-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2017; 6(6): 73-80
doi:10.5923/j.otolaryn.20170606.01

Post-surgical Outcomes of Patients Undertaken Septoplasty with Regard to Initial Clinical Complains
Abdullah Alotaibi1, Bassam Ahmed Almutlaq2
1University of Hail, College of Medicine, Department of Otolaryngology Head and Neck Surgery, Saudi Arabia
2University of Hail, College of Medicine, Saudi Arabia
Correspondence to: Bassam Ahmed Almutlaq, University of Hail, College of Medicine, Saudi Arabia.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Septoplasty is commonly performed to offer qualitative and quantitative advantage to those with nasal obstruction owing to septal deviation. Therefore, the aim of the present study was to assess the post-surgical outcomes of patients undertaken septoplasty with regard to initial clinical complains. Methodology: This study included a series of patients presented with nasal obstruction and subsequently undergone septoplasty. In the present study, patients presented with different clinical complains; 83.2% presented with nasal congestion, 94% with nasal blockage, 87% with breathing trouble, 84% with sleeping trouble, 71% with exercise problem, and 3.8% with other complications (e.g bleeding, loss of smell). Conclusion: In patients with nasal obstruction due to DNS or other causes, nasal septoplasty results in significant improvement in reduction or completely eliminates the prior complications.
Keywords: Septoplasty, Deviated nasal septum, Nasal obstruction, Breathing trouble
Cite this paper: Abdullah Alotaibi, Bassam Ahmed Almutlaq, Post-surgical Outcomes of Patients Undertaken Septoplasty with Regard to Initial Clinical Complains, Research in Otolaryngology, Vol. 6 No. 6, 2017, pp. 73-80. doi: 10.5923/j.otolaryn.20170606.01.
1. Introduction
- Septoplasty or surgical modification of the deviated nasal septum (DNS), is the most common ear, nose and throat (ENT) operation in adults [1]. Patients with a septal deviation and worries about nasal obstruction regularly undertake septoplasty to mend nasal airflow [2]. Obstructed nasal breathing can happen due to deviation of the nasal septum. When the external nose looks grossly normal and cosmetics is not the emphasis, septoplasty has been the method performed to straighten the septum with the goal of improving nasal airflow [3].Presently, the key sign to do septoplasty is nasal obstruction. Nasal obstruction is commonly defined as patient discomfort manifested as a sensation of inadequate airflow through the nose [4]. The etiology of nasal obstruction is generally divided into mucosal and anatomical causes. DNS is the most common anatomical cause of nasal obstruction [5]. Still, underlying pathogenesis is often multifactorial. For example, DNS is commonly attended with compensatory mucosal hypertrophy of the contralateral turbinate [6]. This corrected mechanism is presumed to shield the more patent nasal side from the drying and crusting effects of extra airflow [7]. Compensatory hypertrophy can happen in both the inferior as well as the middle turbinate on the side contralateral to nasal septal deviation [8]. It has been revealed that turbinate amplification not only includes mucosal elements, but may also encompass the conchal bone [6]. Since these variations may not be spontaneously reversible, they sometimes requisite to be amended in combination with septal surgery to prevent nasal obstruction on the non-deviating side postoperatively [9, 10]. By straightening the DNS and carrying out simultaneous turbinate surgery, nasal passages are expected to extend and as a consequence nasal breathing is thought to improve.At present the efficacy of septoplasty in adults with nasal obstruction and a DNS remains uncertain. Objective measurements do not always correlate with subjective measures to evaluate the efficiency of septoplasty [11]. Furthermore, additional benefits of corresponding turbinate surgery are unidentified, and signals and procedures applied vary greatly [12, 13]. Unusually, the literature displays a prevalence of nasal septal deviation of up to 80 %, while only a minority of subjects suffers from nasal obstruction [14]. More essential in this respect, is the fact that scientific publications on the effects of septoplasty are rare and inadequate [14].Following primary septoplasty, however, some patients have persistent symptoms due to nasal valve dysfunction and may need nasal valve surgery. Nasal valve dysfunction remains an underdiagnosed entity and should be considered in all patients with septal deviation before septoplasty, especially in patients with a severe dorsal deflection and a narrow middle vault [2]. Therefore, the aim of the present study was to assess the post-surgical outcomes of patients undertaken septoplasty with regard to initial clinical presentations and complications.
2. Materials and Methods
- This study included a series of patients presented with nasal obstruction and subsequently undergone septoplasty. Archives related to all patients selected for septoplasty between 2012 and 2017 were retrieved from ENT department, King Khalid hospital in Hail, Northern Saudi Arabia. Only adults over 18 years of age were included in the study. Patients’ medical records were investigated, and patients with a history of rhinoplasty, cranial and facial trauma or bone deformity (except DNS), and patients with a mass in the nasal cavity were excluded from the study. Several nasal obstruction clinical presentations were recorded included: nasal congestion, nasal blockage, breathing trouble, sleeping trouble, and exercise problems. Demographical characteristics including; age, gender and residence were also recorded.The different initial clinical presentations and complications were compared after three months of septoplasty.Ethical consentOur study protocol was conformed according to the 2013 Declaration of Helsinki and this study was approved by ethics committee of College of Medicine, University of Hail, Saudi Arabia.Statistical analysisStatistical analysis was performed using SPSS software for Windows (version 16.0, SPSS Inc., Chicago, IL, USA). Categorical variables are given as frequencies and percentages, and continuous variables. For all statistical comparisons, a p value below 0.05 was considered statistically significant.
3. Results
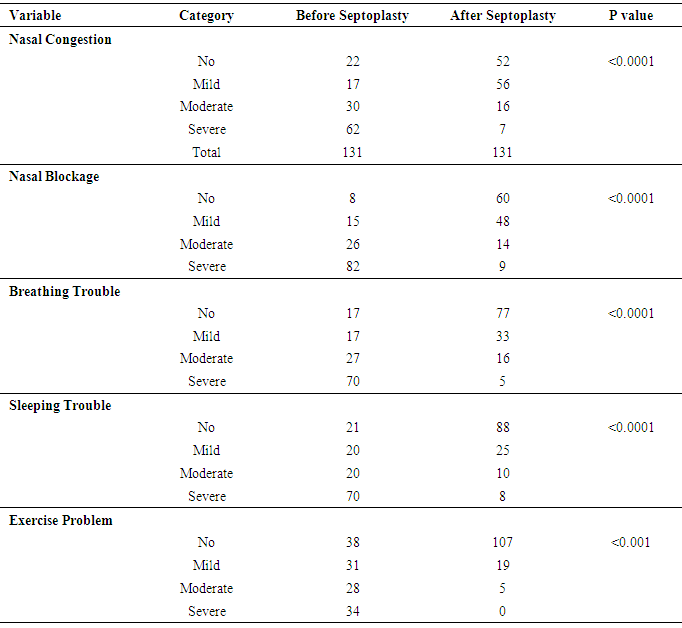
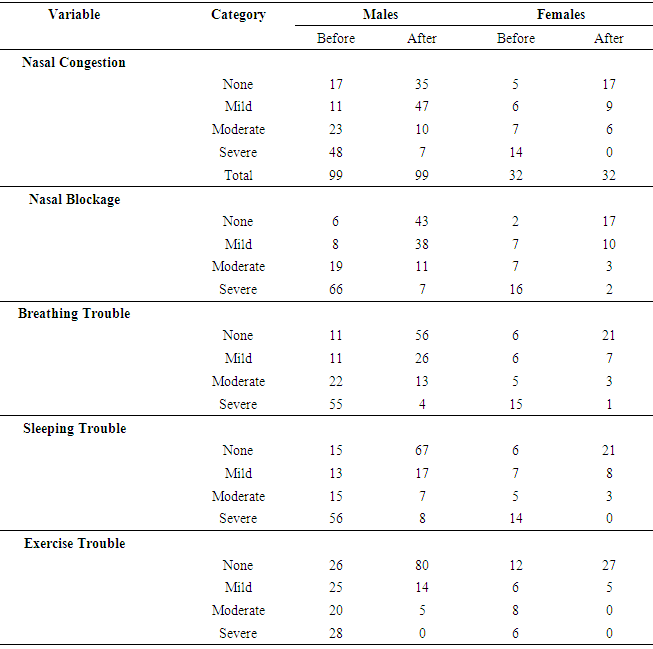
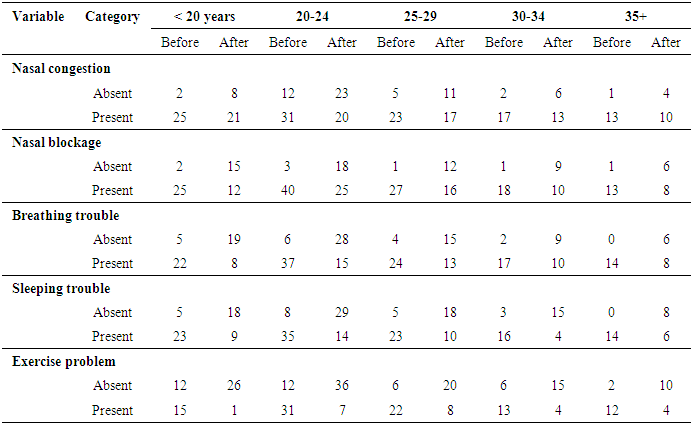
- In the present study, 131 patients presented with clinical presentations mainly nasal obstruction subjected them for septoplasty selection. Out of the 131 patients, 112 were diagnosed with deviated nasal septum (DNS) and the remaining 19 patients were diagnosed with other nasal obstructive conditions. The 131 patients presented with different clinical presentations; 109/131(83.2%) presented with nasal congestion, 123/131(94%) with nasal blockage, 114/131(87%) with breathing trouble, 110/131(84%) with sleeping trouble, 93/131(71%) with exercise problems, and 5/131(3.8%) with other complications (e.g bleeding, loss of smell). Table 1 summarizes the distribution of the study population by nasal obstruction related clinical complications before septoplasty and after 3 months of septoplasty. For nasal congestion, symptoms completely disappeared from 30/131(22.9%) patients. Severe and moderate symptoms disappeared from 55/62(88.7%) and 14/30 (46.7%) respectively, as indicated in Table 1, Fig 1. These findings indicate that septoplasty is critical for the treatment of nasal congestion and this was found to be statistically significant P <0.0001.For nasal blockage, symptoms completely disappeared from 52/131(39.7%) patients. Severe and moderate symptoms disappeared from 73/82(88%) and 12/30 (40%) respectively, as indicated in Table 1, Fig 1. These findings indicate that septoplasty is critical for the treatment of nasal blockage and this was found to be statistically significant P <0.0001.For breathing trouble, symptoms completely disappeared from 60/131(45.8%) patients. Severe and moderate symptoms disappeared from 65/70(93%) and 11/30 (36.7%) respectively, as indicated in Table 1, Fig 2. These findings indicate that septoplasty is critical for the treatment of breathing trouble and this was found to be statistically significant P <0.0001.For sleeping trouble, symptoms completely disappeared from 67/131(51%) patients. Severe and moderate symptoms disappeared from 62/70(88.6%) and 10/30 (33.3%) respectively, as indicated in Table 1, Fig 2. These findings indicate that septoplasty is critical for the treatment of sleeping trouble and this was found to be statistically significant P <0.0001.For exercise problems, symptoms completely disappeared from 69/131(52.7%) patients. Severe and moderate symptoms disappeared from 34/34(100%) and 25/30 (83.3%) respectively, as indicated in Table 1, Fig 2. These findings indicate that septoplasty is critical for the treatment of exercise problem and this was found to be statistically significant P <0.0001.The distribution of patients by clinical presentation before and after septoplasty by gender was summarized in Table 2. All clinical presentations (including: nasal congestion, nasal blockage, breathing trouble, sleeping trouble and exercise problem) were significantly improved after 3 month of septoplasty (P <0.0001) both for males and females. However, within each sex kind there was variations within the degree of symptoms, as shown in Fig 3, Fig 4.Table 3 summarised the distribution of the study population by age. The improvement after septoplasty was statistically significant in all age groups (P < 0.0001). However, the improvement has inconsistent variability in different ages, as indicated in Table 3.Other complications such as bleeding and loss of smell were completely disappeared.
|
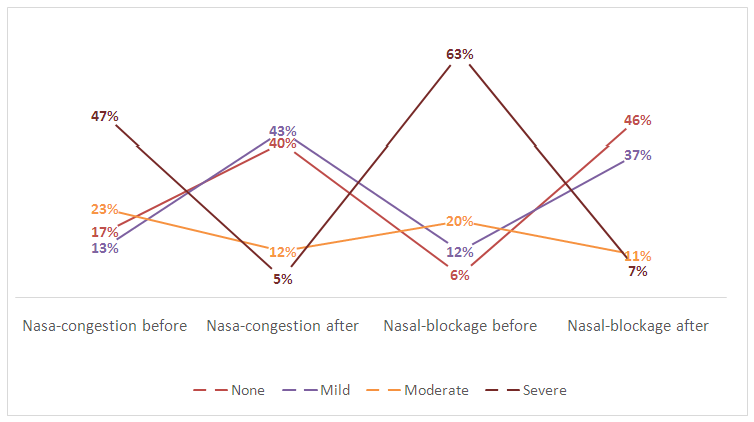 | Figure 1. Description of the patients by nasal congestion & nasal blockage and degree of symptoms before and after 3 months of septoplasty |
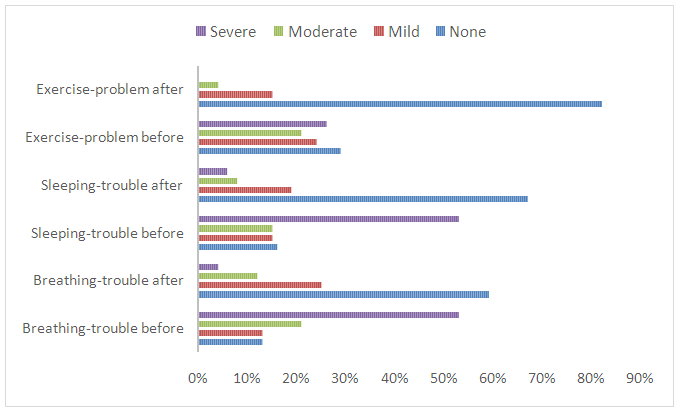 | Figure 2. Description of the patients by breathing trouble, sleeping trouble, exercise problem and degree of symptoms before and after 3 months of septoplasty |
|
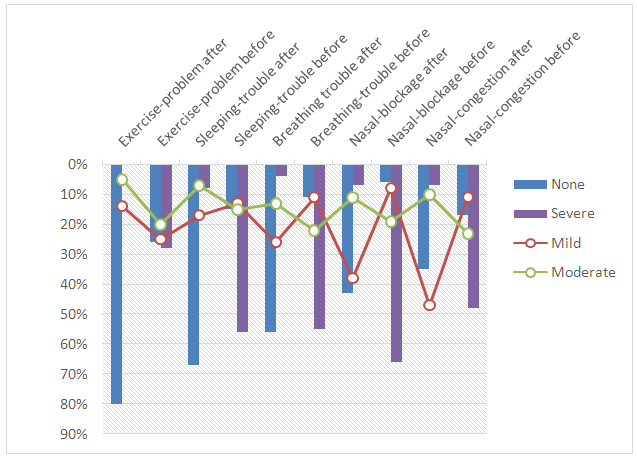 | Figure 3. Description of males by clinical presentations before and after septoplasty |
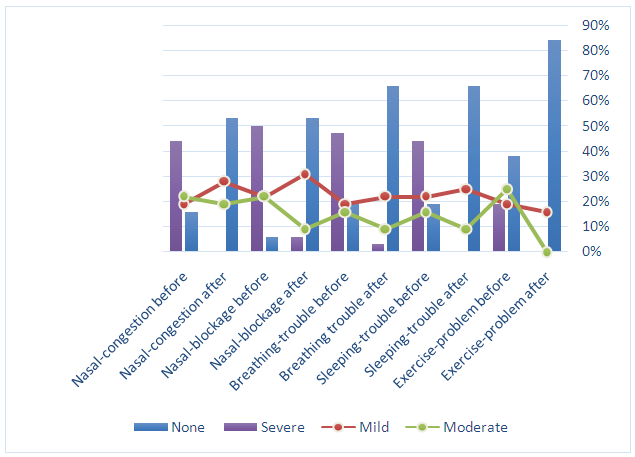 | Figure 4. Description of females by clinical presentations before and after septoplasty |
|
4. Discussion
- In the present study, patients presented with multiple clinical presentations and complications with most frequently encountered; nasal congestion, nasal obstruction, breathing trouble, sleeping trouble, exercise problems. Moreover, some patients attended with complications such as bleeding and loss of smell. However, the initial diagnosis for this series included DNS in 112(85.5%) and the remaining 19(14.5%) have nasal obstructive but without DNS. Although, there are varying prevalence rates of DNS, our findings in the present study might be categorized within the highest occurrence rates among patients presented with nasal obstruction. In a study to determine the prevalence of nasal septal deformities among Turkish school children, the overall prevalence of NSD has been found to be 34.9%. For the age groups, the prevalence of NSD was 16.5% in pre-school children, 38.7% in primary school children and 39.9% in secondary school children [15]. In another study to classify the NSD according to the Guyuron and Mladina classifications, and to evaluate the correlation between anterior rhinoscopy and CT findings. Of 970 patients, 50.3% had NSD. According to the Guyuron and Mladina classifications, type 2 (41.4%) and type 1 (35.4%) were most common, respectively [16].However, in the present study all studied clinical presentations including nasal congestion, nasal obstruction, breathing trouble, sleeping trouble, exercise problems; have significantly all disappeared or reduced to lower degrees (severe became moderate or mild). These findings indicated the benefit of septoplasty in management of DNS and other causes of nasal obstruction. However, the outcomes of septoplasty differ according to many factors including the method of performance. There are multiple different methods of performing this operation. Each specific method of performing a septoplasty has its own benefits and advantages. Irrespective of the method, septoplasty is a valuable procedure in nasal surgery [17]. Subjects with anterior septal deformities were shown to benefit the most from septoplasty. Selection of patients on clinical grounds alone does carry, however, a considerable risk of patient dissatisfaction with end results. Nevertheless, despite a very strong correlation between anterior septal deviations and increased nasal resistance, preoperative rhinomanometry data failed to prove useful in predicting the long-term surgical outcome. Surgeons' appreciation of the types of septal deviation that do benefit from surgical correction falls short of desirable. Patients' satisfaction, however, did not improve if rhinomanometry was included in the preoperative evaluation [18]. Anterior septal reconstruction has been shown to be a safe and effective means by which to address severe caudal septal deviation and long-term reduction in preoperative symptoms [19].Nevertheless, there are some studies reported similar findings to our results. In a study investigated 86 patients with septal deviation they were asked using an outcomes instrument (the Nasal Obstruction Symptom Evaluation scale) before and 3 and 6 months after septoplasty. Seventy-seven patients (89.5%) reported a subjective improvement in their nasal obstruction [20].Despite the significant number of septoplasties performed each year, complications after this procedure are relatively uncommon. Most complications result from inadequate surgical planning or poor technique and often can be prevented. Surgeons should discuss these risks with patients before surgery as part of the informed consent process. The septoplasty surgeon must be aware of all the possible complications that may arise so as to convey the benefits and risks of surgery effectively to prospective patients [21].Septoplasty may lead to the following complications: nasal obstruction, nasal septal hematoma, nasal septal abscess, saddle nose or other nasal deformity, nasal septal perforation, epistaxis, acute or chronic rhinitis. All these complications are rare (occurring in less than 1 % of all cases) and most of them resolve without additional treatment. In selected cases, an additional intervention (drainage of hematoma or abscess, antibiotics, additional nasal packing, surgical correction of saddle nose or other nasal deformities) may be needed to resolve the complication [1]. However, none of these complication has been experienced in our series.Although the findings of the present study may provide platform as well as inspiration for further research in this perspective but it has some limitations; sleeping distress, breathing distress, nasal congestion, exercise unease, and other complaints, are to some extent subjective rather than to be measureable, but at least give some orientations in this context.
5. Conclusions
- In patients with nasal obstruction due to DNS or other causes, nasal septoplasty results in significant improvement in reduction or completely eliminates the prior complications. Patients with nasal obstruction due to causes other than DNS can benefit from septoplasty to the same extent as patients with septoplasty.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML