B. Ramya , Borlingegowda Viswanatha , Maliyappanahalli Siddappa Vijayashree , Aparna Mohan
Otorhinolaryngology Department, Bangalore Medical College & Research Institute, Bangalore, India
Correspondence to: Borlingegowda Viswanatha , Otorhinolaryngology Department, Bangalore Medical College & Research Institute, Bangalore, India.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Aim: To assess the quality of life after adenotonsillectomy in pediatric population. Materials and Methods: 100 children who underwent adenotonsillectomy between Jan 2010 to Dec 2011 were included in the study. Parents were made to fill pre and post operative questionnaires one day prior to the surgery and 6 months after the surgery respectively, which included 3 of the 6 features of Tonsil and adenoid health status instrument (TAHSI) scoring system and the results were tabulated and analyzed. Results and Conclusions: There was a statistically significant reduction in the total symptom score of children post adenotonsillectomy in terms of recurrent tonsillitis, airway/sleep and eating/swallowing disturbances. Thus breaking the myth and implying that adenotonsillectomy has a positive impact on the quality of life of children if operated for definitive indications.
Keywords:
Adenotonsillectomy, Quality of life, Sleep disordered breathing
Cite this paper: B. Ramya , Borlingegowda Viswanatha , Maliyappanahalli Siddappa Vijayashree , Aparna Mohan , Quality of Life Post Adenotonsillectomy in Children with Adenotonsillar Hypertrophy: A Prospective Study, Research in Otolaryngology, Vol. 5 No. 2, 2016, pp. 32-38. doi: 10.5923/j.otolaryn.20160502.03.
1. Introduction
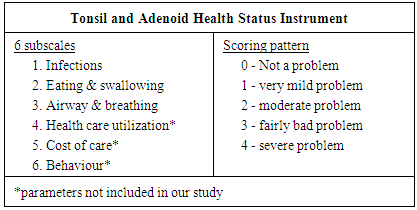
Tonsils and adenoid form a part of the Waldeyer’s ring with lingual tonsils, lateral pharyngeal bands and tubal tonsils forming the other components. They act as first line of defence to the aerodigestive system forming a part of the Nasal associated lymphoid tissue (NALT)/ mucosa associated lymphoid tissue (MALT) [1]. They sample bacteria and viruses, release Ig (esp IgA) producing B cells and bring about antigenic/ non antigenic reaction thus participating in cellular and humoral immunity. Over years controversy exists as to the effect of removing tonsils and adenoid in children as they form an important part of the immune system implicating their removal only when the benefits of alleviating the preoperative morbidity outweigh the risks of surgery and the loss of the first line of defence of the aerodigestive system [2]. But it is found that in long term, adenotonsillectomy only removes the nidus for stimulated cellular and humoral immunity seen in tonsillitis, without any effect on the patients normal immune function [3, 4, 5]. The quality of life (QoL) of patients with chronic tonsillitis is multidimensional with the outcome of the surgical intervention forming the main factor associated with the change of quality of life QoL [6]. In children aged 2-16 years with tonsil and adenoid disease, - Tonsil and adenoid health status instrument (TAHSI) is a validated questionnaire for disease specific QoL measurement [6]. Other measures for quality of life include SF-12, with physical and mental subscales forming a validated global QOL instrument for adults [6], Glasgow Benefit Inventory (GBI) Questionnaire for retrospective study after surgery and the Child Health Questionaire-PF28 (CHQ-PF28) which includes physical functioning, parental impact, general health perceptions, family activities, behavior and bodily pain [7].This study aims to assess the quality of life in terms of recurrent tonsillitis requiring antibiotics, sleep/airway disturbances and eating/swallowing disturbances before and after adenotonsillectomy using a modified TAHSI questionnaire in pediatric population.
2. Material and Methods
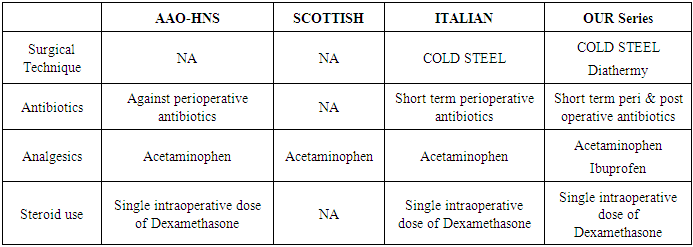
This is a prospective observational study where a total of 100 children between 4 -14 years of age who underwent adenotonsillectomy from Jan 2010 to Dec 2011 by the conventional dissection and snare method were included in the study. Among indications for adenotonsillectomy were included adenotonsillar hypertrophy with obstructive symptoms and recurrent adenotonsillitis. Children who underwent isolated adenoidectomy, isolated tonsillectomy and Adenotonsillectomy with nasal surgeries were excluded from the study. Questionnaires enquiring about the complaints of children, their severity and their effect on the health and quality of life were filled by parents both pre operatively one day prior to surgery and post operatively 6 months after surgery. The results were tabulated based on the TAHSI scoring system omitting parameters which were not feasible to assess in our study. Table 1 shows the TAHSI scoring system.Table 1. Showing the TAHSI components and scoring system
 |
| |
|
3. Statistical Analysis
The data was entered in Microsoft Excel Workbook and was analysed in “SPSS 10 for Windows (Statistical Packages for Social Sciences 19.0 version)” software.Chi-square test was performed to compare the significant association between categorical variables and p value < 0.05 was taken as statistically significant.
4. Results
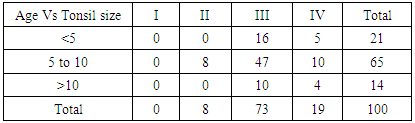
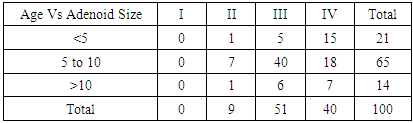
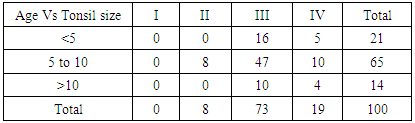
Out of the 100 children in the study 60 were male and 40 were female. Majorities i.e., 65% of these children were in the age group of 5-10 years. Tables 2 & 3 shows the tonsil and adenoid sizes seen in children of different age groups with grade-III tonsils seen in 73% of children and grade III & 1V adenoids seen in 51% & 40% of children respectively.Table 2. Showing tonsil size in children of different age groups
 |
| |
|
Table 3. Showing adenoid size in children of different age groups
 |
| |
|
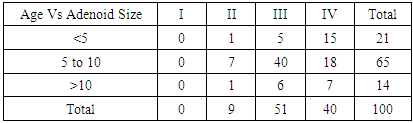
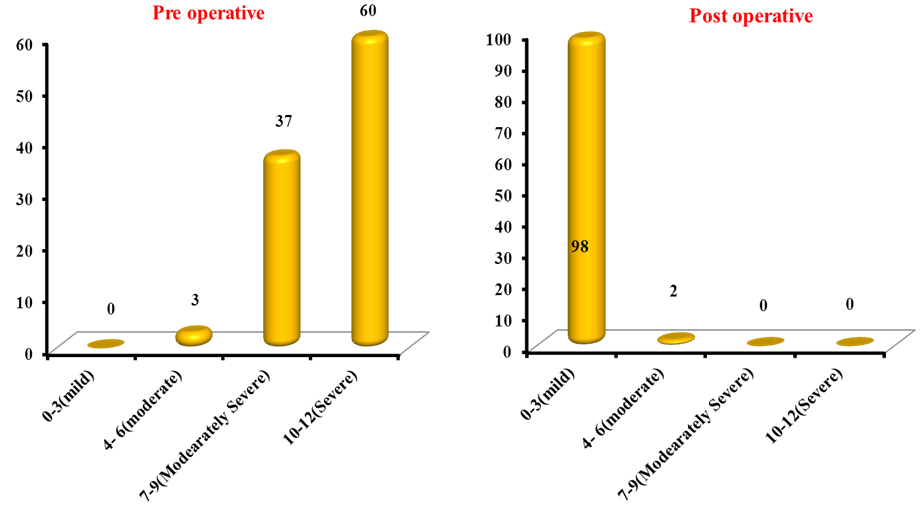
Graph 1 shows the pre and post operative total symptom scores with respect to recurrent sore throat, sleep disturbance and swallowing problems. Pre operatively 37% & 60% of children had scores 7-9 & 10-12 belonging to the moderately severe and severe group respectively with 98% of children having scores of only 0-3 post operatively and hence falling into the mild group indicating a successful outcome.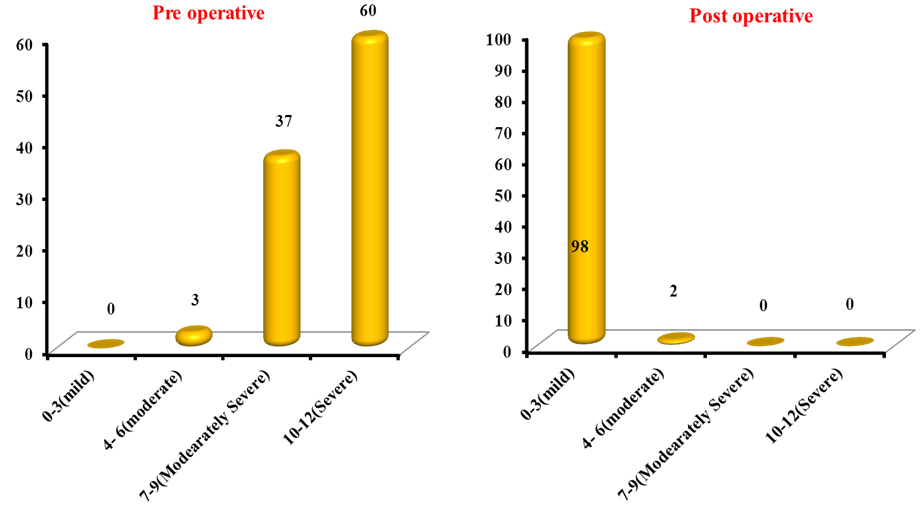 | Graph 1. Showing Total Symptom Score pre and post operatively |
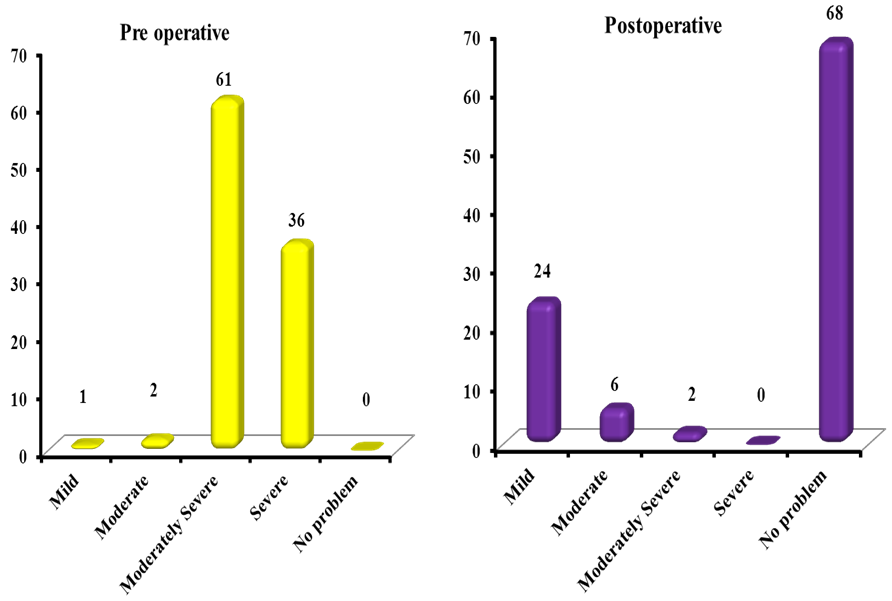
Patients had significant improvement in terms of recurrent sore throat. Pre & post operative symptom score for recurrent sore throat is shown in chart 2.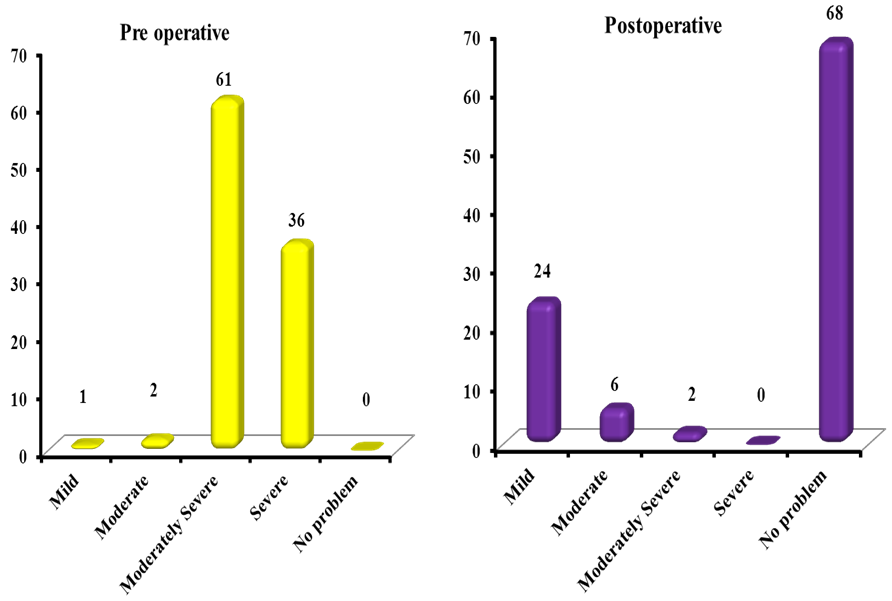 | Chart 2. Showing pre & post operative symptom score for recurrent sore throat |
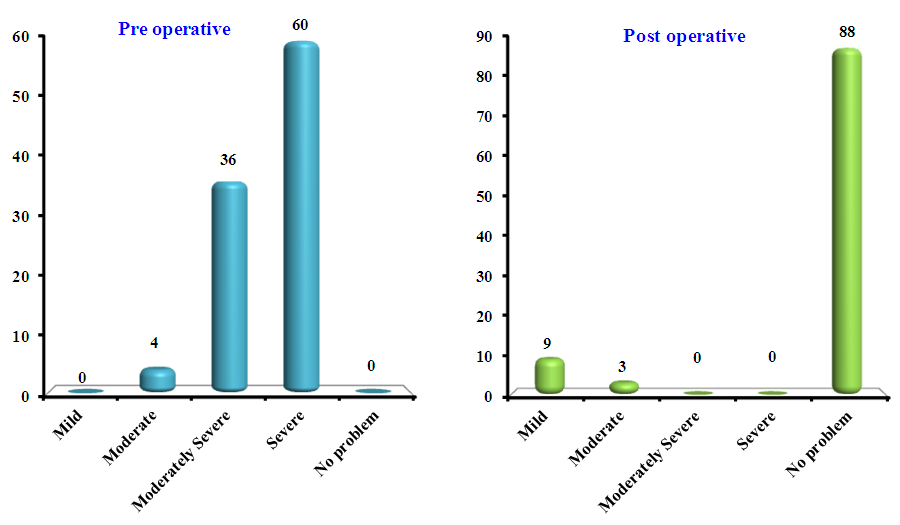
Patients had significant improvement in sleep disturbance. Pre & post operative symptom score for sleep disturbance is shown in chart 3.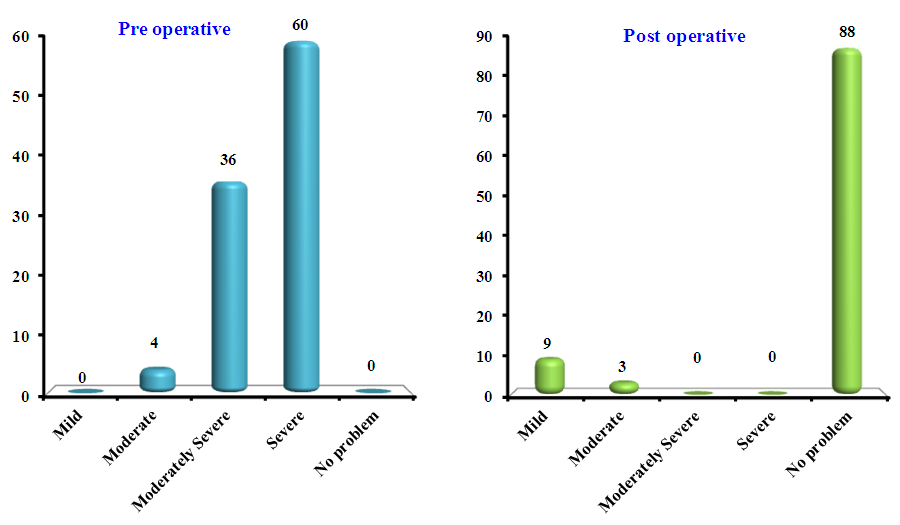 | Chart 3. Showing pre & post operative symptom score for sleep disturbance |
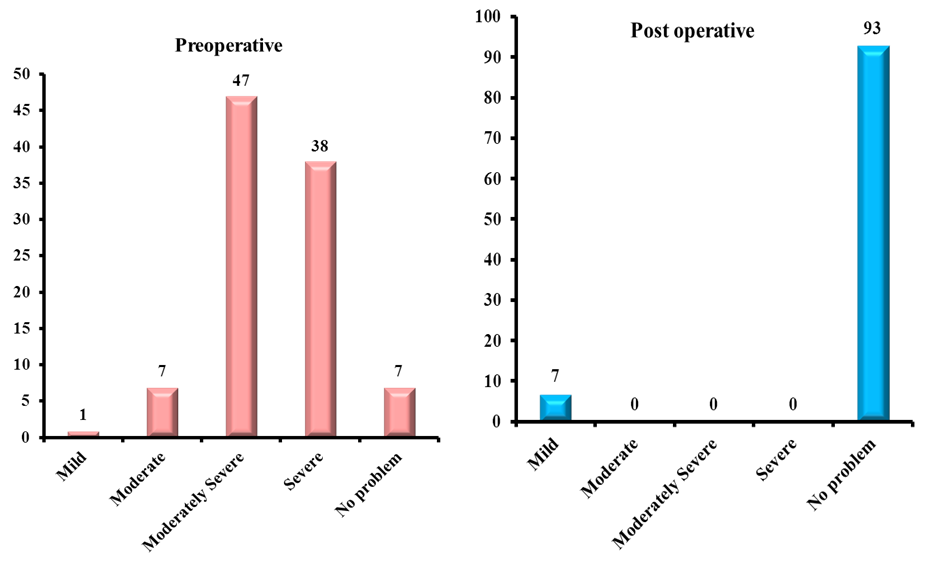
Patients had significant improvement in swallowing disturbance. Pre & post operative symptom score for swallowing disturbance is shown in chart 4.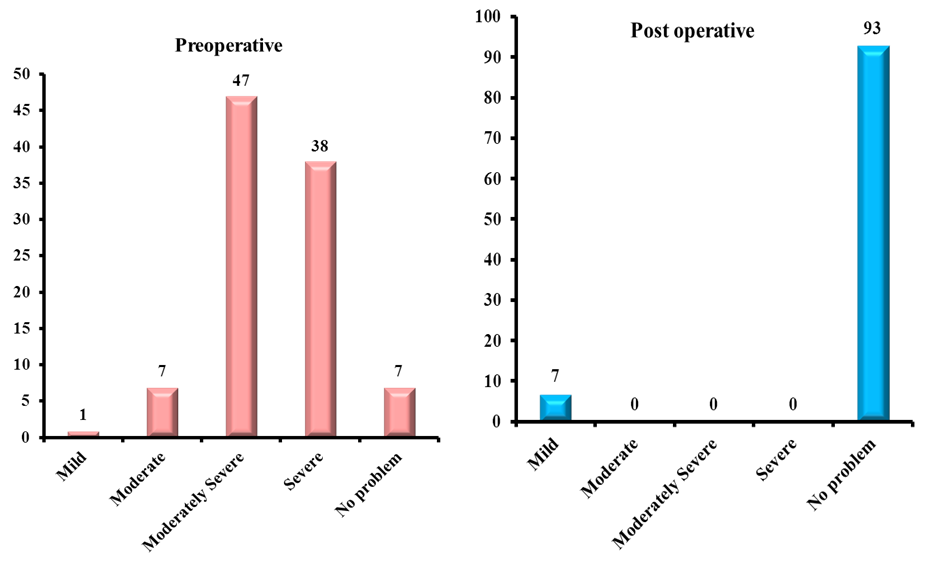 | Chart 4. Showing pre & post operative symptom score for swallowing disturbance |
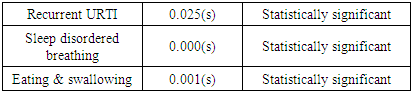
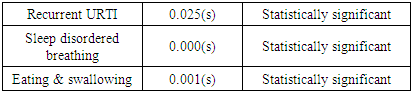
Table 4 shows the ‘p’ value for the 3 main parameters studied namely recurrent sore throat, sleep and swallowing disturbances which were found to be statistically significant.Table 4. Showing statistical significance of the 3 parameters studied
 |
| |
|
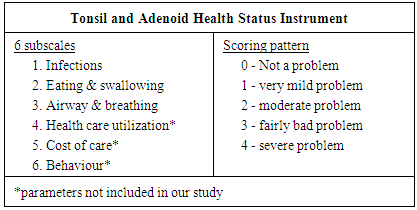
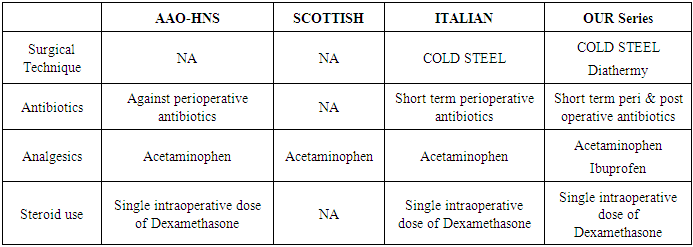
Table 5 shows the comparison of the practice protocol of AAO-HNS, Scottish and Italian otolaryngologists academy with the protocol followed in our institution study.Table 5. Showing the comparison of our practice protocol with others
 |
| |
|
Primary Haemorrhage (in theatre) was encountered in 8% of cases which was effectively controlled by electrocautery and nasal packing. Reactionary (within 24 hours of surgery) Haemorrhage was seen in 1 patient who was taken back to theatre and posterior nasal packing was done as it was secondary to adenoidectomy while fortunately no cases of secondary haemorrhage (after 48hours of surgery) were encountered. There were no cases requiring re-exploration / re-admission.
5. Discussion
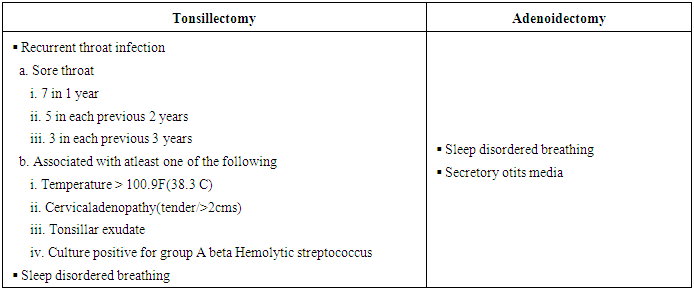
Tonsils and adenoid form a part of the Waldeyer’s ring and Nasal associated lymphoid tissue NALT/ mucosa associated lymphoid tissue MALT1 thereby acting as 1st line of defense to the aerodigestive system. They play a role in both cell mediated and humoral immunity [3]. Tonsillitis could present as acute, chronic, recurrent or obstructive type caused by bacteria like GABHS( Group A beta hemolytic streptococci)-most common, H.influenza, M.catarrali, staphylococcus aureus or viruses more commonly seen in younger children [8] like echovirus, RSV, infuenza A&B, adenovirus and EB virus. Though adenotonsillectomy is one of the most common surgeries performed in children [9] initially the medical line of management is started which includes analgesics for the initial 3 days followed by antibiotics like penicillin, amox-clav, cephalosporins or macrolides if symptoms persist. Surgical removal is done based on the AAP (American Academy of Paediatrics) guidelines for the indications of adenotonsillectomy depicted in table 6. Though various surgical tools are being used apart from the cold steel like laser, cryosurgery, harmonic scalpel, raiofrequency with coblator being the latest and widely used tool, the surgical method remains the same. The post operative morbidity and quality of life depends on multiple factors like indications of surgery, surgical technique, surgical complications and post operative care with children generally facing lesser morbidity [10]. In the post operative period most surgeons use broad spectrum antibiotics which cover beta lactamase producing organisms but the role of prophylactic antibiotics postoperatively and the type of antibiotic to be used needs thorough investigation.Table 6. Showing AAP indications for adenotonsillectomy
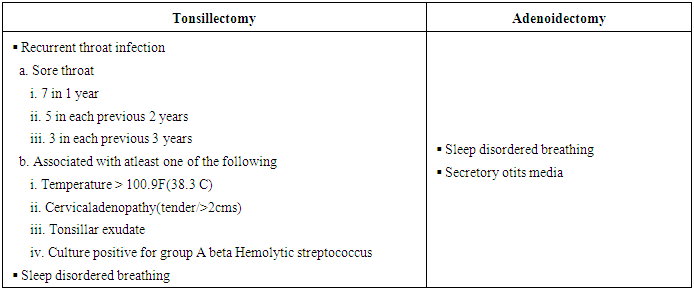 |
| |
|
The usefulness of surgery is assessed by its effectiveness in reducing the pre operative symptoms [2] as opposed to its risks and thus improving the quality of life. To measure the quality of life post operatively many health status instruments are available which include a variety of parameters. The Tonsil and Adenoid Health Status Instrument with 6 distinct subscales- eating and swallowing, airway and breathing, infections, health care utilization, cost of care, and behavior is a valid, reliable, and sensitive instrument for outcomes research in children with tonsil and adenoid disease [11, 7]. The CHQ-PF28 scored 0-100 contains 12 subscales like physical functioning, emotional/ behavioral problems, physical problems, bodily pain/ discomfort, behavior, mental health, self-esteem, general health perceptions, parental impact on time and emotions, family activities, and family cohesion [7].In a study by Colreavy et al [12] it was found that H Influenza, Streptococcus viridans and Staphylococcus aureus were the most common organisms found in the core tonsillar tissue and postoperative morbidity in terms of amount of analgesia consumed, normal diet resumption time and pain analogue scores could be significantly reduced with Amoxycillin and clavulanic acid given for a week post operatively [12]. In an Open, randomised controlled trial where 300 children between 2-8 years of age with symptoms of adenotonsillar hypertrophy /infection were divided into two groups ,one with adenotonsillectomy and the other with watchful waiting it was found that adenotonsillectomy could be considered an indication for surgery for children with three to six episodes of throat infection in a year and not in children with with mild symptoms of adenotonsillar hypertrophy or infection as the surgical benefit did not outweigh the effects of watchful waiting in mild cases [13].In an uncontrolled observational prospective study by Nira et al [7] where disease specific and global quality of life of 92 children who underwent adenotonsillectomy were studied with 6months and 1year follow-up of 58 & 38 children respectively using the TAHSI and CHQ-PF28 scoring system it was found that all parameters studied showed improvement which was statistically significant. Though initially aimed to be a controlled study comparing medical & surgical line of treatment for adenotonsillitis due to inadequate control group, selection bias and parental belief that surgery is needed it was converted to an uncontrolled observational study. This study lacked a control group but in view of the consistent and large changes in parameters studied the positive results cannot be ignored.In a hospital-based prospective study by Afolabi et al [2] the most common indication for adenotonsillectomy was obstructive symptoms and the reduction in pre operative symptoms recorded were from 93.1% pre op to 10.3% post op for recurrent sore throat, from 100 to 13.8% for sleep disordered breathing and from 79.3% to 13.8% for eating & swallowing disturbances which is similar to our results of reduction from 100% to 32% for recurrent sore throat, from 100% to 12% for sleep disturbances and from 93% to 7% for eating/swallowing disturbances. This study stressed the importance of parental satisfaction and that parents often expected improvement in quality of life of the child as a whole rather than just reduction in a particular symptom which formed the indication for the surgery. In a prospective study by Carneiro et al [14] it was observed that parental satisfaction was significant for snoring, recurrent tonsillitis and use of antibiotics post adenotonsillectomy similar to our study. However rhinitis did not show significant improvement post operatively. Our study showed a statistically significant improvement in the pre operative symptoms similar to other studies [2, 14, 15] based on parental satisfaction using questionnaires on parameters pertaining to quality of life before and after surgery [2]. This study included parameters which are commonly used by otolaryngologists as criteria for surgery though not very severe but affecting the quality of life, making it clinically more significant [7]. Though adenotonsillectomy is documented to reduce the number of episodes of sore throat due to any cause like pharyngitis etc [16], in our study only children with documented recurrent episodes of adenotonsillitis by otolaryngologist in our hospital or elsewhere were included excluding bias involving other causes of sore throat [7]. In this study only children with both pre operative and 6 months post operative filled questionnaires were included in the study making room for bias due to patients lost on follow up. The results of our study help in reassuring parents, especially the urban population about the usefulness of adenotonsillectomy and in removing the widely accepted myth of immunity being compromised life long by the surgery [5]. However a multicenter study with larger sample size and assessing more number of parameters is warranted.
6. Conclusions
Adenotonsillectomy has a positive impact on the quality of life of children like reduction in episodes of sore throat, difficulty in swallowing and sleep disturbances, if operated for definitive indications. Indications based on quality of life are more valuable than culture documented infections of adenotonsils. However more studies on quality of life with larger study groups and randomization is warranted with questionnaires prepared suiting Indian population and facilities as the Standardized international questionnaires available are not very suitable in the Indian scenario.
References
| [1] | Hellings P, JorissenM, Ceuppens JL. The Waldeyer's ring. Actaotorhinolaryngol belq 2000; 54(3): 237-241. |
| [2] | Afolabi OA, Alabi BS, Ologe FE, Dunmade AD, Segun- Busari S. Parental satisfaction with post-adenotonsillectomy in the developing world. Int J Pediatr Otorhinolaryngol 2009; 73: 1516–1519. |
| [3] | Kaygusuz I, Gödekmerdan A, Karlidaˇg T et al.. Early stage impacts of tonsillectomy on immune functions of children. Int J Pediatr Otorhinolaryngol 2003; 67: 1311-1315. |
| [4] | Zielnik-Jurkiewicz B, Jurkiewicz D.. Implication of immunological abnormalities after adenotonsillotomy. Int J Pediatr Otorhinolaryngol 2002 Jun 17; 64(2): 127-132. |
| [5] | Kaygusuz I, Alpay HC, Gödekmerdan A, Karlidag T et al. Evaluation of long-term impacts of tonsillectomy on immune functions of children: A follow-up study. Int J Pediatr Otorhinolaryngol March 2009; 73(3): 445-449. |
| [6] | Skevas T, Klingmann C, Sertel S, Plinkert PK, Baumann I. Measuring quality of life in adult patients with chronic tonsillitis. The Open Otorhinolaryngology Journal 2010; 4: 34-46. |
| [7] | Goldstein NA, Stewart MG, Witsell DL, Hannley MT, Weaver EM et al. Quality of life after tonsillectomy in children with recurrent tonsillitis. Otolaryngol Head Neck Surg 2008; 138: S9-S16. |
| [8] | Douglas RM, Miles H, Hansman D, Fadejevs A, Moore B, Bollen MD. Acute tonsillitis in children: microbial pathogens in relation to age. Pathology 1984 Jan; 16(1): 79-82. |
| [9] | Craig S Derkay , Paediatric otolaryngology procedures in the United States: 1977–1987, Int. J. Pediatr. Otorhinolaryngol. Jan 1993, Vol 25, issues 1-3, pages 1–12. |
| [10] | Piltcher OB, Scarton FB. Antibiotic use in tonsillectomies: therapeutic or prophylactic? Required or excessive? Rev Bras Otorrinolaringol.2005; 71(5): 686-690. |
| [11] | Stewart MG, Friedman EM, Sulek M, deJong A, Hulka GF, Bautista MH, Anderson SE. Validation of an outcomes instrument for tonsil and adenoid disease. Arch otolaryngol head neck surg 2001 Jan; 127(1): 29-35. |
| [12] | Colreavy MP, Nanan D, Benamer M, Donnelly M, Blaney AW et al. Antibiotic prophylaxis post-tonsillectomy: is it of benefit?. Int J Pediatr Otorhinolaryngol Oct 1999; 50(1): 15-22. |
| [13] | Staaij BK, Akker EH, Rovers MM, Hordijk GJ et al. Effectiveness of adenotonsillectomy in children with mild symptoms of throat infections or adenotonsillar hypertrophy: open, randomised controlled trial. BMJ, doi:10.1136/bmj.38210.827917.7C (published 10 September 2004). |
| [14] | Carneiro LEP, Neto GCR, Camera MG. Adenotonsillectomy Effect on the Life Quality of Children with Adenotonsillar Hyperplasia. Int.Arch.Otorhinolaryngol 2009; 13(3): 270-276. |
| [15] | Blair RL, McKerrow WS, Carter NW, Fenton A, The Scottish tonsillectomy audit. The Audit Sub-Committee of the Scottish Otolaryngological Society, J Laryngol. Otol. 20 (1996) 1–25. |
| [16] | Blakley BW, Magit AE. The role of tonsillectomy in reducing recurrent pharyngitis: a systematic review. Otolaryngol Head Neck Surg. 2009; 140:291-297. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML