-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2016; 5(1): 16-19
doi:10.5923/j.otolaryn.20160501.03

Pleomorphic Adenoma of the Palate: Presentations and Management
Sanwar Mal Bajia , Trisha Srivastava , Borlingegowda Viswanatha , Roopashri Tarikere Jayaram , Maliyappanahalli Siddappa Vijayashree , Shashikala Ballur Srinivasan
Otorhinolaryngology Department, Bangalore Medical College & Research Institute, Bangalore, India
Correspondence to: Borlingegowda Viswanatha , Otorhinolaryngology Department, Bangalore Medical College & Research Institute, Bangalore, India.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Pleomorphic adenoma is a benign mixed tumour composed of various morphological patterns of epithelial and myoepithelial cells component, demarcated from surrounding tissues by fibrous capsule. We report 3 cases of pleomorphic adenoma of the minor salivary gland of the palate.
Keywords: Pleomorphic adenoma, Palate
Cite this paper: Sanwar Mal Bajia , Trisha Srivastava , Borlingegowda Viswanatha , Roopashri Tarikere Jayaram , Maliyappanahalli Siddappa Vijayashree , Shashikala Ballur Srinivasan , Pleomorphic Adenoma of the Palate: Presentations and Management, Research in Otolaryngology, Vol. 5 No. 1, 2016, pp. 16-19. doi: 10.5923/j.otolaryn.20160501.03.
Article Outline
1. Introduction
- Pleomorphic adenoma (PA) is the most common tumour (60%) of major and minor salivary glands; nearly 70% of the tumours of minor salivary glands are PA. The mean age at presentation of patients with pleomorphic adenomas between 40 to 50 years, but they can develop at any time of life. Overall, there is a slight female predominance (1.4:1). The importance of lesions lies in the fact that when associated with minor salivary glands they are more likely to be malignant (50%) [1, 2].
2. Case Reports
2.1. Case 1
- A 45-year-old female presented with a slow growing swelling, for duration of 20 years involving her hard and soft palate on the left side. The lesion was asymptomatic, with no associated pain or paresthesia. She had no complaints of pharyngeal or airway obstruction. The patient presented a typical ‘hot potato in mouth’ speech.The clinical examination revealed nonulcerated, dome-shaped, palatal swelling on the left side involving the hard and soft palate, crossing the midline. The mass had a bosselated surface and overlying mucosa was cherry red and stretched. The lesion was multinodular, firm, and nontender on palpation (Figure 1).
 | Figure 1. Photograph showing swelling over the left side of the palate |
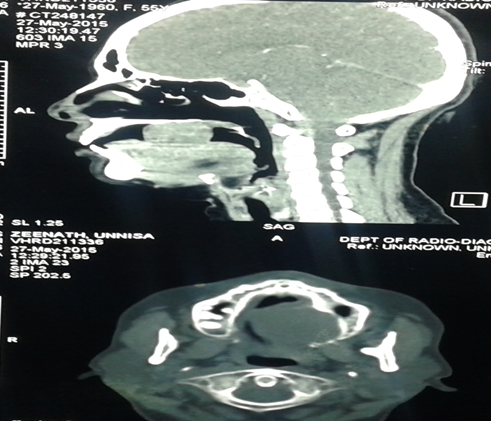 | Figure 2. CT scan saggital and axial cuts showing the mass |
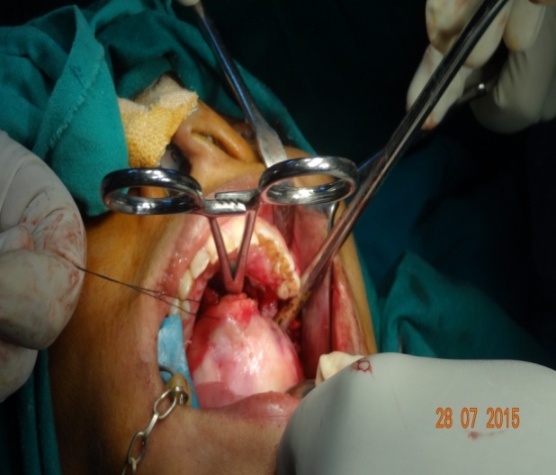 | Figure 3. Intra operative picture showing the mass |
 | Figure 4. Photograph showing excised mass |
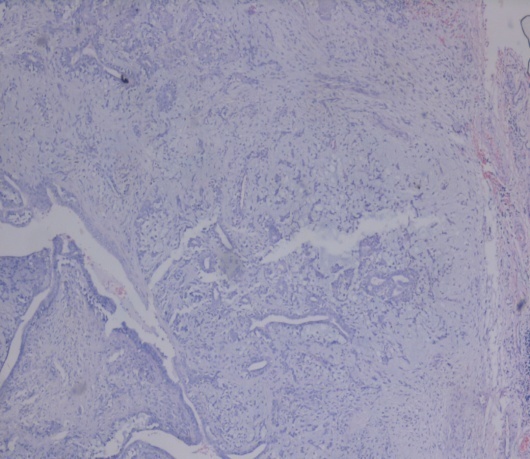 | Figure 5. Microphotograph showing cells arranged in sheets and duct-like pattern with a mucoid background |
2.2. Case 2
- A 37 year old male presented with slow growing palatal swelling for the past 14 years at the junction of soft and hard palate on the left side. The lesion was associated with pain. There was no associated paresthesia with the swelling. He had no complaints of pharyngeal or airway obstruction. The patient presented a typical ‘hot potato in mouth’ speech.Clinical examination revealed ulcerated, dome-shaped, palatal swelling on the left side involving the hard and soft palate, crossing the midline. The mass had bosselated surface and overlying mucosa was ulcerated. The lesion was multinodular, firm, and nontender on palpation (Figure 6). The patient was subjected to Computed tomography (CT) scan and FNAC.CT showed a well-circumscribed mass measuring 5.2X3.6X4.1 noted in the oral cavity. There was no erosion of the underlying bone. FNAC showed benign mixed tumor composed of epithelial and myoepithelial cells arranged with various morphological patterns, demarcated from surrounding tissues by fibrous capsule suggestive of pleomorphic adenoma of minor salivary gland of the palate.
 | Figure 6. Photograph showing the swelling over the palate |
 | Figure 7. Intra operative picture showing the palate after mass excision |
 | Figure 8. Photograph showing excised mass |
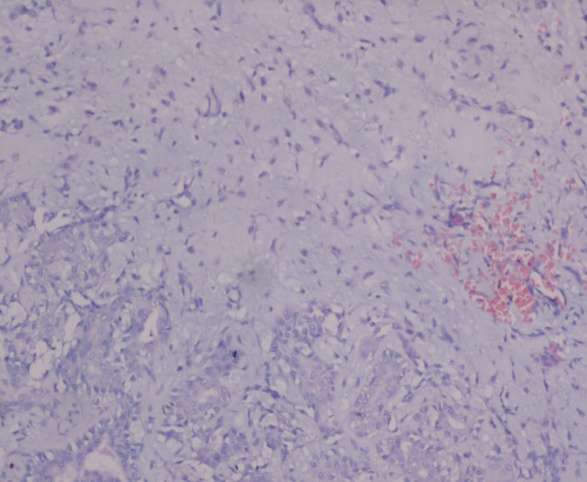 | Figure 9. Microphotograph showing salivary acini lined by ductal epithelial and myoepithal cells in a background of chondromyxoid stroma |
2.3. Case 3
- Female aged 24 years presented with a swelling of the palate for duration of 3 years. The swelling was insidious in onset and gradually progressed to present size. Oral cavity examination showed 3cm x2 cm swelling at the junction of the hard and soft palate on the right side. There was no pain. On palpation the swelling was firm in consistency with no tenderness. The mucosa over the swelling was normal (Figure 10). The patient was subjected to CT scan, which showed a well circumscribed lesion on the palate with no erosion of underlying bone. FNAC revealed myxoid stroma and spindle cells were seen embedded in stromal matrix and cells were also seen in cohesive clusters. All these features were suggestive of pleomorphic adenoma. Routine investigation results were within normal limits. Wide excision of the mass was done with removal of the underlying periosteium under general anaesthesia. The wound was closed in layers.
 | Figure 10. Intraoperative picture showing the swelling over the palate |
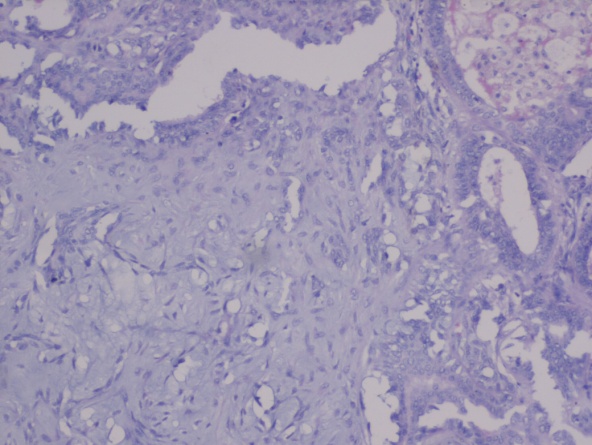 | Figure 11. Microphotograph showing epithelial and myoepithelial cells |
3. Discussion
- Salivary gland neoplasms are rare, comprising of 1- 4% of all neoplasm and 3-5%of all head and neck neoplasm.11% of tumour bulk found in minor salivary glands with incidence ranging from 33% to 70 %.Most studies have shown minor salivary gland tumours are more common in females. Most common in 4th-6th decade [1-3].In the minor glands, the majority of pleomorphic adenomas are found in the palate (42.8-68.8%), the next most common sites are the lips (10.1%) and the cheeks (5.5%). They are also occasionally found at other sites such as the tongue, retromolar fossa, pharynx or tonsil [1-3]. These tumours are exceedingly rare in the sublingual glands, but occasionally found at sites in the airways that extend from the nasal cavity to the bronchi, the middle ear and external auditory meatus and in the lacrimal glands. Tumours develop in an insidious fashion, growing slowly over a long period of time without causing any other symptom [3, 4]. Pain is extremely uncommon and, if present, usually heralds malignant change. The tumour is readily palpable, bosselated surface and bluish areas maybe discernable through the mucosa [5]. In addition, these tumours, like any others in the mouth and particularly those in the palate, can become ulcerated by friction or trauma. The firmness of these tumours varies with the nature and amount of the stromal component and thus ranges from soft, in the case of the more mucinous tumours, to hard in the case of tumours with an extensive chondroid or collagenous component [5, 6]. The differential diagnosis of PA cheek includes dermoid cyst, sebaceous cyst, neurofibromas, lipoma, mucoepidermoid carcinoma and polymorphous lowgrade adenocarcinoma [7].The main diagnostic modality are imaging and FNAC. CT or MRI scanning has to be done in cases of tumours having ill defined margins, to rule out suspected involvement of the nose or maxillary antra. FNAC may be a valuable pre-treatment diagnostic test. Its overall accuracy is greater than 96%, with sensitivity for benign tumours of 88-98% and a specificity of 94%. Frozen sections are 93% accurate when performed at surgery [3, 7, 8].A recurrence rate of 2 to 44% in the pleomorphic adenoma has been reported due to pseudopodia, capsular penetration, and tumour rupture with spillage of tumour cells are the most frequently encountered surgical issues. The treatment of choice for pleomorphic adenoma in minor salivary gland is wide local excision with the removal of periosteum or bone if they are involved. Simple enucleation of this tumour is believed to lead to high local recurrence rate and should be avoided [8, 9].
4. Conclusions
- Pleomorphic adenoma though being a common entity has to be dealt with utmost care when it is originating from minor salivary glands. One should be aware of the chances of recurrence and malignant potential of the tumour.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML