-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2015; 4(2): 24-28
doi:10.5923/j.otolaryn.20150402.02
Osteoplastic Surgery of the Frontal Sinus – Our Experience
Karthik. Shamanna, Vidya B. Thimmaiah, Roopashri Tarikere Jayaram
Department of Otorhinolaryngology, Bangalore Medical College and Research Institute, Bangalore, India
Correspondence to: Vidya B. Thimmaiah, Department of Otorhinolaryngology, Bangalore Medical College and Research Institute, Bangalore, India.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Frontal sinus disease is not only surgically challenging to treat but is usually associated with failure and complications including intracranial penetration and external fistulous tract. The history of frontal sinus surgery highlights the fact that a number of surgical procedures were introduced from time to time, as there was not a single surgical procedure that was capable of managing the various disease spectrum and were associated with their own set of complications and failures. The latest modalities for management of the frontal sinus disease are endoscopic sinus surgery, microscopic and stereotactic surgeries. However, there are still indications which require conventional or traditional surgical procedure. Our article highlights the importance and effectiveness of combining osteoplastic flap procedure and use of endoscopes in the management of frontal sinus disease which could not be managed by other modalities.
Keywords: Osteoplastic surgery of the Frontal sinus
Cite this paper: Karthik. Shamanna, Vidya B. Thimmaiah, Roopashri Tarikere Jayaram, Osteoplastic Surgery of the Frontal Sinus – Our Experience, Research in Otolaryngology, Vol. 4 No. 2, 2015, pp. 24-28. doi: 10.5923/j.otolaryn.20150402.02.
1. Case Report 1
- A 40 year old female patient presented with history of headache since 2 years and swelling over the forehead since 6 months. Examination revealed a smooth non tender, cystic swelling over the right side of the forehead measuring 3x3 cm with absent cough impulse. No bruit was heard on auscultation.CT scan showed homogenous soft tissue opacity in both the frontal sinus with erosion of the outer and inner table of the right frontal sinus with extension into the cranium and right orbit. A diagnosis of frontal mucocele with intracranial extension was made. Since the mucocele had eroded both the anterior and posterior table of the frontal sinus, the best modality of surgical management was the osteoplastic flap procedure.A bicoronal incision was made over the scalp about 10 mm behind the hairline to camouflage the resulting scar. The frontal skin flap was reflected away from the anterior table periosteum up to the emergence of supraorbital neurovascular bundle. As there was erosion of the anterior table, the defect was enlarged.so as to permit easy access of endoscope. The use of a 30 degree endoscope through the anterior table defect permitted us to visualize the entire breadth of the frontal sinus and easily strip away the mucocele from the walls of the frontal sinus. The defect in the posterior table measuring about 5mm X 5 mm was freshened and a piece of temporalis fascia measuring 10 mm X 10 mm was placed over the exposed dura and the edges of the fascia was tucked between the dura and freshened posterior table. A layer of bone wax was spread over the fascia to seal the bony defect. The frontonasal duct was plugged with temporalis fascia and the frontal sinus was obliterated with fat harvested from the anterior abdominal wall. The forehead flap was repositioned and the incised scalp was approximated with staples. At 6 months of follow up patient remained symptom free without any cosmetic deformity.
 | Figure 1. Profile view of patient showing swelling over the right frontal sinus |
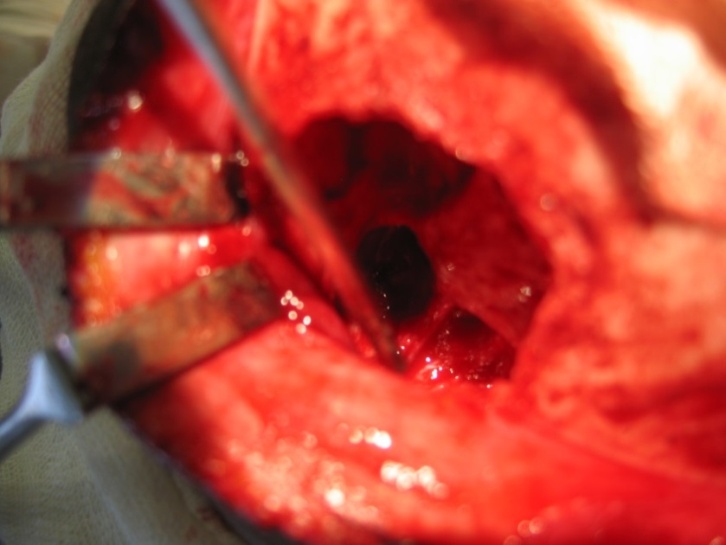
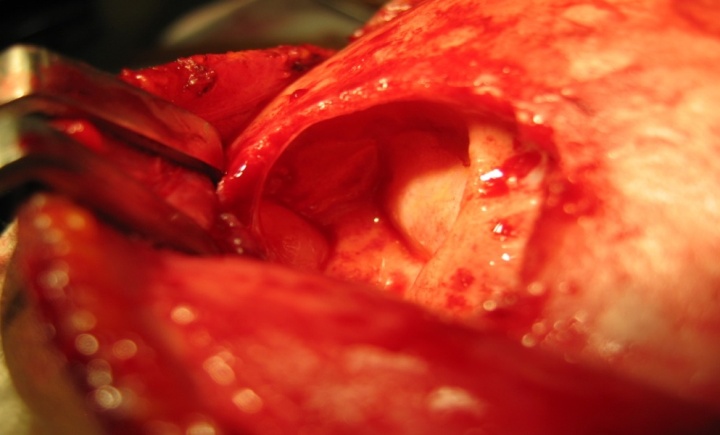 | Figure 2. Intra operative view of defect in both anterior and posterior table of right frontal sinus |
2. Case Report 2
- A 36 year old female patient presented with a history of slow growing swelling over the forehead since 3 months. The onset of the swelling was insidious and gradually progressive in size. It was not associated with pain, fever, headache, nasal discharge, bleeding from the nose, nasal obstruction, alteration in the sense of smell or taste sensation. There was no history of trauma or loss of consciousness.General physical examination was normal. On inspection, diffuse swelling was seen over the left frontal region measuring around 4x3 cm extending from glabella to 3cms above the left supra orbital area. Skin over the swelling was normal. On palpation, the swelling was firm, no local rise of temperature, non tender. Skin over the swelling was mobile. Examination of the nose revealed DNS to the left.CT PNS revealed high density contents in left frontal sinus with erosion of anterior and posterior wall of the frontal sinus causing ill-defined lytic lesion superiorly into the subcutaneous plane of the forehead. Adjacent frontal bone shows reactive sclerosis and erosion of the roof of the left orbit. Nasopharynx appeared normal. The radiological features were suggestive of fungal sinusitis.Opinion from Neurologist, Neurosurgeon and Ophthalmologist was sought and a decision to clear the frontal sinus with osteoplastic flap procedure was made. After elevating the forehead flap the defect in the anterior table of the left frontal sinus was enlarged. The soft tissue mass filling the frontal sinus was visualized, it appeared to be fleshy and aroused the suspicion of malignancy. Inner table of frontal sinus was lined by granulation tissue. With the help of a 30 degree endoscope, an attempt was made to remove the mass. As complete removal of the mass was not possible, the frontal sinus was not obliterated. A type 3 Draf procedure was done to enlarge the frontonasal duct and a large bore soft rubber drain was placed in the sinus and brought out through the left nasal cavity. The forehead flap was repositioned and the scalp skin stapled. The mass was sent for HPE to two different laboratories.Histopathology revealed tissue lined by respiratory epithelium (hyperplastic pseudo stratified ciliated columnar epithelium). Subepithelial stroma was edematous and shows mixed inflammatory infiltrate including plasma cells with reactive lymphoid aggregates and Russell bodies. One HPE report suggested the diagnosis of Rhinoscleroma and the other HPE report mentioned that the diagnosis of Rhinoscleroma cannot be ruled out. However no evidence of fungal elements or malignancy was seen in both HPE specimens. Nasal swab for bacterium Kleibsiella Rhinoscleromatis was negative. Nasal secretion culture did not grow any pathological bacteria. Patient was put on Tab Tetracycline 500 mg QID along with Tab Rifampicin 450mg TID for 6 weeks based on Literature data. Post operative period was uneventful. After 2 weeks of surgery the frontal sinus drain was removed. Patient was followed up at regular intervals, she remained symptoms free. A CT scan of the PNS done 2 years post op showed no recurrence of the lesion.
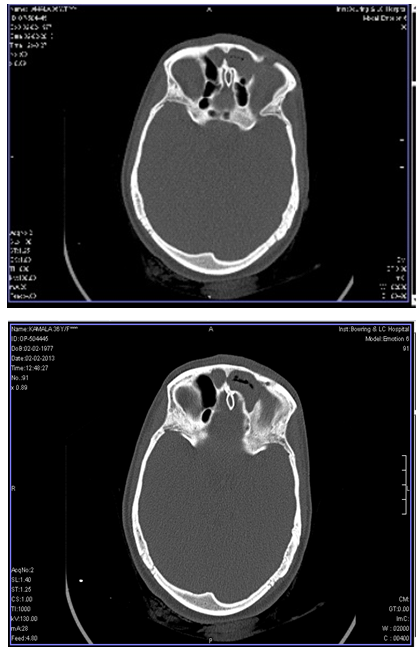 | Figure 3. Axial CT scan showing mass in the left frontal sinus with breach in the anterior wall |
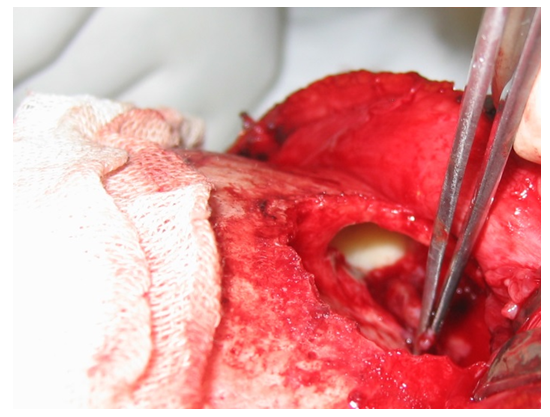
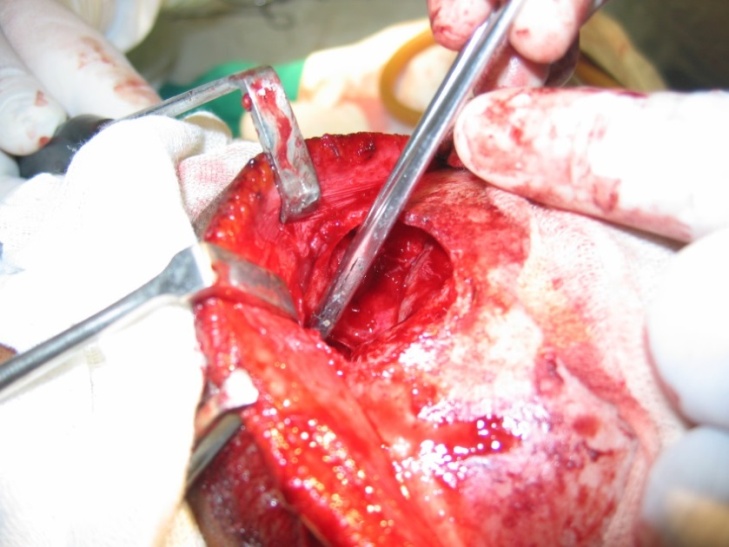 | Figure 4. Intra operative view of fleshy mass in the left frontal sinus |
 | Figure 5. Draf 3 widening of frontonasal duct |
 | Figure 6. Post operative view of the large bore soft rubber drain placed in the sinus and brought out through the left nasal cavity |
3. Case Report 3
- A 40 year old female patient presented with history of recurrent headache of many years duration, which was initially intermittent and later continuous at the time of presentation. She noticed a bulge in the right side of the forehead which was painful.CT scan PNS showed erosion of the anterior wall and a small dehiscence in the posterior table of the right frontal sinus, a mucocele was seen filling the frontal sinus completely and was more laterally placed. Endoscopic surgery was ruled out due to the extensive nature of the disease. Intra operatively on elevating the forehead flap, thinning and erosion of the anterior table was noted with a tense mucocele bulging from beneath. The thinned out frontal bone was removed and drilled to expose the frontal sinus, using a 30 degree endoscope the mucocele was dissected from its attachments, a small defect was identified in the posterior table, the margins was freshened and sealed with bone wax and the frontal sinus cavity was obliterated with abdominal fat after sealing the nasofrontal duct. The forehead flap was repositioned and stapled. Immediate post op period was uneventful. On follow up after 6 months patient was symptom free.
 | Figure 7. Intra operative view of mucocele with mucopus in the right frontal sinus |
4. Discussion
- History of frontal sinus surgeryTrephination era (1750)In 1750 Runge performed an obliteration procedure of the frontal sinus (1). In 1870 Wells described an external and intracranial drainage procedure for frontal sinus mucocele (3). In 1884 Alexander Ogston described trephination procedure, Luc described similar procedure (4).2 years later Ogston-Luc procedure was described, but failed to gain popularity due to frontal duct stenosis (5).Radical Ablation Procedures (1895)In 1895 Kuhnt described this procedure which involves removing the anterior wall of the frontal sinus, the mucosa is stripped at the level of the frontal recess and stent placed for temporary drainage (6). In 1898 Riedel/ Schenke described frontal sinus obliteration procedure was not very popular because of the resulting cosmetic deformity of the forehead (7).In 1903 Killian modified Riedel/ Schenke procedure to avoid the forehead deformity but his procedure resulted in restenosis, supraorbital rim necrosis, post-operative meningitis, mucocele and death (8).Conservative Procedures (1905)In 1908 Knapp described ethmoidectomy through the medial wall (9). In 1911, Schaeffer proposed an intranasal puncture technique to re- establish the drainage and ventilation of the frontal sinus (10). Halle described a procedure in which the frontal process of the maxilla was chiseled out, and then a burr was used to remove the floor of the frontal sinus (11).In 1914, Lothrop described a procedure to enlarge the frontal drainage pathway in a way that would prevent restenosis as well as closure as was reported with other procedures at that time (12).External Frontoethmoidectomy (1897, 1906, 1921)Between 1897 and 1906, the details of frontoethmoidectomy was described in Germany. In Anglo-American literature, Lynch (1921) (13) in the United states and Howarth (14) in the United Kingdom popularized the principle of frontal sinus floor resection and enlargement of the frontal sinus drainage. Therefore, in those countries Frontoethmoidectomy is known as Lynch and Howarth operation (15).Osteoplastic Anterior Wall Approach to the frontal sinus (1958)The osteoplastic anterior wall approach to the frontal sinus was described at the turn of the 19 th century by several authors including Brieger, Schoenborn, Winkler and later Beck and others (16). However, little attention was paid to this technique at the turn of the century, because of the concern about the difficulty of re-approximation of the bony flap to its original position. Osteomyelitis, infection of the bone was thought to be a major morbid condition of the procedure. Tato and Bergaglio in 1949 and Lyman in 1950 (17) reported on obliterating the frontal sinus for frontal sinusitis with success and no cosmetic deformity (18).Endoscopic intranasal approaches (1991)Earlier intranasal frontal sinus procedures had a high complication rate due to poor visualization. In 1990, Schaefer and Close reported on the use of the endoscope to treat 36 patients with frontal sinus disease. They performed endoscopic frontal sinusotomy with 12 patients reporting complete resolution of symptoms and 11 reporting improvement (19).Draf, in 1991, reported a series of 100 cases in which he used both a microscope and an endoscope to perform intranasal frontoethmoid surgery for frontal sinus disease. He described a concept of three procedures with a 90% success rate. He reported no complications with this endoscopic technique. All 10% of his failures had an open osteoplastic obliterative procedure. The Draf procedures were aimed at opening the frontal ostium intranasally and allowing the sinus to drain.Draf I consisted of an anterior ethmoidectomy with opening of the nasofrontal duct.Draf II in addition consists of unilateral resection of the floor of the frontal sinus.Draf III is bilateral resection of the frontal sinus floor (20).The present trend among Otorhinolaryngologists is the use of endoscope in the surgical management of frontal sinus disease due to its advantages like• lower morbidity rates, • shorter hospital stay ,• a less invasive procedure and• no external scarring.(21)A open procedure is usually reserved for patients with absent or distorted intranasal landmarks, failed endoscopic approaches, complicated frontal sinusitis, and evidence of lateral disease or posterior table erosion (22).In our study, benign conditions affecting the frontal sinus was exenterated completely, small posterior bony defects were sealed with temporalis fascia and bone wax. The disease free frontal sinus was obliterated using abdominal fat. In one case where the suspicious mass could not be completely removed the frontal sinus was not obliterated. Draf 3 widening of the frontonasal duct was done with placement of a large bore drain. The patient responded well to medications and remained symptom free. In all the three cases post operative period was uneventful.Weber et al. reported on their complications from 82 OPF with obliteration for mucopyocele, frontal sinus fracture, chronic sinusitis, and tumor. The most common complications were exposure of orbital fat (19.5%) and unintentional fracture of the frontal sinus anterior wall (19.5%). There were no sequelae from these other than temporary orbital ecchymosis. Other complications included bony flaps that were too large with concomitant dura exposure (8.5%) or too small, leading to more bony cuts for adequate access (8.5%). Late complications in this series included persistent numbness in the supraorbital and frontal region (8.5%), mucocele formation (6.8%), and persistent pain (3.4%) [23].In the comprehensive study by Hardy and Montgomery in which 250 OFSO surgeries were performed with a median follow up of 8 years, they noted a revision rate of 4%, while 93% of 208 patients reported full resolution of symptoms. Mucocele formation rate was not known as computerized imaging of the obliterated sinus was not yet available. Morbidity from OFSO primarily related to postoperative infection, abdominal wound complications, and troubling aesthetic changes of the frontal bone have been reported between 12 and 18% [24].In our experience, we had 2 cases of mucoceles involving the frontal sinus and a case of Rhinoscleroma. All 3 patients had swelling over the frontal region in the immediate post operative period, there were no delayed complications after 2 years of follow up.Our study highlights the point that: in a situation where it is not possible to access the entire breadth of frontal sinus or if the disease is more laterally placed, the osteoplastic flap procedure is an invaluable approach for complete eradication of the frontal disease by giving a wide access to the entire breadth of the frontal sinus. The use of endoscopes during the osteoplastic procedure helps minimize the necessity to create bone flap or large defect in the anterior table of the frontal sinus. Small opening to allow insertion of the endoscope and instruments is adequate to clear the frontal disease. The advantage of this small opening is that reconstruction of the anterior wall may not be required and the forehead flap alone is sufficient to close the opening without significant cosmetic deformity.
5. Conclusions
- The surgical field of Otorhinolaryngology has seen technological advancement and up-gradation from the old conventional measures of management of frontal sinus disease. The modern otorhinolaryngologist is inclined to master the newer techniques of endoscopy and microscopic procedures with better outcome. This article emphasizes the importance of osteoplastic flap surgery to the new surgeons, as the exposure of the frontal sinus and its visualization is unparalleled even with the advent of the latest technology.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML