-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2015; 4(4): 45-48
doi:10.5923/j.otolaryn.20150404.01

Superior Semicircular Canal Dehiscence Syndrome - A Case Report
Prem G. Nair 1, Dayana Devassy 1, Bini Faizal 2, Gayathri K. S. 1
1Department of Speech pathology and Audiology, Amrita Institute of Medical Sciences and Research Centre, Kochi, India
2Department of Ear Nose and Throat, Amrita Institute of Medical Sciences and Research Centre, Kochi, India
Correspondence to: Dayana Devassy , Department of Speech pathology and Audiology, Amrita Institute of Medical Sciences and Research Centre, Kochi, India.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Superior Semicircular Canal Dehiscence Syndrome (SCDS) is a rare disease. The present article reports about a patient who presented with recurrent episodes of giddiness since 10 years and tinnitus since three months. She also reported symptoms of autophony. Tullio phenomenon was also positive. Audiological investigations such as immittance audiometry, puretone audiometry and Vestibular Evoked Myogenic Potential (VEMP) evaluation helped in identifying SCDS in this patient. The audiological and vestibular evaluation corresponded with High Resolution Computerized Tomography (HRCT) findings. The present report signifies the importance of audiological investigations in uncovering SCDS. Thorough analysis of case history and ability to correlate various audiological and vestibular findings are crucial in identifying cases like SCDS.
Keywords: Superior Semicircular Canal Dehiscence Syndrome, Vestibular Evoked Myogenic Potential, Tullio Phenomenon
Cite this paper: Prem G. Nair , Dayana Devassy , Bini Faizal , Gayathri K. S. , Superior Semicircular Canal Dehiscence Syndrome - A Case Report, Research in Otolaryngology, Vol. 4 No. 4, 2015, pp. 45-48. doi: 10.5923/j.otolaryn.20150404.01.
1. Introduction
- The Superior Semicircular Canal Dehiscence Syndrome (SCDS) is a rare condition. It is estimated to be seen in approximately 0.1% of the population [1]. The SCDS is a dehiscence (opening) in the bone overlying the superior semicircular canal of the inner ear. It is the most common cause of sound and pressure induced vestibular symptoms such as imbalance, vertigo and oscillopsia. It was first described by Minor, Solomon, Zinreich and Zees in 1998 [2]. It consists of a variety of auditory symptoms including autophony, hyperacusis, tinnitus, as well as vestibular symptoms of sound-induced and pressure-induced vertigo. These symptoms arise as a result of the third mobile window effect from a dehiscence of the Superior Semicircular Canal (SCC). Estimation of Vestibular Evoked Myogenic Potential (VEMP) threshold has been considered an important diagnostic tool in SCDS [3]. The present case study reports of a patient who was primarily complaining of recurrent episodes of giddiness since 10 years (associated with change in position of head-more to left). The patient was diagnosed as having Left SCDS. The objective of this paper is to highlight the importance of audiological investigations in identifying SCDS.
2. Case Report
- This 25 year old patient was referred to Department of Speech pathology and Audiology, Amrita Institute of Medical Sciences, Kochi from Department of ENT. The patient was complaining of recurrent episodes of giddiness since past 10 years. She reported marked worsening of the symptoms since past 3 months. She reported no true rotatory sensation. The giddiness episodes lasted for approximately 5 minutes and used to relieve on rest. It was associated with change in position of head (more to left). She had no complaint of decreased hearing, ear discharge or ear pain. The patient also had complaint of left ear pulsatile tinnitus since 3 months and increased perception of patients own speech (autophony). Tullio phenomenon was positive. Positional testing, tandem walking and Untenberger were negative.
3. Method
- Immittance audiometry was performed using Grason Stadler Incorporates (GSI) Tympstar equipment. Tympanogram and acoustic reflexes (ipsilateral and contralateral recordings) were carried out. The puretone audiometry was performed using GSI-61 clinical audiometer over the frequency range of 250 to 8000 Hertz (Hz) for air conduction and 250 to 4000 Hz for bone conduction. Audiometric Weber testing was also carried out for the frequencies from 250 Hz-4000 Hz. The earphones used were TDH-50 P and bone vibrator was B-71 Radioear. Vestibular Evoked Myogenic Potential (VEMP) evaluation was carried out using Intelligent Hearing System. The VEMP recordings were made by single channel recording. The non-inverting electrode was placed on the middle of testing side sternocleidomastoid muscle, inverting electrode on sternoclavicular junction and ground electrode on forehead. The subject was instructed to activate the sternocleidomastoid muscle by adjusting the head position. The stimulus used was 500 Hz Blackman tone at 95 decibel normal Hearing Level (dB nHL). The intensities were lowered in 10 dB steps till responses were obtained. The polarity used was rarefaction. All evaluations were carried out in acoustically sound-treated rooms.
4. Results
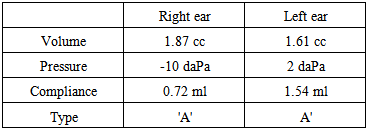
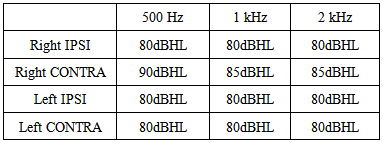
- Immittance audiometry revealed bilateral A type tympanogram indicating intactness of external ear and middle ear. Acoustic reflexes were obtained bilaterally. The puretone audiometric results indicated that hearing sensitivity was essentially within normal limits bilaterally. Weber test results revealed that responses were lateralized to left ear at all frequencies. Speech Reception Thresholds were correlating with Puretone Average and Speech Discrimination Scores were 100% bilaterally. The VEMP evaluation revealed that P1 and N1 were obtained at normal latencies up to 75 dB nHL. Left ear VEMP amplitudes were higher than right ear values and asymmetry ratio was significantly different (73%) at 95 dB nHL. High Resolution Computed Tomography (HRCT) done on this patient revealed Superior Semicircular Canal Dehiscence (SCD) in the left ear. The symptomatology of the patient and results obtained in audiological investigations such as audiometric Weber, Immittance audiometry and VEMP clearly correlated with the HRCT findings. Pre-operative investigations: Table 1 and 2 reveals immittance audiometry findings. Figure 1 and 2 provide puretone audiometry findings and VEMP findings respectively.
|
|
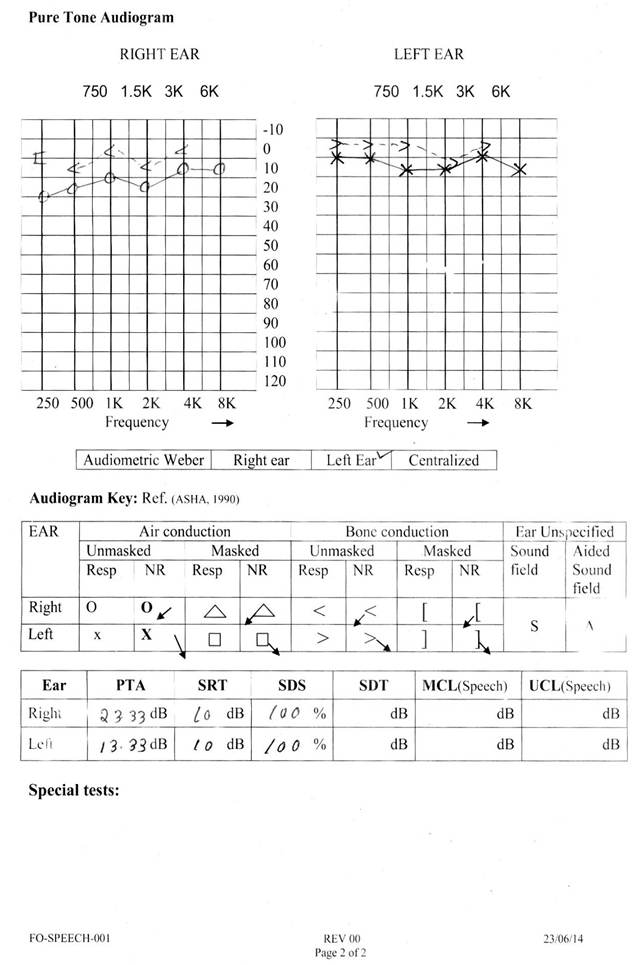 | Figure 1. Pure Tone Audiometry |
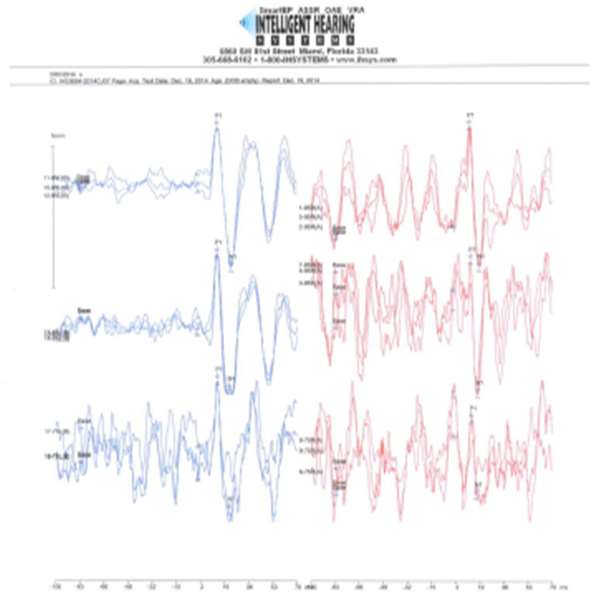 | Figure 2. Vestibular Evoked Myogenic Response (VEMP) |
5. Discussion
- This patient with SCDS had classifical features such as giddiness, tinnitus and increased perception of own speech (autophony). Tullio phenomenon (sound induced vertigo) was also present. It had been demonstrated previously that patients with SCDS show Tullio phenomenon, i.e, vestibular hypersensitivity to air conducted low frequency sounds [2, 4, 5, 6]. The altered air conducted response in patients with SCDS is attributed to be due to the low impedance for sound transmission through the superior canal [2]. Weber test done using tuning fork revealed that sound energy was lateralized to left ear. This was confirmed using bone vibrator, which also revealed similar findings. Minor, 2005 [7] reported that the third mobile window in SCDS allows acoustic energy to be dissipated through the dehiscence and this mechanism resposible for vestibular abnormalities also underlies the auditory manifestation in Weber test [7]. This finding is further supported by the study of Rosowski et al., 2004 [9] which reported that cochlear potential measured in Semicircular Canal Dehiscence (SCD) showed an increase in bone conducted sounds.Tympanometric findings of bilateral A type with present acoustic reflexes ruled out the possiblity of any external ear or middle ear pathology bilaterally. This was in agreement with ENT findings of bilateral intact tympanic membrane. VEMP is considered as an important diagnostic tool in diagnosing SCDS. Our finding revealed that left ear VEMP amplitudes were higher than right ear and the assymetry ratio was significantly different (73%). The VEMP response to air conducted sounds are larger as reported by Brantberg, Lofqvist and Fransson, 2004 [10]. The VEMP responses have larger amplitude in superior canal dehiscence.The present study finding is in accordance with the literature and this could be attributed to lowered impedance for transmission of sound and pressure stimuli created by the third mobile window. Thus the VEMP stimulus in an ear with superior canal dehisence results in larger activation of the sacculus than a comparable stimulus in an ear without dehiscence [7]. The presence of symptoms and signs such as giddiness, tinnitus, autophony and Tullio phenomenon along with Weber, immittance audiometry and VEMP test findings pointed to the probable diagnosis of SCDS in left ear. The symptamatology of patient and audiological results correlated with HRCT findings. This signifies that careful analysis of patients history along with thorough audiological examination will help in diagnosing conditions such as SCDS. Although different mechanisms like proprioception, vision and vestibular system are involved in maintaining balance and posture, a thorough case history and careful audiological investigations have the potenial to identify the broad system involved and even arrive at the exact pathology as demonstrated in this case study. The clinician's knowledge regarding the anatomy, physiology and pathophysiology of vestibular system is extremely crucial. Plus, the strength of a thorough case history should be fully utilized and findings from related professionals should be clinically correlated. The neurosurgery team performed neuronavigation guided left middle fossa approach and repair of dehiscence under general anesthesia in this patient. Postoperative findings: Figure 3 demonstrates postoperative CT scan. The repaired SCD can be seen in figure 3.
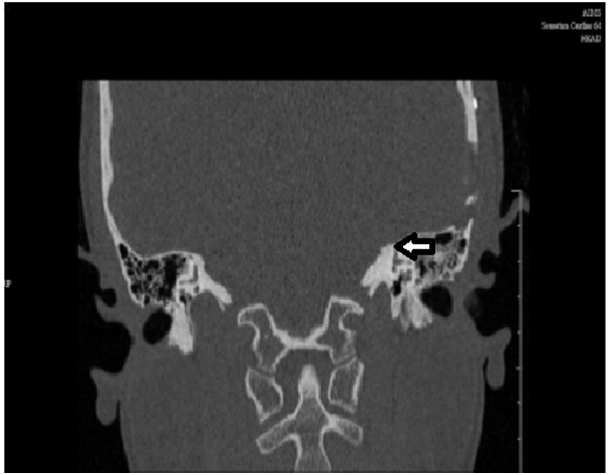 | Figure 3. Postoperative CT scan demonstrating repaired SCD on the left ear |
6. Conclusions
- Balance is maintained by intact functioning of proprioceptive, vision and vestibular mechanisms. Defective functioning of any of these mechanisms could lead to dizziness/balance disorders. The audiologists have a pivotal role in diagnosing the deficits involved. A precise case history, correlation of findings from allied professionals and a thorough audiological and vestibular system work-up could help the audiologists in making significant contributions towards differential diagnosis of vestibular/balance disorders.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML