-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2017; 6(3): 40-43
doi:10.5923/j.otolaryn.20170603.02

Management of Auricular Keloids using Scar Based Skin Flap
Karthik Shamanna, Veena B. Ganga, Lakshmi Priya S.
Department of ENT, Bangalore Medical College & RI, Bangalore, India
Correspondence to: Karthik Shamanna, Department of ENT, Bangalore Medical College & RI, Bangalore, India.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

A prospective study was conducted to evaluate the effectiveness of scar based flap in treating auricular keloid. This study included 30 patients with auricular keloid between ages 18 to 60 years. All patients underwent keloid excision with scar based flap technique under local anesthesia. Post-operative intralesional steroid was given in four sittings at weekly interval. All patients were followed up for a period of one year. Of the 30 patients, three patients (10%) complained of pain and two patients (6.6%) complained of pruritis post-operative. Three cases of recurrence were reported during the follow up period of 1 year. Scar based flap excision combined with post-operative steroid injections give good results in terms of cosmesis and maintenance of auricular contour. Avoidance of tension, accurate approximation of wound margin and good vascularity are the important factors in reducing the recurrence rate of auricular keloids following surgical excision.
Keywords: Auricular keloid, Intralesional steroid, Scar based flap
Cite this paper: Karthik Shamanna, Veena B. Ganga, Lakshmi Priya S., Management of Auricular Keloids using Scar Based Skin Flap, Research in Otolaryngology, Vol. 6 No. 3, 2017, pp. 40-43. doi: 10.5923/j.otolaryn.20170603.02.
Article Outline
1. Introduction
- The head and neck region is prone to frequent injuries due to its delicate nature, resulting in hypertrophied scar or keloid formation. The pinna in particular is commonly affected largely due to ear piercing and the presence of cartilage. Unfortunately the exact mechanism of keloid formation still eludes us. Hence the treatment of keloid remains enigmatic and often involves controversial and unconventional therapies including the use of radiation. Following injury to the skin, normal healing involves the proliferation of fibrous ingrowth to repair the damaged tissues. When there is an excessive local tissue response to injury, a dysregulated deposition of extracellular matrix and collagen occurs resulting in either a hypertrophic scar or keloid [1]. Skin, particularly over cartilages such as pinna, ala of nose, sternum etc is very rich in collagen and fibrous tissue, this could probably explain the common occurrence of hypertrophied scar or keloid over these regions.Scars with aesthetically unfavorable characteristics include those that are wide, misaligned with relaxed skin tension lines or aesthetic subunits, thickened, hypertrophied scars or keloids.Several treatment options are available, including steroid injections, silicone sheeting, pressure dressing, surgery, radiation therapy and combined approaches. In spite of the growing research on pathogenesis of keloids, the current best treatment modality for keloid is still not determined. However, complete surgical excision of the keloid followed by post-operative intralesional steroid therapy remains the most accepted modality of treatment.
2. Objectives of the Study
- To evaluate the effectiveness of scar based flap technique in treating auricular keloids.
3. Materials and Methods
- A Prospective study was conducted over a period of one year (January 2015-2016) at the department of ENT, Bangalore Medical Collage And Research Institute. A total of 30 patients were studied during this period, out of which 22 were females and 8 were males.INCLUSION CRITERIA:Ÿ Patients presenting with auricular keloidŸ Patients who are willing to give consent.Ÿ Patients within age group of 18 to 60 years.EXCLUSION CRITERIA:Ÿ Patients under the age of 18 yearsŸ Revision casePatients with auricular keloids attending out-patient department requiring surgery underwent routine blood investigations and after obtaining fitness for surgery were selected for the proposed procedure. Patients were operated under local anesthesia using scar based flap technique. Local infiltration was given with 2% lignocaine and the overlying skin was elevated from the keloid matrix. Dissection was carried out till the edges of the keloid and the exposed keloid matrix was shaved, leaving behind the healthy cartilage. The redundant skin was trimmed, placed over the freshened cartilage and the margins were sutured with 5-0 monocryl or prolene to create a smooth and continuous contour. Mastoid dressing was applied to prevent post-operative hematoma and removed after 24 hours. Sutures were removed after 5 days. Following suture removal, the patients were advised to apply a pressure dressing with soft rubber/ silicone sheet for 2 weeks at night.
 | Figure 1. Auricular keloid: preoperative |
 | Figure 2. Following the skin flap elevation |
 | Figure 3. Excision of keloid matrix |
 | Figure 4. Exposing freshened cartilage |
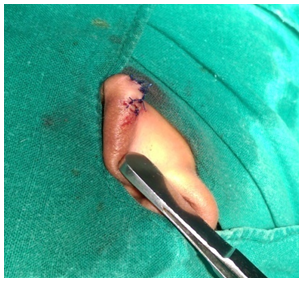 | Figure 5. Following skin flap suturing |
 | Figure 6. Maintenance of normal contour |
4. Results
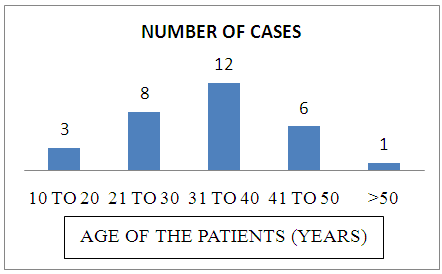 | Graph 1. Age distribution of study population |
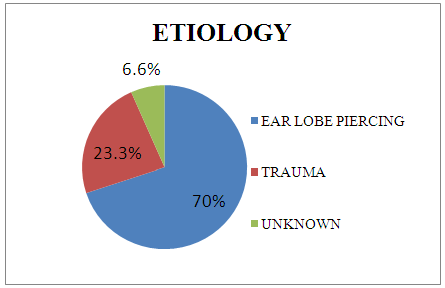 | Graph 2. Etiology of auricular keloids |
5. Discussion
- Several factors that are beyond the surgeon’s control can affect the final appearance of the scar like mechanism of injury, position of the wound, health status of the patient, patient’s skin type and tendency to form robust scars. Factors that are under the surgeon’s control include proper realignment of wound edges, conservative debridement of injured tissues, meticulous handling of tissues during primary repair and aesthetically favorable alignment of scars whenever possible. [2]After complete maturation and healing, an ideal scar should be1. Flat and level with the surrounding skin2. Good color match with the surrounding skin3. Narrow, parallel to the relaxed skin tension lines 4. On the border of aesthetic facial subunits 5. Without straight unbroken lines that can be easily followed with the eye. [1]Multiple modalities of treatment options are available for treating auricular keloid including cold excision, laser excision, intralesional steroids, radiation and combinations of these modalities. A topical application of silicone sheet to the surface of keloid has been shown to be beneficial in the management of these lesions. It causes an increase in scar hydration by more than 50 percent and reduction in evaporation leading to decrease in capillary activity and subsequent collagen deposition. Pressure therapy is a conservative mode of treatment which causes thinning of the dermis, a decrease in edema, and reduction of blood flow producing a hypoxic environment and as a result causes decrease in collagen synthesis. Studies on the use of steroids alone to treat keloids have shown response rates of 30–100 percent [3]. Surgery alone has a recurrence rate in the range of 54–93 percent [3-5]. Combined treatment modalities showed better results compared to single modality. In a prospective study done by W Y Myron on 6 patients who underwent a combined approach using CO2 laser for excision followed by postoperative steroid injections showed good cosmetic results with no recurrence. When postoperative radiation is combined with surgical excision the response rates have been reported to be 33–100 percent [6]. Study by Stahl S et al included 23 patients with auricular keloids who were treated using sandwich technique protocol: extralesional excision and external beam radiotherapy were given a day before and a day after the operation. The results were satisfactory with low recurrence and complication rates [7]. The combination of surgery followed by regularly scheduled postoperative intralesional steroid injections is regarded by many as the current standard of care for the majority of keloids seen in clinical practice. Best results were seen in those cases where steroids were administered at the time of excision and at repeated postoperative visits.Akoz T et al did a prospective study on 12 patients who were treated with a combined approach of excision, early postoperative steroid injection, and pressure applied by an earring covered with a silicone gel sheet. The results showed almost 90% success rate without any side effects [8].In our study of 30 patients with scar based flap excision, 22 were females and 8 were males. Patient’s average age was 33years. The most common etiology of keloid was ear piercing. Out of 30 cases only 2 patients showed recurrence at 6 months and 1 patient at one year follow up, which was treated conservatively with intralesional steroid injection. Partial flap necrosis was seen in three cases where the keloid was larger in size, this could be attributed to larger skin flap and inadequate vascularity. The overall patient satisfaction was high as the aesthesis of the pinna was well preserved.
6. Conclusions
- In conclusion, the scar based skin flap technique followed by postoperative intralesional steroid therapy can be used very effectively in the management of auricular keloids with a low complication rate and better cosmetic results. Although the follow up period was one year, the recurrence rate was found to be low. Avoidance of tension, accurate approximation of wound margins and good vascularity, were the important factors in reducing the recurrence rate of auricular keloid following surgical excision. Good cosmesis and maintenance of contour were the added advantages. However follow up for a longer period is recommended to assess the long term recurrence rate.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML