-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2014; 3(5): 81-83
doi:10.5923/j.otolaryn.20140305.05
Button Hole Tympanoplasty
G. Shankar, Narendranath A.
Department of ENT, Vijayanagar institute of medical sciences, Bellary, Karnataka, India
Correspondence to: G. Shankar, Department of ENT, Vijayanagar institute of medical sciences, Bellary, Karnataka, India.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Tympanoplasty is one of the most common surgeries performed in Otology due to the high incidence of chronic otitis media and temporalis fascia is the most common material used for the closure of tympanic membrane perforation. Tympanoplasty can be considered the final step in the surgical conquest of conductive hearing loss and is the culmination of over 100 years of development of surgical procedures on the middle ear to improve hearing. [1] Temporalis fascia was described by Heermannin 1961 and was introduced in the United States by Storrs in 1963. [2, 3] since then temporalis fascia has been advocated and preferred for reconstruction of middle ear hearing mechanism, either alone or with ossicular reconstruction. We aim to describe and promote a simple technique of temporalis fascia graft placement wherein its placement and fixity is aided by a button hole made in the temporalis fascia graft and inserted through the handle of the malleus.
Keywords: Temporalis Fascia, Buttonhole, Tympanoplasty
Cite this paper: G. Shankar, Narendranath A., Button Hole Tympanoplasty, Research in Otolaryngology, Vol. 3 No. 5, 2014, pp. 81-83. doi: 10.5923/j.otolaryn.20140305.05.
Article Outline
1. Introduction
- The Tympanic Membrane (TM) plays a significant role in the physiology of hearing as well as in the pathophysiology of chronic inflammatory middle ear diseases. The cardinal principles of tympanoplasty have been and still are (1) control of infection through eradication of disease, and (2) reconstruction of the middle ear's sound-conducting mechanism. Autogenous grafts are readily available and preferred. Temporalis fascia contains biologically inert collagen fibers. [4] Temporalis fascia is preferred, although other autologous materials have given satisfactory results in specific situations.The overlay technique has been associated with a higher incidence of blunting of anterior sulcus and graft lateralization, which may result in significant conductive hearing loss. [1] The most widely used and accepted method is underlay graft of temporalis fasciaor sometimes perichondrium. [5] The main drawback of underlay technique, is medialisation and adherence to promontory. The technique used here, where the graft is anchored in position by the manubrium of the malleus, avoids these complications.
2. Materials and Methods
- The study included 46 patients (21 males and 25 females) who Underwent primary buttonhole tympanoplasty between august 2012 and march 2014 at the Department of Otolaryngology–Head and Neck Surgery of a tertiary care hospital. At our center, pure-tone average audiometric examination is routinely conducted before tympanoplasty.Only tubotympanic type disease with ears that have been dry for at least 3months and pure tone average of <40 dB conductive hearing loss were included in this study.
3. Technique
- The instruments [Figure-1] and steps of the operation are similar to any tympanoplasty surgery. After canal infiltration of local anesthetic (lignocaine + adrenaline) preparation, Korner’s flap is elevated. Using post auricular approach temporalis fascia graft is harvested and depending on the disease status, combined with/ without mastoidectomy.
 | Figure 1. Showing instruments used for tympanoplasty |
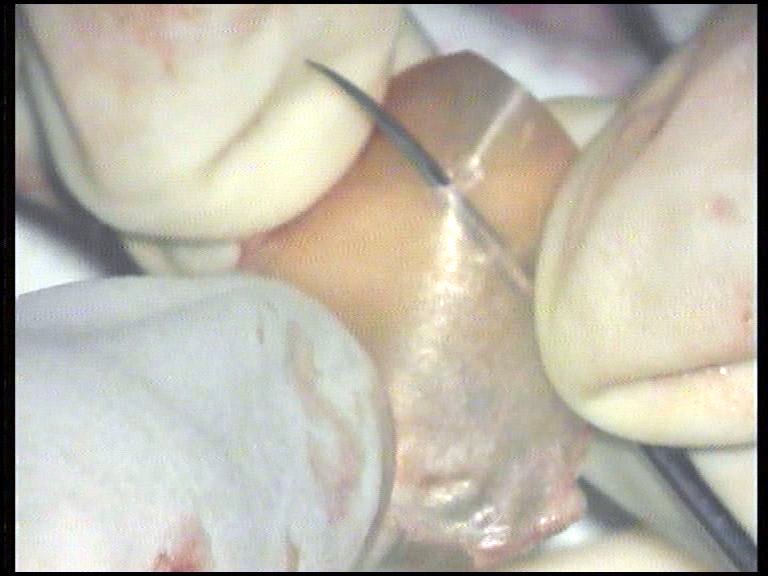 | Figure 2. Showing making of a button-hole in the fascia using a curved pick |
 | Figure 3. Showing button-hole in the temporalis fascia graft |
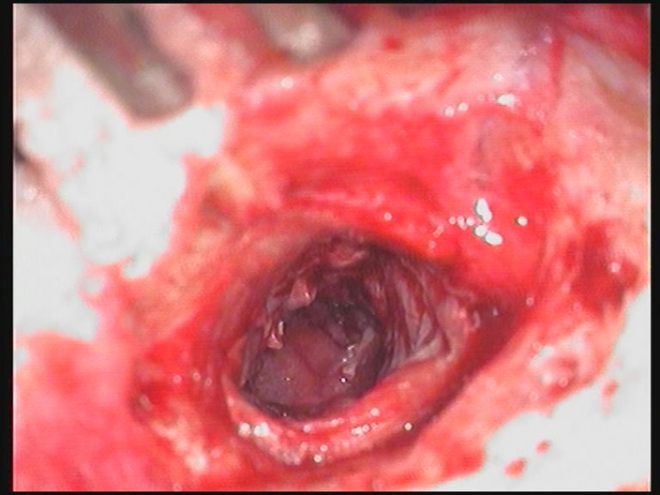 | Figure 4. Intra operative picture showing placement of graft |
4. Results
- In our study, 46 patients (46 ears) were included based on the criteria mentioned above, of which, 21 were males and 25 were females. Among these cases, 44 ears (20 males and 24 females) had significant air- bone closure to within 10-15 dB on 6month follow-up. 2 cases (1 male and 1 female) did not have satisfactory air bone closure and thus betterment of hearing. This was because of re-perforation and graft failure secondary to neglected upper respiratory tract infection in second post-op month (6th and 7th week respectively).
5. Discussion
- Temporalis fascia is the commonly used graft material for tympanic membrane reconstruction, because it is an auto graft with an excellent chance of take up, available close to the site of operation making it’s harvesting easier, a low basal metabolic rate, increased success rate, and its thickness is more or less similar to that of a tympanic membrane.Fascia is composed largely of collagen fibers. It is usually prepared by drying the tissue under a heat lamp or a hot air dryer. This makes the material cellophane-thin and more resilient to manipulation [6]. Histologically, tympanic membrane grafts become lined by squamous epithelium on the ear canal side and middle ear mucosa on the tympanic cavity side [5]. The graft itself becomes the middle or connective tissue portion of the reconstructed drum, but the orderly arrangement of concentric and radial collagen fibers as seen in the normal drum is not reconstituted in the graft [7].Lateralization and anterior blunting can occur when grafts are placed in an overlay fashion; Sheehy has suggested such grafts will have a lower "take" rate, being more prone to retract away from the anterior margin and leavinga gap [6].Gersdoff Mand Grard J-M in their text on ‘Atlas of middle ear surgery’ have described a technique of anchoring the temporalis fascia graft to the handle of malleus. [8] The technique described here is different from the above technique.The advantage of anchoring the temporalis fascia graft to the handle of the malleus through the buttonhole is:On table- On placing the graft and anchoring it to the handle of the malleus, all around (3600) movement of the graft is possible- Does not fallback over the medial wall of middle ear as it is held in position. Aids in creation of neotympanum.- It prevents inadvertent movements and displacement of the graft while maneuvering intra-operatively.- Easy to learn and follow.Post-operative-Graft lateralization and subsequent hearing loss as with overlay technique is not an issue.-With proper placement and anchoring, anterior retraction and blunting is prevented.- Because the graft is firmly held in position, chances of medial retraction and adherence to promontory are prevented.It is especially important to position the graft tightly in the anterior sulcus, where failure of graft occurs most commonly as a result of technical error. It is here that the branches of the anterior tympanic and deep auricular arteries provide a critical blood supply to the graft. [4] Numerous authors have reported that the failure rate in anterior perforations is higher. However, this failure rate can be greatly reduced by anchoring the anterior margin of the graft beneath the annulus. [9] In our study, this complication was avoided since the fascia graft was anchored to the handle of malleus. This is a new technique, and studies are needed with long term results and comparisons needed with well established techniques of underlay and overlay. One limitation of this technique is it could not be done in cases where handle of the malleus is eroded.
6. Conclusions
- Temporalis fascia grafting for tympanic membrane reconstruction has been in use since centuries now. Here we describe and promote the technique of making a buttonhole in the temporalis fascia graft and inserting the same into manubrium of malleus, thereby attaining the aforementioned benefits and reducing the incidence of complications. The authors have been successfully practicing this technique with excellent results (air-bone closure 15-20 dB) for the past 2 years.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML