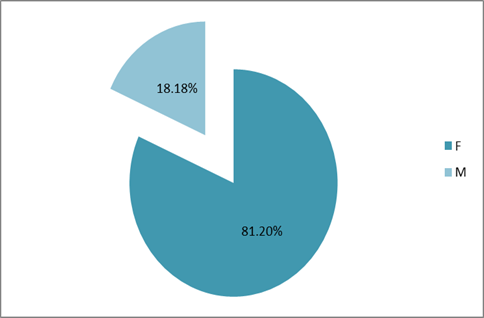 | Figure 2. Sex distribution among studied patients (group A, B) |
|
4. Discussion
- After searching the Egyptian Universities Libraries Consortium, it was found that the role of (Esterified HA) in the healing of the tympanic membrane perforations was not clinically studied in Egypt in the past 20 years. The aim of the current study is studying the efficacy of the Esterified Hyaluronic acid (EH) in the closure of tympanic membrane perforations, in an attempt to try the modern resources to achieve the best myringoplasty outcome; Tympanic membrane perforation remains a major healthcare burden and management challenge. Hyaluronic acid is a naturally occurring high-molecular- weight linear glycosaminoglycan with excellent visco-elastic, rheological and hygroscopic properties that play prominent roles in all stages of inflammation and wound healing [9].The objectives of the current study were, to determine the difference between the superficial temporalis fascia grafts (sTFG) when combined with the esterified Hyaluronic acid (EH) versus (sTFG) without (EH) in the closure of tympanic membrane perforations in underlay tympanoplasty type I and to compare the hearing results between both techniques. The current study, included 22 patients (81.82% females & 18.18% males) ranged between 18-47 years old, with the mean age of (29.73 ± 7.343) the distribution of cases according to their sex and age revealed no statistical significant difference (P>0.05). In the present study, small central tympanic membrane perforation “figure 3” was treated using esterified Hyaluronic acid in combination with superficial temporalis fascia graft “figure 4” in group (A), & the graft uptake occur in (80%) of the patients, Stenfors in 1989 studied fifteen dry tympanic membrane perforations (small or medium-sized) were treated by local application of 1 per cent Hyaluronic acid after excision of the perforation rim. Fourteen of the perforations were healed; Stenfors reported that Hyaluronic acid treatment of dry tympanic membrane perforation not exceeding one quadrant seems to be an alternative to surgical myringoplasty [10].
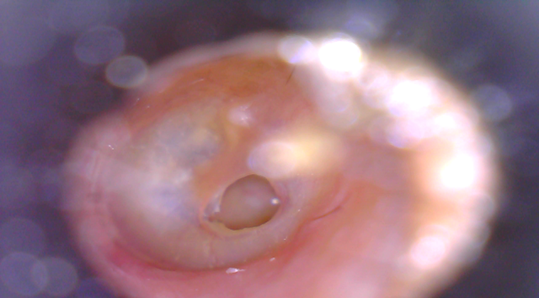 | Figure 3. RT central tympanic membrane perforation, ENT department at Al-zahraa university hospital, Cairo |
 | Figure 4. Superficial temporalis muscle fascia, ENT department at Alzahraa university hospital |
5. Conclusions
- There were no articles found comparing between the using of temporalis fascia versus the combination between temporalis fascia and esterified Hyaluronic acid in the literature.The Esterified Hyaluronic acid that can be used to improve healing of tympanic membrane perforation. There is a statistically significant difference in the results of tympanic membrane healing and air-bone conduction gap; pre & post-operatively after using Esterified Hyaluronic acid.
ACKNOWLEDGEMENTS
- To all the contributors for developing and maintaining this research.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML