Syed Mohammed Shoib, B. Viswanatha
Otorhinolaryngology Department, Bangalore Medical College & Research Institute, Bangalore, India
Correspondence to: B. Viswanatha, Otorhinolaryngology Department, Bangalore Medical College & Research Institute, Bangalore, India.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Objectives: Sinusitis is one of the most common diseases of the nose and sinuses; it affects 1 in 7 adults. Nasal septum deviation is a common disorder that presents in up to 62% of the population, and its role in the pathogenesis of chronic sinusitis remains uncertain. This study was done to find the association between the presence of symptomatic septal deviation and rhinosinusitis.Methods: Totally 200 patients with chronic rhinosinusitis– persistent nasal symptoms (nasal congestion, discharge, postnasal drip, hyposmia or facial pain) of greater than twelve weeks duration that are refractory to medical treatment were analyzed over a period of 18 months between Oct 2013 to May 2015 in a tertiary care institute. All patients underwent otorhinolaryngology examination, digital radiograph of paranasal sinuses, and rigid nasal endoscopy under local anesthesia. In required patients CT scan of nose and paranasal sinuses was done. Patients who were above 15 years of age and below 60 years with symptoms of sinusitis with septal deviation, who agreed to participate in the study were selected to evaluate for the association & severity of sinusitis. Results: In our study 112 were males, 88 were females. C-shaped deviated nasal septum was commonest type found in our study (70.5%). The most common type of sinusitis was bilateral maxillary sinusitis (49%). Pansinusitis was seen in 5.5% of patients and it was seen only in patients with S-shaped deviated nasal septum.
Keywords:
Deviated nasal septum, Sinusitis
Cite this paper: Syed Mohammed Shoib, B. Viswanatha, Association between Symptomatic Deviated Nasal Septum and Sinusitis: A Prospective Study, Research in Otolaryngology, Vol. 5 No. 1, 2016, pp. 1-8. doi: 10.5923/j.otolaryn.20160501.01.
1. Introduction
Sinusitis is one of the most common diseases of the nose and paranasal sinuses. Sinusitis affects 1 in 7 adults resulting in about 50 million individuals diagnosed with sinusitis every year world over. More than 1 in 5 antibiotics prescribed in adults are for sinusitis, making it the fifth most common diagnosis for which antibiotics are prescribed [1].Chronic rhinosinusitis (CRS) is an extremely prevalent disorder affecting up to two percent of the world population, has a significant impact on the quality of life of affected individual [2]. The term ‘rhinosinusitis’ refers to a group of disorders characterized by inflammation of mucosa of nose and paranasal sinuses. CRS occurs when the duration of symptoms is greater than 12 weeks duration. Any anatomical, physiological or pathological features which in a way or other obstructs free drainage from the sinuses, permits the stasis of secretion and thus predisposes to infection. Many factors have been described as playing a role in the development of chronic sinusitis. These include allergy, asthma, dental disease, nasal polyps, immunodeficiency, mucociliary disorders, trauma, medications, surgery, noxious chemicals and micro-organisms (viral, bacterial and fungal), anatomic abnormalities such as a septal deviation, concha bullosa, septal spur or paradoxical turbinate [2].Nasal septal deviation is a common disorder that presents in up to 62% of the population, and its role in the pathogenesis of chronic sinusitis remains uncertain [3]. Nasal septal deviation may either cause osteomeatal obstruction or may interfere with proper airflow and results in sinusitis. The purpose of this study is to observe the correlation between deviated nasal septum (DNS) and CRS. Hippocrates in 5th century B.C stated that “In a person having a painful spot in head, with intense headaches, pus or fluid running from the nose removes the disease”, which may be referred to as describing sinusitis [4].Messerklinger studied mucociliary clearance of the sinuses. He observed that wherever two mucosal surfaces came into contact, localized disruption of mucociliary clearance occurred, causing retention of secretions in the area of contact and results in increased potential for infection. Anatomically, areas of mucosal contacts are mostly likely to occur in the narrow mucosal lined channels of the middle meatus and ethmoid air cell system [5]. Collet et al found no definite role of the nasal septum in the pathogenesis of chronic sinusitis nor as a contributing factor [6]. Harar et al found no significant difference between the chronic rhinosinusitis group and the control group with regards to septal deviation [7]. Rao et al used Mladina’s classification of 7 types of deviated nasal septum and concluded that disturbance to the area in the posterior flow(Type III-Type VI) played major role in sinonasal disease rather than obstruction in the nasal valve area (Type I and Type II) [8]. Smith et al, found no definitive relationship between septal deviation and development of maxillary sinusitis [9]. Gencer, et al suggested that maxillary sinus volumes tend to be higher at the contralateral side of the severe septal deviations. In addition, the chance of finding maxillary sinusitis on ipsilateral to the severe septum deviation was significantly increased [10]. Moorthy et al found that “S” shaped DNS showed statistically significant correlation with sinus disease even in absence of any nasal symptoms [11]. Rehman et al reported sinus pathology in majority of patients who had nasal septal deformity and obstruction [12]. Mohebbi et al. in their study ‘An epidemiologic study of factors associated with nasal septum deviation by computed tomography scan: a cross sectional study’ published in 2012 found no relationship between the severity of sinusitis, osteomeatal involvement and the degree of septal deviation [13].Objective of the study:To study the association and relationship of symptomatic deviated nasal septum with chronic rhinosinusitis.
2. Methods
This study entitled was conducted in department of ENT, Head & Neck surgery, from October 2013 to May 2015. Source of data: All the patients with symptomtomatic DNS and rhinosinusitis of more than 12 weeks duration are included in the study.Sample size: 200 patients Inclusion criteria:1. Patients >15 years and <60 years.2. Patients diagnosed as cases of rhinosinusitis based on TFR criteria.3. Patients with symptomatic deviated nasal septum.TFR CRITERIA [Lanza and Kennedy [14]]
 |
| |
|
The presence of two or more major factors, or one major and two minor factors, is considered suggestive of sinusitis.Methods of collection of data:The cases selected for the study were subjected to 1. Clinical examination.2. Diagnostic nasal endoscopy: 3. X-ray of nose and paranasal sinuses4. CT scan of nose and paranasal sinuses (in required cases) Statistical Methods: Descriptive and inferential statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean ± SD (Min-Max) and results on categorical measurements are presented in Number (%). Significance is assessed at 5% level of significance. Chi-square/ Fisher Exact test has been used to find the significance of study parameters on categorical scale between two or more groups.
3. Results
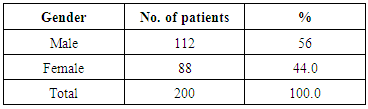
In the present study 112 were males (56%) and 88 were females (44%). Male to female ratio was 1.27: 1 [Table-1].Table 1. Showing sex distribution
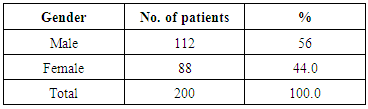 |
| |
|
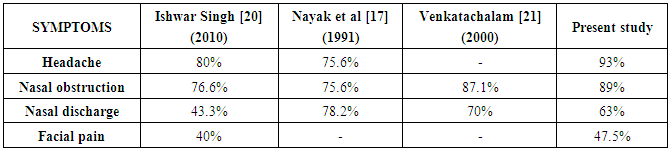
In this study 16 patients were in the age group of ≤20 yrs (8%), followed by 62 of them in age group of 21-30 years (31%) and 53 patients in age group of 31-40 years (26.5%), 51 patients were in 41-50 years (25.5%) and 18 patients in 51-60 years (9%) [Graph-1]. 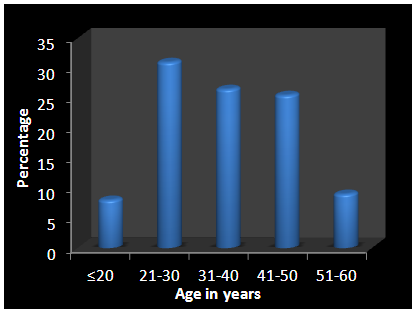 | Graph 1. Showing age distribution of patients studied |
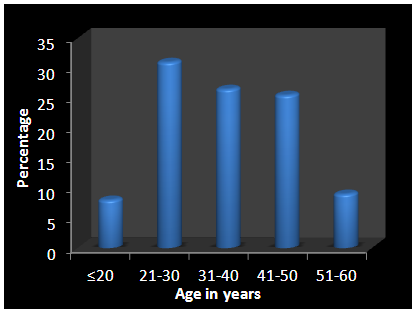
16 patients in group of ≤20 yrs included 10 males (8.9%) and 6 females (6.8%), followed by 62 of them in age group of 21-30 years included 36 males (32.1%) and 26 females (29.5%) and 53 patients in age group of 31-40 years included 30 males and 23 females, 51 patients were in 41-50 years included 26 males (23.2%) and 25 females (28.4%) and 18 patients in 51-60 years included 10 males (8.9%) and 8 females (9.1%). Youngest patient was 17 years and oldest patient was 60 years [Graph-2].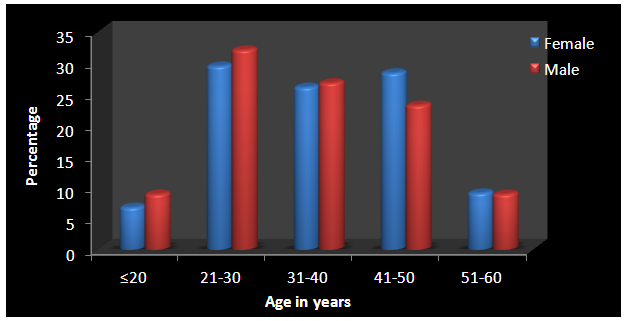 | Graph 2. Showing age distribution of patients studied in relation to sex |
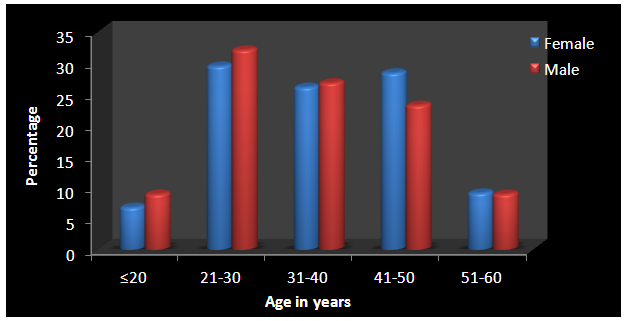
Headache is seen in 186 patients (93%), nasal obstruction seen in 178 patients (89%), nasal discharge in126 patients (63%), facial pain in 95 patients (47.5%), fever in 55 patients (27.5%), halitosis in 20 patients (10%), cough in 17 patients (8.5%), fatigue in 6 patients (3%) [Graph-3].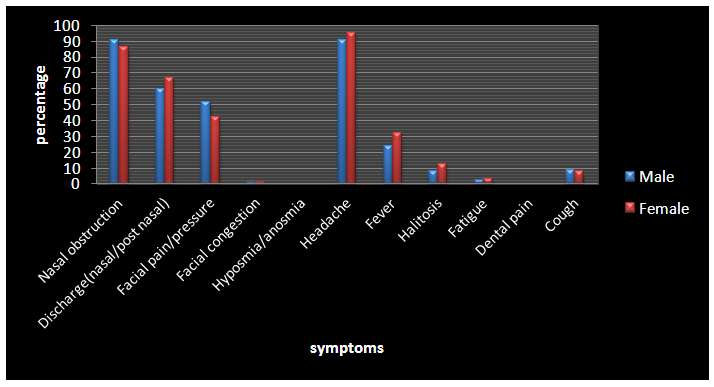 | Graph 3. Showing clinical features of patients studied |
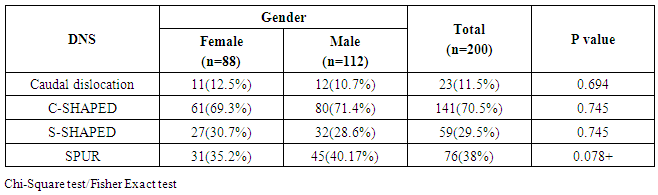
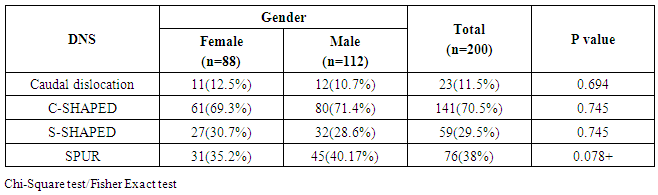
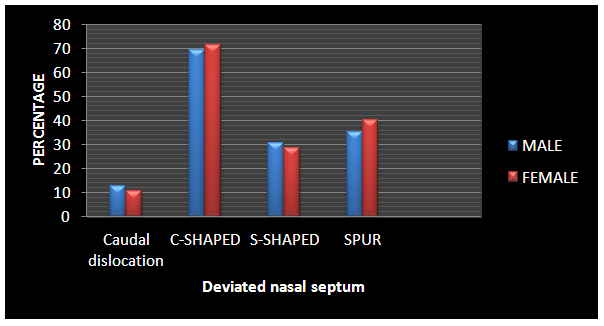
Caudal dislocation was seen in 23 patients (11.5%), C-shaped deviation was seen in 141 patients (70.5%), S-shaped deviation was seen in 59 patients (29.5%) and spur impinging on lateral wall in 76 patients (38%) [Table-2, Graph-4].Table 2. Showing types of deviations according to gender
 |
| |
|
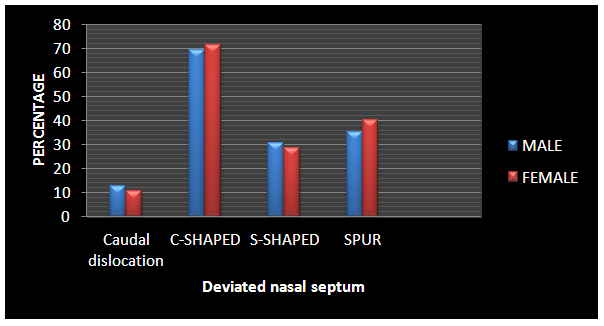 | Graph 4. Showing types of deviations according to gender |
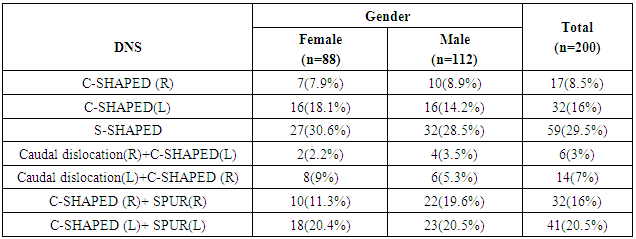
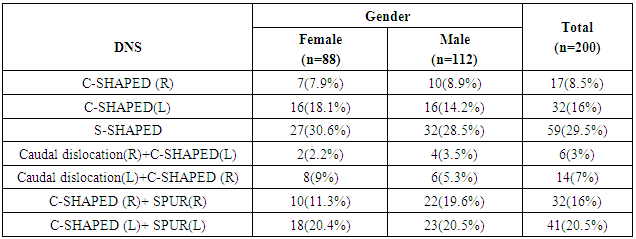
In our study patients presented with islolated C-Shaped deviation to left in 32 patients (16%) C-shaped deviation to right in 17 patients (8.5%), S-shaped deviation in 59 patients (29.5%), C-shaped deviation with spur to left in 41 patients (20.5%), C-shaped deviation with spur to right in 32 patients (16%), caudal dislocation to left with C-shaped deviation to right in 14 patients (7%), caudal dislocation to right with C-shaped to left in 6 patients(3%) [Table-3].Table 3. Distribution of presentation of DNS in relation to sex
 |
| |
|
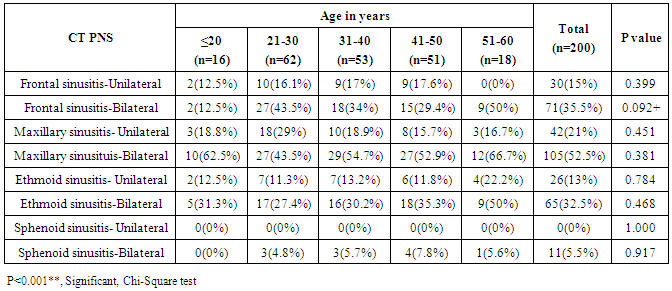
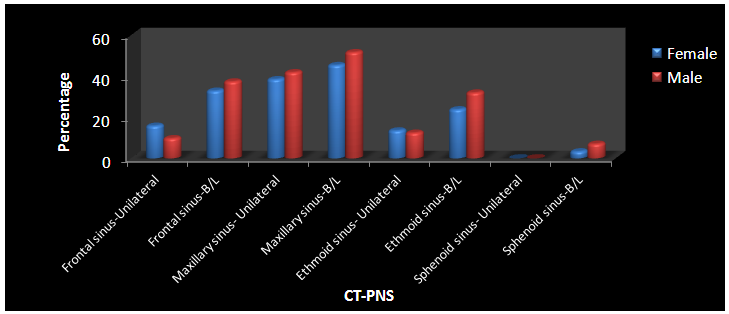
In this study patients bilateral maxillary sinusitis was seen in 98 patients (49%), unilateral maxillary sinusitis in 81 patients (40.5%), bilateral frontal sinusitis in 71 patients (35.5%), unilateral frontal sinusitis in 25 patients (12.5%), bilateral ethmoidal sinusitis in 54 patients (27%), unilateral ethmoidal sinusitis in 26 patients (13%) and bilateral sphenoidal sinusitis was seen in 11 patients (5.5%). 11 patients had pansinusitis (5.5%) [Graph-5].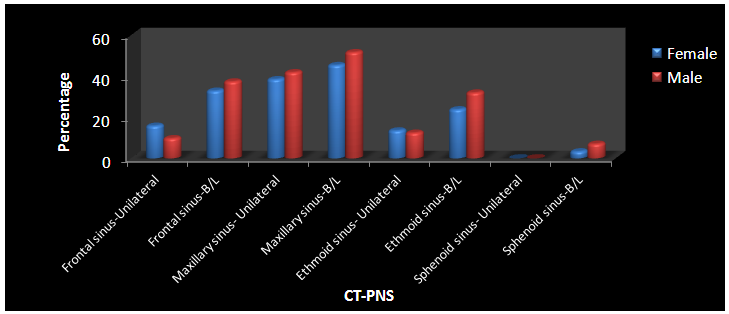 | Graph 5. Showing distributions of CT-PNS findings of patients studied |
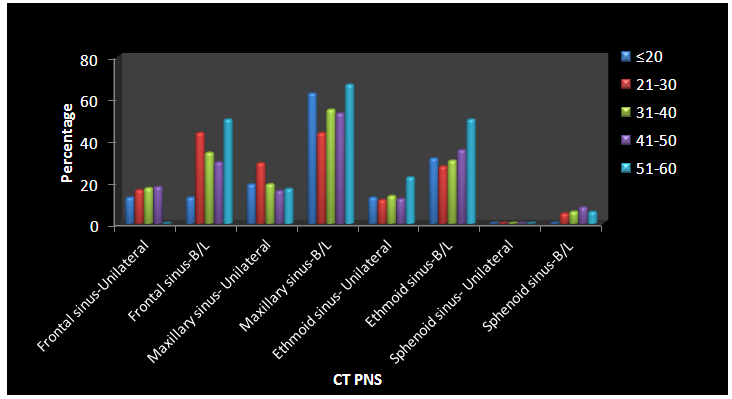
In our study frontal sinusitis was commonly presented by age group 21-30 yrs, while maxillary sinusitis was seen in age group in 21-30 yrs, ethmoidal sinusitis was a common presentation in 51-60 yr age group, sphenoidal sinusitis was seen as part of pansinusitis commonly in age group of 41-50 yrs [Table-4, Graph-6].Table 4. CT- PNS showing sinusitis in relation to Age in years
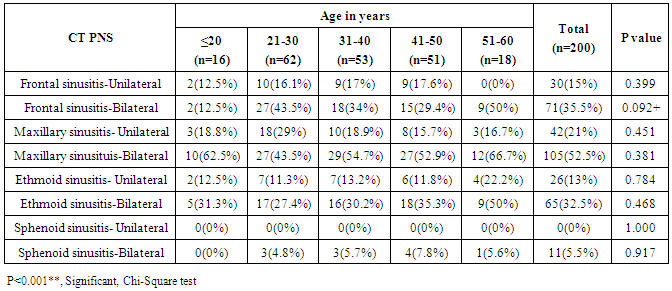 |
| |
|
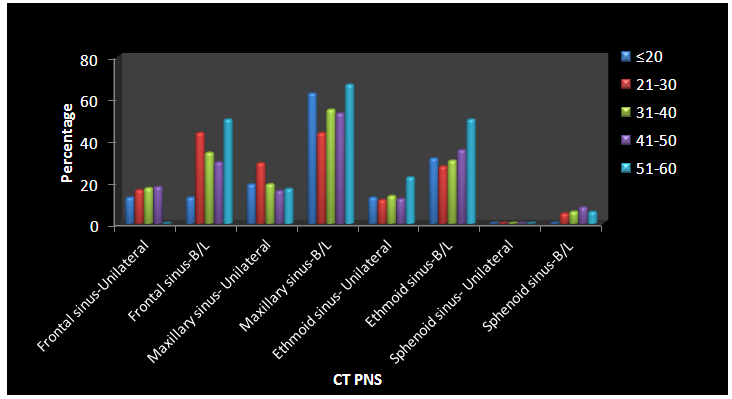 | Graph 6. CT- PNS showing sinusitis in relation to Age in years |
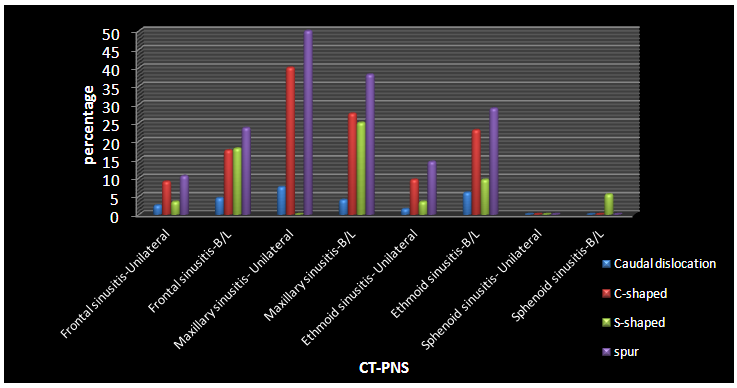
In this study 80 patients with unilateral maxillary sinusitis (40%), 55 patients of bilateral maxillary sinusitis (27.5%), 46 patients with bilateral ethmoidal sinusitis (23%), 19 patients with ethmoidal sinusitis (9.5%), 35 patients with bilateral frontal sinusitis (17.5%) and 18 patients of unilateral frontal sinusitis (9%) were associated with C-shaped DNS. 50 patients with bilateral maxillary sinusitis (25%), 36 patients of bilateral frontal sinusitis (18%), 19 patients of bilateral ethmoidal sinusitis (9.5%) and 11 patients of bilateral sphenoidal sinusitis (5.5%) were associated with S-shaped DNS.38 patients of unilateral maxillary sinusitis (50%), 29 patients of bilateral maxillary sinusitis (38.1%), 18 patients of bilateral frontal sinusitis (23.6%), 8 patients of unilateral frontal sinusitis (10.5%), 22 patients of ethmoidal sinusitis (28.9%)s and 11 patients of unilateral ethmoidal sinusitis (14.4%) were associated with spur [Graph-7].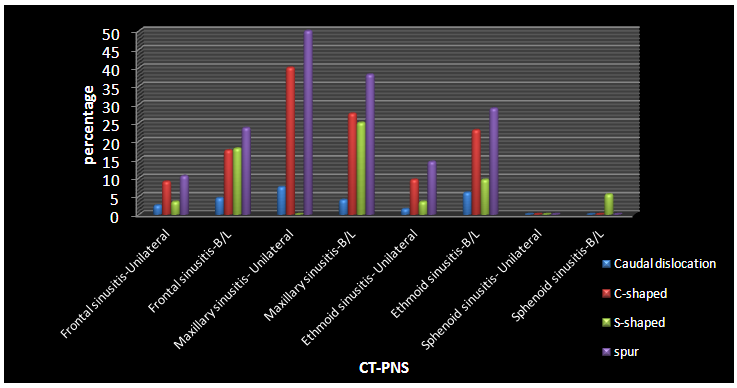 | Graph 7. CT-PNS in relation to DNS |
4. Discussion
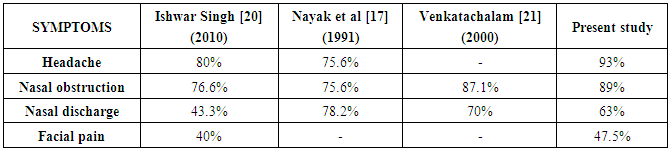
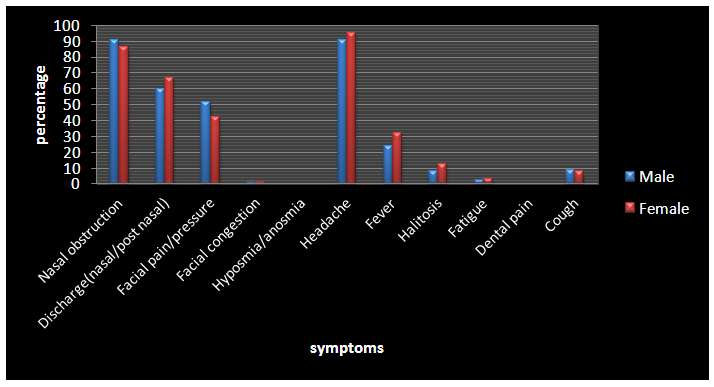
A total of 200 patients were enrolled in the study between 15 and 60 years old. All the patients presenting with symptoms of deviated nasal septum and rhinosinusitis of more than 12 weeks duration with 2 major and one minor or 2 minor symptoms were included in the study. Patients diagnosed as cases of rhinosinusitis based on TFR criteria [14].There are three theories explaining physiopathological relation between the nasal septal deviation and chronic rhinosinusitis. The first of these is the mechanical theory which states that secretions accumulates in the sinus as a result of narrowing of the ostiomeatal complex and thus infections ensues in the retained secretions and causes chronic rhinosinusitis. The second theory is the aerodynamic theory. According to this theory, the mucociliary activity decreases following the nasal flow rate increase and mucosal dryness in relation with the nasal septal deviation and consequently, chronic rhinosinusitis develops. The third theory is the Bachert’s pressure theory. According to this theory, deviation of the posterior nasal septum causes chronic rhinosinusitis by creating pressure and air flow changes within the maxillary sinuses [15, 16].In the present study the incidence of DNS was more in male than female with an approximate ratio of 2:1 which is in agreement to a study done by Nayak et al [17]. In a study by Madani et al, there were 68.3% male and 31.7% female with a mean age of 29.13±15.21 years [18]. Ozkurt et al in his study observed that incidence was more in male as compared to female [19].Headache was predominant symptom in our study seen in 186 patients (93%), nasal obstruction in 178 patients (89%), nasal discharge in 126 patients (63%), facial pain in 95 patients (47.5%), fever in 55 patients (27.%), halitosis in 20 patients (10%), cough in 17 patients (8.5%), fatigue in 6 patients (3%). In the study conducted by Ishwar Singh (2010) headache was the predominant symptom seen in 80% of patients, nasal blockage was seen in 76.66%, nasal discharge was seen in 43.33%, facial pain in 40% patients [20]. While in the study by Venkatachalam et al (2000) the commonest symptoms were nasal obstruction in 87%, nasal discharge in 70% of patients and the other symptoms were post nasal drip in 41% and abnormalities in sensation of smell in 36% of patients [21]. In another study by Nayak et al (1991) nasal discharge was the commonest complaint seen in 78.2%, while nasal blockage and headache was seen in 75.6% of patients [17] [Table 5].Table 5. Comparison of CRS symptoms of different studies
 |
| |
|
In our study most patients had bilateral maxillary sinusitis in 98 patients (49%) while unilateral maxillary sinusitis was seen in 81 patients (40.5%), bilateral frontal sinusitis was seen in 71 patients (35.5%), while unilateral frontal sinusitis was seen in 25 patients (12.5%), bilateral ethmoidal sinusitis was presented in 54 patients (27%) while unilateral ethmoidal sinusitis was seen in 26 patients (13%) and bilateral sphenoidal sinusitis was seen in 11 patients (5.5%). 11 patients had pansinusitis (5.5%) while no patient presented with unilateral sphenoidal sinusitis.In a study by Mohebbi et al, bilateral maxillary sinusitis presentation was seen in 27% of patients while unilateral presentation was seen in 18.4%, similarly unilateral frontal sinus involvement was seen in 12.5% and bilaterally in 11.2%, bilateral ethmoidal sinusitis was seen in 36.1% and unilateral ethmoidal sinusitis was seen in 18.1%, bilateral sphenoidal sinusitis was seen in 12.3%, unilateral sphenoid sinusitis was seen in 13% [13]. In a study by Madani et al, involvement of maxillary sinuses is seen in 41.6% followed by ethmoidal sinuses in 22.9%, then sphenoidal sinusitis in18%, frontal sinuses in17.3% [18].In this study, C-shaped DNS was associated with unilateral maxillary sinusitis in 40% of patients, bilateral maxillary sinusitis in 27.5% of patients, bilateral ethmoidal sinusitis in 23% of patients, unilateral ethmoidal sinusitis in 9.5% of patients, bilateral frontal sinusitis in 17.5% of patients and unilateral frontal sinusitis in 9% of patients. S-shaped DNS was associated with bilateral maxillary sinusitis in 25% of patients, bilateral frontal sinusitis in 18% of patients, bilateral ethmoidal sinusitis in 9.5% of patients and bilateral sphenoidal sinusitis in 5.5% of patients.Spur was associated with unilateral maxillary sinusitis in 50% patients, bilateral maxillary sinusitis in 38.1% of patients, bilateral frontal sinusitis in 23.6% of patients, unilateral frontal sinusitis in 10.5% of patients, bilateral ethmoidal sinusitis in 28.9% patients and unilateral ethmoidal sinusitis in 14.4% of patients.In a study done by Moorthy et al, C-shaped deviation was associated with ostiomeatal complex block in 42.5% of patients and pansinusitis was seen in 50% of patients, similarly S-shaped deviation was associated with OMC block in 23.3% and pansinusitis in 83.3%, spur was associated with OMC block and pansinusitis in 30% of patients each respectively [11].Rao et al in their study found horizontal spur was most commonly associated in sinus pathology, 43.4% of patients spurs were accounted for sinus pathology, similarly type III (posterior vertical deviation) was seen having osteo meatal complex (OMC) block in 62.5% of cases, S-shaped deviation was associated with OMC block in 50% of cases [8].In this study we found that the prevalence of nasal septal deviations and the sinusitis was significant [p-value is <0.001]. Present study showed:1. Chronic sinusitis was prevalent in males.2. Headache was the most common symptom followed by nasal blockage due to pressure and airflow changes caused by DNS. 3. C-shaped deviation was the most common presentation, being more common on the left side. 4. Bilateral Maxillary sinusitis was the commonest presentation, more so in association with C-shaped DNS.5. Pansinusitis was only associated with S-shaped deviation, since S-shaped DNS obstructs the laminar airflow pattern in both the nasal cavities.6. Isolated sphenoid sinusitis was not seen as the sinuses occupy a midline position. The ostium occupies a medial and superior position on either side of the nasal septum; hence obstruction of the ostia due to DNS is less commonly seen.
5. Conclusions
Chronic rhinosinusitis is most common rhinological problem encountered worldwide which has greater propensity to cause morbidity. Deviated nasal septum can be associated with significant sinonasal disease, especially a C-shaped DNS which showed statistically significant correlation with sinus disease in our study. This study brings to light various presentations of DNS implicated in causation of chronic sinusitis which will influence the treatment decisions and also reduce the morbidity caused by it.
References
| [1] | Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, Itzhak Brook I, Kumar KA, Kramper M, et al. Clinical Practice Guideline (Update): Adult Sinusitis. Otolaryngology–Head and Neck Surgery 2015, Vol. 152(2S) S1–S39. |
| [2] | Rodney J Schlosser and David W Kennedy, Nasal endoscopy, Scott-Brawn's Otorhinolaryngology, Head and Neck Surgery, volume 2:2008, pg 1344. |
| [3] | Lloyd G. CT of the paranasal sinuses: study of a control series in relation to endoscopic sinus surgery. J LaryngolOtol. 1990; 104:477–481. |
| [4] | Lusk RP, McAlister B, Ahmed F. Anatomic variations in Pediatric chronic sinusitis. A CT study. OCNA 1996; 29:75-91. |
| [5] | Kennedy DW, Zinreich J, Arthur E, Rosenbaum, Johns ME. Theory and diagnostic evaluation. Arch Otolaryngol Head and Neck Surg 1985; 111(9): 576- 582. |
| [6] | Collet S, Bertrand B, Cornu S, Eloy P, Rombaux P. Is septal deviation a risk factor for chronic sinusitis? Review of literature. Acta Otorhinolaryngol Belg.2001; 55(4):299-304. |
| [7] | Harar RPS, N.K. Chadha, G. Rogers, The role of septal deviation in adult chronic rhinosinusitis: a study of 500 patients, Rhinology 2004; 42:126-130. |
| [8] | Rao JJ, Kumar ECV, et al. Classification of nasal septal deviations-relation to sinonasal pathology,” Indian journal of otolaryngology and head and neck surgery 2005; 57(3): 199-201. |
| [9] | Smith KD, Edwards PC, Saini TS, Norton NS, The prevalence of concha bullosa and nasal septal deviation and their relationship to maxillary sinusitisby volumetric tomography. International Journal Of Dentistry. 2010. |
| [10] | Kapusuz Gencer Z, Ozkins M, Okur A, Karacavus S, Saydam L, “The effect of nasal septal deviation on maxillary sinus volumes and development of maxillary sinusitis. Eur arch Otorhinolaryngol.2013 Nov; 270(12)3069-73. |
| [11] | Moorthy PNS, Kolloju S, Madhira S, Jowka AB. Clinical study on deviated nasal septum and its associated pathology. International Journal of Otolaryngology and Head & Neck Surgery, 2014, 3, 75-81. |
| [12] | Rehman A, Hamid S, Ahmad M, Rashid AF. A prospective study of nasal septal deformities in Kashmiri population attending a tertiary care hospital”, International Journal of Otolaryngology and Head & Neck Surgery, 2012, 1, 77-84. |
| [13] | Mohebbi et al.: An epidemiologic study of factors associated with nasal septum deviation by computed tomography scan: a cross sectional study. BMC Ear, Nose and Throat Disorders 2012 12:15. |
| [14] | Lanza DC, Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg 1997; 117(3):S1–7. |
| [15] | Brown S. Anatomy of nose and paranasal sinuses. In: Lund VJ, H Stammberger, Scott Brown Otolaryngology, Basic Sciences; 5, Butterworth-Heinemann; oxford, 7th edn; 2008: Pg1318. |
| [16] | Adrian Drake-Lee “The Physiology of the Nose and Paranasal Sinuses” Scott Brown’s Otolaryngology. 6th edition, Volume 1, Basic Sciences pp 1/6/11-15. |
| [17] | Nayak DR, Balakrishnan R, Murty DK. Hazarika P. Endoscopic septo turbinoplasty: our update series”, Indian Journal of Otolaryngology and Head and Neck Surgery Vol. 54 No. 1, January - March 2002. |
| [18] | Madani SA et al: Association between anatomical variations of the sinonasal region and chronic rhino sinusitis: A Prospective Case Series Study. Scientific Journal of the Faculty of Medicine in Niš 2013; 30(2): 73-77. |
| [19] | Ozkurt FE et al., Relation Between the Nasal Septal Deviation and Chronic Rhinosinusitis, International Journal of Basic and Clinical Studies (IJBCS) 2014; 3(1): 25-30. |
| [20] | Singh I et al, Chronic Rinosinusitis and Nasal Polyposis in Nepal, Clinical Rhinology: An International Journal, May-August 2010; 3(2):87-91. |
| [21] | Venkatachalam VP, Bhat A. Functional endoscopic sinus surgery: A newer surgical concept in the management of chronic sinusitis. Indian J Otolaryngol Head Neck Surg 1999- 2000; 52(1):13-16. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML