-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2015; 4(4): 49-53
doi:10.5923/j.otolaryn.20150404.02

Silicone Stenting and Polypropylene Stenting in Endoscopic Dacryocystorhinostomy: A Prospective Comparative Study
Borlingegowda Viswanatha, Maliyappanahalli Siddappa Vijayashree
Otorhinolaryngology department, Bangalore medical college & research institute, Bangalore, India
Correspondence to: Borlingegowda Viswanatha, Otorhinolaryngology department, Bangalore medical college & research institute, Bangalore, India.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: This study was done to compare the clinical efficacy of silicon and polypropylene for stenting in endoscopic dacryocystorhinostomy.Patients and methods: There were 20 patients who were randomly divided into two groups [Group A – 10 patients and Group B– 10 patients]. All 20 patients underwent unilateral endoscopic dacryocystorhinostomy operation. Group-A patients underwent dacryocystorhinostomy and silicone stenting. Group-B patients underwent dacryocystorhinostomy and polypropylene suture material was used for stenting. Stents were left in the lacrimal sac for 3 months. The patients were followed up for 6 months. Based on the improvement in the complaint of epiphora, they were grouped as good improvement, partial improvement and no improvement.Results:In group-A, improvement was good in 9 patients (90%), whereas improvement was partial in 1 patient (10%). Granulation tissue formation around the silicon stent was seen in one patient (10%).In group B, improvement was good in 8 patients (80%), whereas improvement was partial in 1 patient (10%), and there was no improvement in 1 patient (10%). Granulation tissue formation around the polypropylene was seen in one patient.Conclusions: Silicone stents and polypropylene stents are equally good for stenting in endoscopic dacryocystorhinostomy. Polypropylene can be used successfully in endoscopic dacryocystorhinostomy as an alternative to silicone stent because polypropylene suture material is cheap, effective, and readily available in all operating theaters.
Keywords: Dacryocystorhinostomy, Silicone stent, Polypropylene stent
Cite this paper: Borlingegowda Viswanatha, Maliyappanahalli Siddappa Vijayashree, Silicone Stenting and Polypropylene Stenting in Endoscopic Dacryocystorhinostomy: A Prospective Comparative Study, Research in Otolaryngology, Vol. 4 No. 4, 2015, pp. 49-53. doi: 10.5923/j.otolaryn.20150404.02.
Article Outline
1. Introduction
- The dacryocystorhinostomy (DCR) surgery involves fistulization of the lacrimal sac into the nasal cavity. DCR is currently the treatment of choice for nasolacrimal duct obstruction [1] The first report of DCR (intranasal approach) was described by Caldwell in 1893 [2]. Since its first description by McDonough and Meiring, endoscopic DCR gained popularity [3]. The operation can be carried out using either an external or endonasal surgical approach. The external approach is the surgery of choice for ophthalmologists [4]. Advances in endoscopic equipment have popularised the endoscopic transnasal approach by Otorhinolaryngologists [5]. The advantages of endoscopic DCR as compared to external DCR include the lack of skin incision, short operating time, and lower risk of interfering with the physiological lacrimal pump mechanism, minimal blood loss and the possibility to correct associated intra-nasal pathological conditions during the same procedure [5, 6]. Many surgeons prefer to place bicanalicular silicon tube to stent the intranasal ostium, with a high success rates. In the literature, as an alternative method to silicone intubation, several other materials have been used to retain the lacrimal aperture following endoscopic DCR. Aslan et al used polypropylene suture material as an alternative to silicone stent in endoscopic DCR operations [4]. Its strength, inertness, retention of strength after application, minimum tissue reactivity, and resistance to bacterial contamination are its advantages [7, 8].This study was done to compare the clinical efficacy of silicone and polypropylene for stenting in endoscopic dacryocystorhinostomy.
2. Patients and Methods
- This prospective study was done at the tertiary care institute. There were 20 patients who were randomly divided into two groups. In this study there were 10 patients in group-A (6 females and 4 males) and 10 patients in group-B (5 females and 5 males). The age of the patients in the study ranged from 26 to 50 years. Informed consent was obtained from the patients. All patients underwent routine pre-operative ophthalmologic and otorhinolaryngologic examination, diagnostic nasal endoscopy and blood investigations. Lacrimal sac or nasolacrimal duct obstruction was confirmed by the results of lacrimal irrigation.
3. Surgical Technique
- All 20 patients underwent DCR under local anesthesia. The nasal cavity on the side of surgery was decongested for 15 minutes using cottonoid pledgets soaked in lidocaine 4% with adrenaline 1:100 000. Patients were given premedication. Inside the operating room, cottonoid pledgets were removed from the nasal cavity. Using nasal endoscope, 2% lidocaine with adrenalin anesthetic solution was injected submucosally to the lateral nasal wall corresponding to the sac location just anterosuperior to the insertion of the middle turbinate. A curved incision was made at the lateral nasal wall mucosa including periosteum, just anterior to the attachment of the middle turbinate. A suction Freer’s elevator was used to lift the mucosal flap, keeping the mucosa between the middle turbinate and the lateral nasal wall intact. Bone over the lacrimal sac area was removed using Kerrison’s punch. Lacrimal sac was identified by passing a lacrimal probe through the inferior canaliculus into the sac, or by pressing on the skin inferior and medial to the medial canthus and observing the movement of the sac. Vertical incision is made on the medial wall of the sac and the opening was widened using cutting punch forceps. The patency of the lacrimal drainage system was checked with saline irrigation. Lacrimal punctum was dilated using punctum dilator. In group-A patients after dacryocystorhinostomy, silicone tube stenting was done [Figure 1 & 2]. In group-B patients after dacryocystorhinostomy, polypropylene suture material was used for stenting. Number 2/0 polypropylene was inserted into the sac through both the canaliculi [Figure 3]. Both ends of the polypropylene were then fastened with several knots [Figure 4]. Precaution was taken to ensure that the polypropylene stayed loose in the region of the inner canthus to prevent canalicular laceration. Gentle nasal packing was done for all the patients.
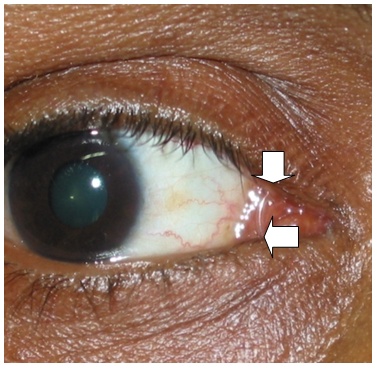 | Figure 1. Showing silicone stent passing through both the canaliculi |
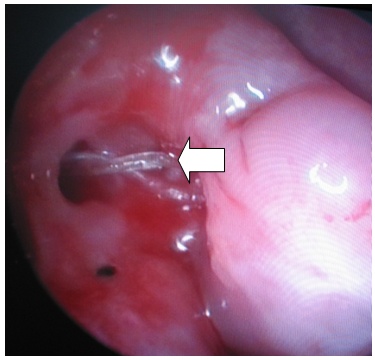 | Figure 2. Showing silicon stent in the nasal cavity |
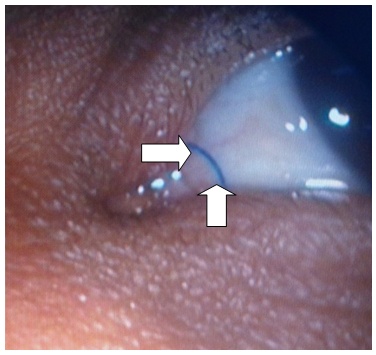 | Figure 3. Showing polypropylene stent passing through both the canaliculi |
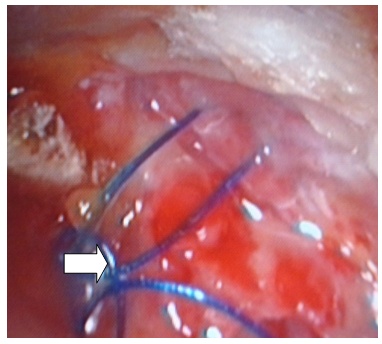 | Figure 4. Showing polypropylene stent tied with multiple knots in the nasal cavity |
4. Postoperative Follow-up
- All the patients were discharged on the next day of the procedure after removing the nasal pack. Oral antibiotics were given for 7 days. Saline nasal drops and topical antibiotic eye drops were given four times a day for 2 weeks. Patients were examined endonasally in the rhinology clinic in second and fourth week in the first month. Nasal endoscopy was done once a month until the stent removal. The stent was removed at the end of 3 months. Patency of the lacrimal system was assessed by rigid nasal endoscopy and irrigation with saline. The resolution of epiphora with patent ostium during nasal endoscopy at the end of six months was accepted as a successful result. The eyes with no epiphora were grouped as good improvement. The eyes which experienced epiphora occasionally were grouped as partial improvement. The eyes that still had epiphora were grouped as no improvement.
5. Results
- The age range of our patients was between 26 and 50. There were 20 patients who underwent revision endoscopic DCR procedures. The patients were followed over a period of 6 months. Anatomical patency with lacrimal syringing and improvement of the epiphora complaint at the end of 6 months was considered as successful surgery.In group-A, improvement was good in 9 patients (90%), whereas improvement was partial in 1 patient (10%). Granulation tissue formation around the silicone stent was seen in one patient (10%) [Figure 5].
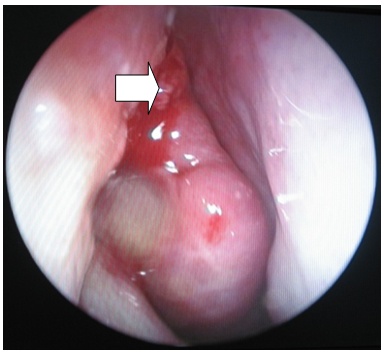 | Figure 5. Showing granulation tissue around silicone stent in the nasal cavity |
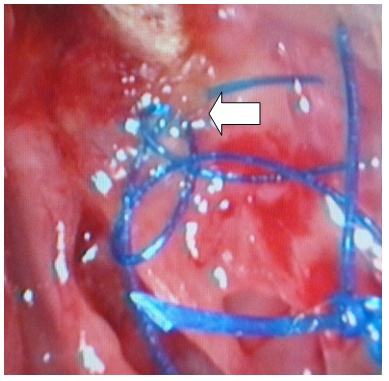 | Figure 6. Showing granulation tissue around polypropylene stent in the nasal cavity |
6. Discussion
- DCR surgery involves fistulization of the lacrimal sac into the nasal cavity. It is currently the main stay of treatment of nasolacrimal duct obstruction [1]. The first report of DCR (intranasal approach) was by Caldwell in 1893 [2]. Later in 1904, Toti described DCR by external approach [9]. Endoscopic DCR is becoming popular as a relatively quick and easy surgery for post-saccal obstruction of the nasolacrimal drainage system [4].Closure of the rhinostomy opening was considered a major factor for surgical failure in external DCR [10]. Inadequate bone removal is also a common cause of failure. Various instruments can be used to remove the bone including drill (cutting or diamond burr), curette, Smith-Kerrison forceps or laser (KTP, Diode, Argon, Holmium: YAG, CO2) [3, 5, 11, 12].The success rate depends on providing a wide intranasal stoma with removal of adequate bone around the stomal area, reducing the chances of postoperative stenosis and adhesions. Inadequate bone removal is the commonest cause of postoperative stomal stenosis [13]. Technical error in locating the sac, intra operative bleeding hampering the vision or small obliterated atrophic sac or impaired canalicular function also leads failure of DCR. Endocanalicular stenting is believed to maintain the patency of the ostium during the post operative period &healing process [1].Although controversial, silicone stents are used to keep the neo-ostium open after the procedure and are thought to maintain the patency of the ostium by preventing circular stenosis of the neo-ostium in the post-operative healing period [10], the use of silicone stents is considered routine in many institutions [6].Insertion of silicone stents prevents rhinostomy stenosis and helps to stabilize epithelialization between two mucosal surfaces having surgical continuity [14]. A bicanalicular silicone tube is the stent most often used in DCR procedures to prevent obliteration of the rhinostomy opening after DCR [4].Allen and Berlin reported a higher failure rate when stents were used [15]. Vishwakarma et al had a high success rate with silicone stenting [16]. During their study Ambani et al [1] noted that the failure of endoscopic DCR especially in cases where no stent was used, were because of granulations and scarring near stoma. Singh et al and Sham et al on the basis of their studies opined that silicone stenting is not routinely indicated in endoscopic DCR. [17,18]. Silicone stent is associated with high failure rate due to granulomatous inflammation and complications as punctal erosion and slitting of canaliculi [10]. Many surgeons may not prefer the stents if the patient has not had a previous operation (external DCR) and if they are available for regular postoperative visits [4]. Silicone tubes were first used in DCR by Gibbs in 1967 [19]. Later, Keith and Quickert and Dryden added probes to the silicone tubes [20, 21]. In the literature, as an alternative method to silicone intubation, T-sheet made from a penrose drain tube, otologic T-tubes, polypropylene suture material have been used to retain the lacrimal aperture following endoscopic DCR [4, 22, 23]. The usefulness of polypropylene for stenting in DCR has been reported by Aslant et al [4].Tamura et al [22] used T-sheet made from a penrose drain tube in seven patients [18]. In their study results were very good in four patients (57%), good in two patients (29%), and showed no change in one patient (14%). They detected granulation tissue in two of seven patients and reported spontaneous tube loss in the early period in 1 of 7 patients. In the present study also granulation was detected in one patient [10%] with silicone tube stenting and in one patient [10%] with polypropylene stenting. Kishore et al [23] used standard otologic T-tubes in endoscopic DCR. Kishore et al [6, 19] did not observe any granulation around the T-tube. Erkan et al [24] used standard otologic T-tubes in endoscopic DCR. In their study results were every good in 11 patients (50%), good in five patients (23%), and showed no change in six patients (27%). They reported spontaneous tube loss in the early period in 3 of 22 eyes and they did not observe any granulation around the T-tube. In the present study, silicone tube was used in 10 patients and polypropylene was used as stents in 10 patients. In both the groups granulation was detected in one patient [10%]. The success rate with polypropylene stenting in endoscopic DCR procedures was 80% and success rate with silicone tube stenting was 90%. When compared to silicone stents, polypropylene is cheaper and it is readily available in all operation theaters. It is a good alternative to silicone stents.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML