C. Ravishankar, N. Dhanapala, Ruchi Rajput
Department of ENT, Bangalore Medical College and Research Institute, Bangalore, India
Correspondence to: C. Ravishankar, Department of ENT, Bangalore Medical College and Research Institute, Bangalore, India.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Abstract
The aim of the present paper is to review the success rate of Type 1 Tympanoplasty in active/discharging ear and inactive/dry ear Chronic Suppurative Otitis Media. Literature reviewed in Medline and other database. Prospective case control, prospective case series, prospective cohort studies, retrospective studies reviewed. Tympanoplasty is a routine procedure but the effect of many factors which influences the success rate remains unresolved. These factors include, age of the patient, site and size of the perforation, duration of the ear being dry prior to surgery and the presence or absence of infection at the time of surgery. The discharging ear presents to the otologist the dilemma of whether to operate on it or not. This is due to the widespread belief that the success rate of Tympanoplasty on wet ears is inferior to that of the dry ears.
Keywords:
"Tympanoplasty", "Myringoplasty", "Wet ear", "Dry ear", "Chronic suppurative otitis media" and "Tubotympanic"
Cite this paper: C. Ravishankar, N. Dhanapala, Ruchi Rajput, A Review of Results of Type I Tympanoplasty in Active and Inactive Tubotympanic Chronic Suppurative Otitis Media, Research in Otolaryngology, Vol. 3 No. 5, 2014, pp. 77-80. doi: 10.5923/j.otolaryn.20140305.04.
1. Introduction
The repair of the tympanic membrane dates back to more than a century. In 1878, Berthold successfully closed a perforation with a full thickness skin graft and introduced the term "myringoplastik" [1].Type 1 Tympanoplasty refers to any operation involving reconstruction of the tympanic membrane defect along with elimination of disease, if any, from the middle ear. A perforation in the tympanic membrane can result from either trauma or infective process; out of which the infective or suppurative process is the most common cause. Most of these perforations usually heal spontaneously. But this spontaneous healing is affected by chronicity of infection and certain patho-physiological changes at the perforation margins, leading to a non-healing permanent perforation. This leads to constant exposure of middle ear for reinfection and hearing disability. The main aim of surgery in Chronic Suppurative Otitis Media is to eliminate disease process and reconstruct middle ear to give the patient a dry, safe and functioning ear. Success rate in the range of 95% are frequently quoted in various studies. There are many factors which influence this success rate, including age of the patient, site and size of the perforation, duration of the ear being dry prior to surgery and the presence or absence of infection at the time of surgery. Discharging ear at the time of surgery is one of them. The main objective of this review is to find the effect of this discharge from the ear on the success of type I tympanoplasty from the available literature and use it to formulate prospective studies further research on this topic.
2. Methods
An extensive search of the literature was performed in Medline, PubMed and Science direct databases, using the keywords "tympanoplasty", "myringoplasty", "wet ear", "dry ear", "chronic suppurative otitis media" and "tubotympanic". The keywords "tympanoplasty" and "myringoplasty" were considered primary and were combined to each of the other keywords individually. In addition, reference lists from the retrieved articles were manually searched. Language restrictions limited the search to English language articles only. Information from standard related books was also included in the analysis of data.
3. Results
Five prospective controlled studies, one prospective cohort, one prospective case series and three retrospective studies met the defined criteria and were included in study selection. The criteria for inclusion being studies done to evaluate the factors influencing the results of type 1 tympanoplasty in adults. We excluded those studies which were done in pediatric population, those done on failure of primary surgeries and tympanoplasties other than type 1.The success rate of Type 1 Tympanoplasty depended upon various factors. The studies analyzing these factors are listed in the Table 1. | Table 1. Studies analyzing various factors affecting outcome of Tympanoplasty |
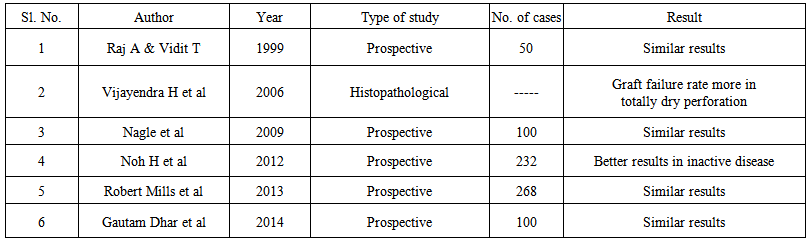
There are a few studies in literature analyzing the influence of discharging ear on the success rate of Type 1Tympanoplasty (Table 2).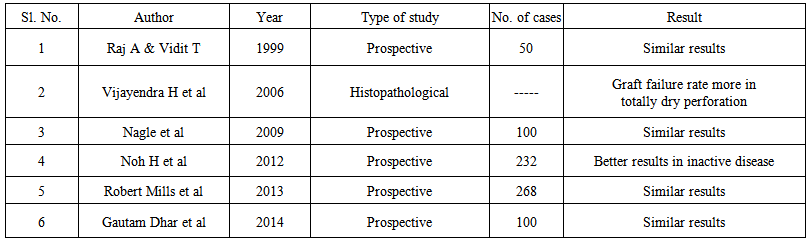 | Table 2. Studies analyzing results of Tympanoplasty in active and inactive ears |
Warren Y et al, 1984; did a retrospective study in 71 cases for analysis of various factors influencing the success rate. Type I Tympanoplasty with temporalis fascia graft was done by underlay technique. The overall success rate was 89%. The two factors which adversely influenced the success rate were the presence of a near total or total perforation and the presence of bilateral perforations. The age of the patient, the length of time the ear had been dry, and the presence of infection at the time of surgery had no influence on the success rate. [3]Fadl et al, 2003; did a retrospective study in 97 patients to study the factors presumed to influence the outcome of surgery and included age, sex, nationality, affected ear, middle ear status at surgery, perforation size and surgical approach and techniques chosen by different surgeons. The data was collected in a set out proformae and tables and analyzed and discussed. The middle ear status at surgery whether wet (6.2%) or dry (93.8%) showed nearly similar results of success. (83.3% and 84.6% respectively). [6]Zakaria Sarker et al, 2011; did a prospective study to evaluate the factors that affect the graft take rate as well as hearing improvement after myringoplasty. In this study 60 patients were divided into several groups based on 4 factors like size of perforation (small, medium and large), site of perforation (anterior central, posterior central and central malleolar), Condition of the middle ear (dry & wet) and surgical approach (post auricular and transcanal). Surgical outcome of myringoplasty was measured on the basis of graft take rate and post-operative hearing improvement. The results showed that the condition of middle ear at the time of operation affects the surgical outcome. Graft take rate was 89.36% in dry perforation and 53.85% in wet perforation. Graft take rate was greater in dry perforation. Closure of air-bone gap was 18.23 dB and 7.8 dB in dry and wet perforation respectively. Hearing improvement was greater in dry perforation. [8]Raj A and Vidit T, 1999; did myringoplasty under local anesthesia on 50 patients with 'wet ear' by underlay technique using temporalis fascia graft. Wet ear was meant as mucoid discharge only. A result of primary closure of 84 percent of the perforations, which was similar to that seen in dry ears, was observed. Hearing improvement was seen in 68 percent of the patients. The incidence of complications was also low and similar to that seen in the dry ears. [10]Vijayendra H et al, 2006; found that the failure rate in totally dry ear Tympanoplasty was more as compared to wet Tympanoplasty. Histopathological study of both dry and wet remnant tympanic membrane was done and findings were compared. In wet perforation, all the layers of tympanic membrane were present along with abundant blood vessels and increased number of inflammatory cells. While in dry perforation, only single layer of epithelium was present along with scanty or absent blood vessels and inflammatory cells. Due to these findings it was inferred that graft failure rate was more in totally dry perforation than in wet central perforation and mainly because of the avascularity of remnant tympanic membrane in totally dry central perforation. It was further observed that such types of failures can be prevented, if (i) the central perforation is converted to subtotal perforation by removing the necrotic portion of the TM, (ii) stabilization of the underlay graft by antero-superior anchoring myringoplasty in which a window in the anterior canal skin is made at about 3 O'clock position in right ear & 9 O'clock position in left ear and the graft is tucked under it. [11]Nagle et al, 2009; conducted a study to compare surgical outcome of Type1Tympanoplasty in dry and wet ears. Wet ear meant that the patient had a mild mucoid discharge which was negative on culture. In this case study of 100 patients, 50 patients had wet ear and 50 patients had dry ear. Type 1 Tympanoplasty was done in all patients under local anesthesia using temporalis fascia graft and by underlay technique. In dry ear, complete graft uptake was seen in 44 (88%) patients and in wet ear complete graft uptake was seen in 37 cases (74%), with p value 0.07 (p > 0.05) which was statistically insignificant. They concluded that the presence of discharge in the ear at the time of operation did not interfere with the results of Tympanoplasty, but only when the discharge was mucoid and scanty. [12] Saeed A et al, 1994; analyzed various factors that might influence the success rate, such as status of middle ear, size and site of perforations, surgical approach and presence of tympanosclerosis. In this study, 12 of 62 patients who failed primary surgery had discharging ears (mucopurulent) at the time of surgery despite intensive treatment pre and postoperatively. No patient with a discharging ear had a successful surgery. [5]Noh H et al, 2012; did a prospective study to evaluate the vascularization process of the grafted fascia or perichondrium in active and inactive chronic mucosal otitis media. In this study 232 patients underwent Type1 Tympanoplasty or myringoplasty by a single experienced surgeon. Postoperative otorrhoea was higher in patients with a preoperative wet middle ear mucosa than among those with a dry one. [13]These two studies observe similar results in that the discharging ear and larger perforations have poorer success and also success rates are better when surgeries are done by more experienced surgeons.Robert Mills et al, 2013; did a case series study to determine whether the presence of aural discharge at the time of surgery adversely affected the success rate of myringoplasty operations. Of the 268 operations carried out, 203 were successful, with an intact tympanic membrane. 6 months postoperatively, 43 had persistent perforations, and 22 patients were lost to follow-up before 6 months. The success rates for closure of the perforation at 6 months after surgery were 83% for inactive and 82% for active ears (P = .9). Hence it was concluded that there was no clinically significant difference in the success rate for Type 1 Tympanoplasty in patients who had active discharge at the time of surgery. [14]Gautam Dhar et al, 2014; did a prospective case control study on 100 patients of chronic suppurative otitis media with central perforation (50 dry and 50 wet perforations). Wet ear had culture negative mucoid discharge. Graft take up rate of both the groups were compared following myringoplasty. There was no significant difference in the success rate for both the groups. [15]
4. Discussion
Only three studies, selected in this review among total of ten, claim that the success of Type 1Tympanoplasty is lesser when discharging ear is operated upon. [5, 8, 13] Rest of the studies agree that there is no statistically significant influence of active /discharging ear on the success rate of Type1Tympanoplasty [3, 6, 10, 12, 14, 15]. The study of Vijayendra et al [11] is interesting in that, the surgeries in discharging ears were having better results compared to surgeries on dry ears. Remnant tympanic membranes of both the groups were subjected to histopathological examination and it was noted that presence of increased vascularity and inflammatory infiltrates were found to be the reasons for better results in the discharging ears. They also suggest that in dry ears, the atrophic portion of the remnant tympanic membrane has to be removed thereby converting all perforations into subtotal perforations, which improved the success rate in their series.All studies in this review are of the opinion that, age, gender, duration of the discharge, size or site of the perforation and condition of the middle ear do not affect the success rate of type1 Tympanoplasty. However it is notable that the anterior perforations required special care while operating, to secure the anterior edge of graft between the bony anterior canal wall and its skin (anterior tucking).
5. Conclusions
Type1Tympanoplasty on wet or discharging ears has little effect on the success rate. (Most of the studies in this review concluded that there is no impact of discharge or active mucoid discharge on the success of Type1 Tympanoplasty.) Further, the results are even better in discharging ear as supported by histopathological evidence. In this review, wet ear meant mucoid and scanty discharge and there was no study which commented about surgery on ears with purulent discharge. This aspect needs to be investigated and validated by a randomized control trial which takes both histopathological and microbiological evidence into consideration.
References
| [1] | George G Browning. Chronic otitis media: The Ear, Hearing And Balance. Chapter 237e: Scott-Brown's Otorhinolaryngology, Head and Neck Surgery: 7th edition; page 3412-3423. |
| [2] | Berthold E. Myringoplastik zeitschrift fur. Ohernheilkunde 1978;12:134. |
| [3] | Warren Y et al. Type I Tympanoplasty: Influencing factors. The Laryngoscope, vol 94 (7): July 1984, 916-918. |
| [4] | Vartianen E et al. Success and pitfalls in myringoplasty: follow-up study of 404 cases. Am J Otol. 1993 May; 14(3): 301-5. |
| [5] | Saeed A. Tympanoplasty: factors influencing surgical outcome. Annals of Saudi Medicine, vol 14, no.6, 1994, 01-04. |
| [6] | Fadl A Fadl. Outcome of Type 1Tympanoplasty. Saudi Med J 2003; vol.24 (1): 58-61. |
| [7] | Wasson JD et al. Myringoplasty: impact of perforation size on closure and audiological improvement. J Laryngol Otol. 2009 September; 123(9): 973-7. |
| [8] | Zakaria Sarker et al. Factors affecting surgical outcome of myringoplasty. Bangladesh J Otorhinolaryngol. 2011; 17(2): 82-87. |
| [9] | Migirov L et al. Does smoking influence the surgical outcome of a myringoplasty? ORL J Otorhinolaryngol Relat Spec. 2013; 75(4): 207-10 |
| [10] | Raj A and Vidit T. Review of patients undergoing wet myringoplasty. Indian J of Otol. Vol 5, no.3, september 99; 134-136. |
| [11] | Vijayendra H et al. Comparative study of Tympanoplasty in wet perforation v/s totally dry perforation in tubotympanic disease. Indian J of Otolaryngol Head NeckSurg. Vol 58, no.2 April-June 2006; 165-167. |
| [12] | Nagle et al. Comparative study of outcome of type I Tympanoplasty in dry and wet eat. Indian J Otolaryngol Head Neck Surg. (April- June 2009) 61: 138-140. |
| [13] | Noh H et al. Vascularisation of myringo-/tympanoplastic grafts in active and inactive chronic mucosal otitis media: a prospective cohort study. Clin Otolaryngol. Vol 37(5); 355-361. Oct 2012. |
| [14] | Robert Mills et al. Results of myringoplasty operations in active and inactive ears in adults. The Laryngoscope. vol. 123(9): 2245-2249, Sep 2013. |
| [15] | Gautam Dhar et al. Outcome of myringoplasty in dry and wet ear- a comparative study. IOSR Journal of Dental and Medical Sciences. Vol. 13(3), Ver V, (March 2014), pp 01-03. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML