-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2017; 6(6): 81-87
doi:10.5923/j.otolaryn.20170606.02

Quality of Life in Patients with Nasal Obstruction after One Year of Septoplasty
Abdullah Alotaibi
Department of Otolaryngology Head and Neck Surgery, College of Medicine, Hail University, Saudi Arabia
Correspondence to: Abdullah Alotaibi, Department of Otolaryngology Head and Neck Surgery, College of Medicine, Hail University, Saudi Arabia.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Nasal blockage is a frequent cause of increased nasal airway resistance, which has negative impact in the quality of life. Therefore, the aim of this study was to assess the quality of life in patients with nasal obstruction after one year of septoplasty. Methodology: This study included a series of patients presented with nasal obstruction and subsequently undergone septoplasty. Several nasal obstruction clinical complains were evaluated included: nasal congestion, nasal blockage, breathing trouble, sleeping trouble, and exercise problem. Results: The majority of patients attended with nasal blockage followed by breathing trouble, sleeping trouble, nasal congestion, exercise problem, and other complications, representing 123(94%), 114(87%), 110(84%), 109(83.2%), 93(71%) and 5(3.8%), respectively. Conclusion: Septoplasty leads to a highly significant enhancement in quality of life and relief of symptoms.
Keywords: Septoplasty, Nasal blockage, Breathing trouble, Nasal congestion, Sleeping trouble
Cite this paper: Abdullah Alotaibi, Quality of Life in Patients with Nasal Obstruction after One Year of Septoplasty, Research in Otolaryngology, Vol. 6 No. 6, 2017, pp. 81-87. doi: 10.5923/j.otolaryn.20170606.02.
1. Introduction
- Nose is a mean for evaluating the disease-specific quality of life associated with nasal obstruction. Nasal obstruction is a public complaint in several population settings. Deviated nasal septum (DNS) might cause nasal obstruction and negative impact on the quality of life of individuals [1]. When caused by a DNS, septoplasty is the method of choice for the treatment these patients [2]. Nasal blockage or inadequate air flow via the nose, can impact significantly on the person's quality of Life. The prevalence nasal obstruction greatly vary [3]. There are many factors incriminated as causes for nasal obstruction, include: rhinitis, adenoid hypertrophy, turbinate hypertrophy and sinonasal polyps. DNS is a very mutual cause of nasal obstruction, of simple diagnosis and eventual treatment is based on septoplasty.DNS have a prevalence ranging from 19 to 65 % due to diverse criteria for describing a deviated septum [4, 5].Septoplasty is the third most common surgery [6] done in the ear nose and throat (ENT) specialty and can be performed under local or general anesthesia, and the procedures might be very challenging for some surgeons. A precise preoperative diagnosis is important for the success of surgery. Intraoperative imagining through microscope or endoscope is very supportive for the surgeon. The current method of septoplasty with the stages of approach, mobilization, resection/repositioning and reconstruction/fixation is offered. As pathologies of the caudal septum are responsible for failures of septal surgery, some special problems of this region such as the vertical fracture of the caudal septum, the lack of caudal septum or anterior convexities of the cartilaginous septum are debated [7].Septoplasty as is one of the most common operations done in otolaryngology, usually anterior nasal packing is done regularly to avoid postoperative bleeding, septal hematoma or nasal synechia. At present, transseptal sutures have gained a bigger practice area, not only for preventing the complications such as septal hematoma and bleeding but also closing any accidental tears of septal mucosa and bringing extra support for the cartilage pieces reserved in septoplasty [8].Complications related to submucous septal resection or septoplasty may create improper sign and diagnosis due to incorrect or partial analysis and interpretation of the anatomical structures of the nose and nasal function tests. Complications can rise from methodological failures throughout the techniques of septal surgery from the incision to the reconstruction of the septum. Early and late complications can be caused by infections in the postoperative period encompassing only the mid-facial region or the entire body. Postoperative and late complications may also arise from damage to the septal soft and hard tissues [9].Our perception on health and health care is fluctuating. Substantial factors in this modification are insights on the social magnitudes of diseases and the knowledge that medical interventions may lengthen life and improve quality of life [10, 11]. Thus the consequence analysis is one of the essential means for the evaluation of quality of medical care. Therefore, the aim of this study was to assess Quality of life in patients with nasal obstruction after one year of septoplasty.
2. Materials and Methods
- This study included a series of patients presented with nasal obstruction and subsequently undergone septoplasty. Archives related to all patients selected for septoplasty between 2012 and 2017 were retrieved from ear, nose, throat (ENT) department, King Khalid hospital in Hail, Northern Saudi Arabia. Only adults over 18 years of age were included in the study. Patients’ medical records were investigated, and patients with a history of rhinoplasty, cranial and facial trauma or bone deformity (except DNS), and patients with a mass in the nasal cavity were excluded from the study. Only patients with apparent nasal obstruction related clinical presentation (complains) were considered. Several nasal obstruction clinical presentations were recorded included: nasal congestion, nasal blockage, breathing trouble, sleeping trouble, and exercise problems. Demographical characteristics including; age, gender and residence were also recorded.The different initial clinical presentations and complications were compared after three one year of septoplasty.Ethical consentOur study protocol was conformed according to the 2013 Declaration of Helsinki and this study was approved by ethics committee of College of Medicine, University of Hail, Saudi Arabia.Statistical analysisStatistical analysis was performed using SPSS software for Windows (version 16.0, SPSS Inc., Chicago, IL, USA). Categorical variables are given as frequencies and percentages, and continuous variables. For all statistical comparisons, a p value below 0.05 was considered statistically significant.
3. Results
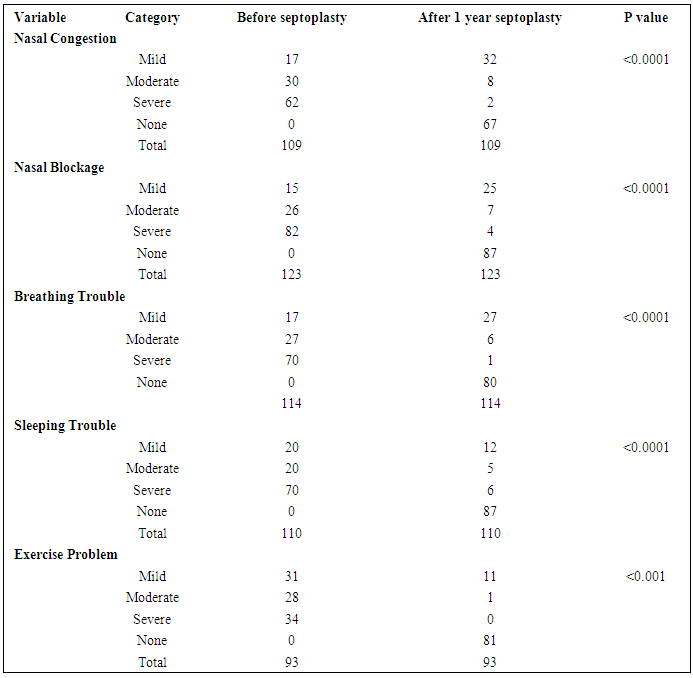
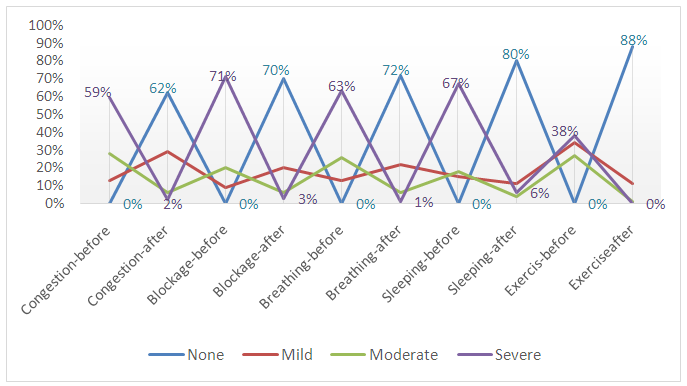
- This study investigated patients presented with different clinical complains related to nasal obstruction. Out of the 131 patients, 112(85.5%) were diagnosed with DNS and the remaining 19 (15.5%) patients were diagnosed with other nasal obstructive disorders. The majority of patients attended with nasal blockage followed by breathing trouble, sleeping trouble, nasal congestion, exercise problem, and other complains, representing 123(94%), 114(87%), 110(84%), 109(83.2%), 93(71%) and 5(3.8%), respectively.Table 1 summarizes the distribution of the patients by nasal obstruction related clinical complications before septoplasty and after one year of septoplasty. For nasal congestion, symptoms completely disappeared from 67/109(61.5%) patients. Severe and moderate symptoms present only in 2/62(3.2%) and 8/30 (26.7%) respectively, as indicated in Table 1, Fig 1. These findings indicated that septoplasty is important for the management of nasal congestion and this was found to be statistically significant P <0.0001.
|
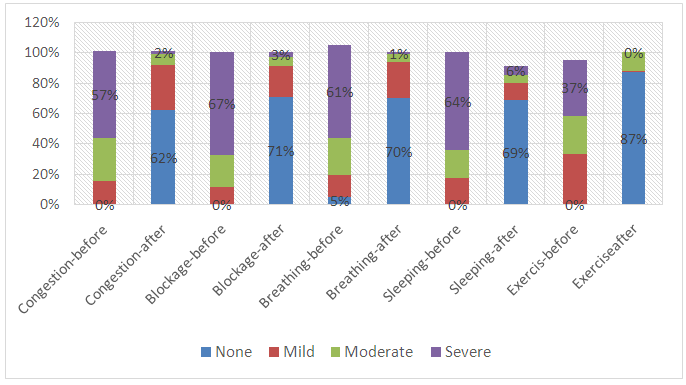 | Figure 1. Description of patients by clinical symptoms at initial presentation and after one year of septoplasty |
|
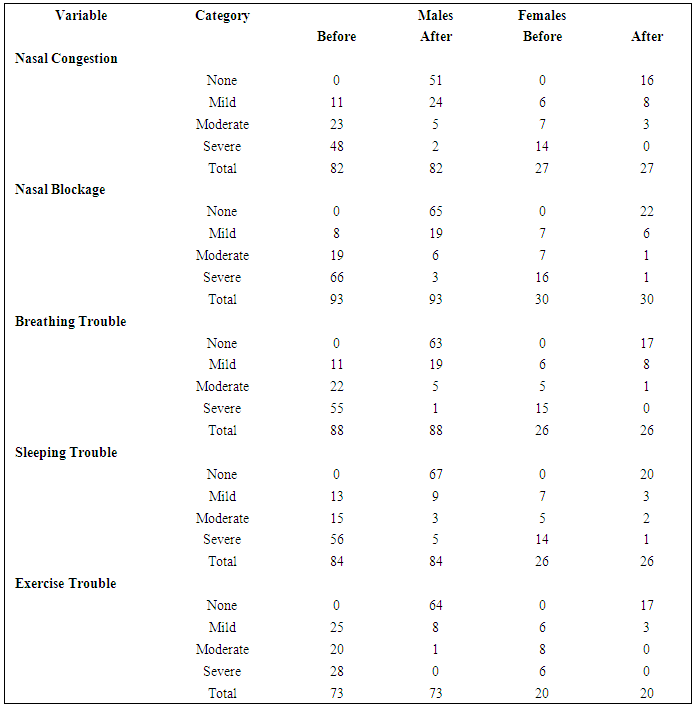
 | Figure 2. Description of males’ patients by clinical presentations and gender at initial presentation and after one year of septoplasty |
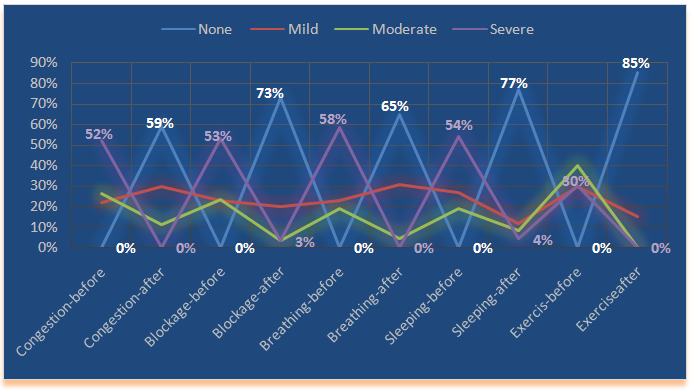 | Figure 3. Description of females’ patients by clinical presentations and gender at initial presentation and after one year of septoplasty |
|
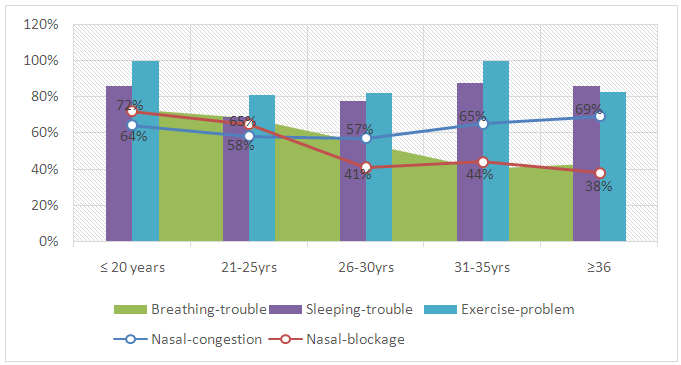 | Figure 4. Description of patients by complete resolve of nasal obstruction related complications after one year of septoplasty |
4. Discussion
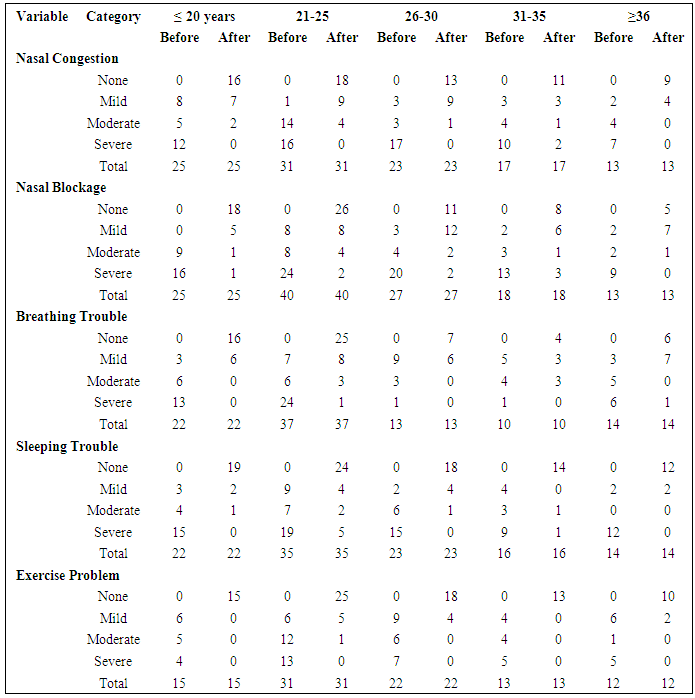
- The assessment of quality of life after certain surgical procedures plays an important aspect of research outcomes has received growing significance in latest years. Consequently in the present study we tried to evaluate the ultimate improve of quality of life after one year of septoplasty. Our assessment depend on the absence or reduction in the degree of the initial clinical complains related to nasal obstruction before septoplasty. This is done through the follow up of patients for one year after septoplasty.Of the clinical complains evaluated in the present study was nasal congestion. Nasal congestion completely eliminated from 61.5% of the patients and comforted to lower degrees in the majority of them. Moreover, nasal blockage was completely eliminated in 70.7% of the patients with significant lowering in the severity of all cases. However, similar outcomes were previously reported. One study found that septoplasty was successful relieved nasal obstruction in 70.5% of patients. Rhinitis, including allergy, congestion, postnasal drip and rhinorrhea did not significantly disturb the success in relieving nasal obstruction [11]. This positive association between septoplasty and relief of nasal congestion and/or obstruction was supported by several studies [12, 13]. However, some studies have another point of view, that Long-term results after septoplasty are inadequate. Apart from a recurrence of deviation, there are various reasons for this: false preoperative analysis, complete straightening of the septum, and a distressed nasal cycle. Preoperative functional diagnostics with a combination of rhinoresistometry, acoustic rhinometry, and long-term rhinoflowmetry are essential for distinguishing between "physiological" and "pathological" septal deviations and spotting other causes for nasal obstruction. The surgical method of septoplasty comprises methodology, mobilization, resection, reposition, and lastly rebuilding of all three layers. The goal of the operation should not be complete straightening of the nasal septum. The space between the septum and turbinates is of utmost importance [14]. However, the majority of studies evaluating the objective advantage of septoplasty did not follow the recommendations of the committee report on the standardization of rhinomanometry. Only three prospective controlled trials, with pooled data from 141 cases, were identified for meta-analysis, which concluded that it can be drawn regarding objective improvement in airway function next nasal septal surgery are limited. More long-term studies, adhering to standardized procedures, are required to deliver more substantial results [15].Furthermore, in the present study, breathing troubles, sleeping troubles and exercise problems have disappeared from around 70%, 97.2% and 87% of the patients respectively. Several studies reported that septoplasty could be recommended for patients with breathing troubles to ensure better nasal breathing outcomes. This was found to be significantly improve the nasal breathing quality of life [16-18]. For particular evaluation of septoplasty consequence measurement nasal obstruction symptom score (NOSE) and sino-nasal outcome test (SNOT22) forms offer exceedingly predictive values [19-21]. Subjective evaluation of upper airway is usually done with rhinomanometry and acoustic rhinometry, which are used by investigators as well. It was found that septoplasty has a positive outcome on pulmonary functions, and this can be an important hint for the association between lung disorders and nasal obstruction [22].In conclusion: Septoplasty leads to a highly significant improvement in quality of life and relief of symptoms. Septoplasty is a very effective and satisfactory treatment for nasal congestion, nasal blockage, breathing trouble, breathing trouble, sleeping trouble and exercise problems caused by nasal septal deviation. Ultimate benefit can be assessed after one year of septoplasty. Author would like to thank doctors Bassam Ahmed Almutlaq, Fawaz sulaiman alshammari, Abdulrahman Saeed Alharbi, Abdullah Ahmed Alkhalaf, for their help in sample collection and Prof. Hussain Gadelkarim Ahmed for manuscript revision.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML