-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Otolaryngology
p-ISSN: 2326-1307 e-ISSN: 2326-1323
2014; 3(4): 60-63
doi:10.5923/j.otolaryn.20140304.03
Tornwaldt’s Cyst, Tornwaldt’s Bursitis and Tornwaldt’s Disease: A Review
Maliyappanahalli Siddappa Vijayashree, Borlingegowda Viswanatha
Otorhinolaryngology Department, Bangalore Medical College & Research Institute, Bangalore, India
Correspondence to: Borlingegowda Viswanatha, Otorhinolaryngology Department, Bangalore Medical College & Research Institute, Bangalore, India.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Tornwaldt’s cystis an uncommon type of nasopharyngeal cyst that may cause significant clinical symptoms. It was described by Tornwaldt in 1885.This is a rare benign disorder induced by persistent notochord remnants. Tornwaldt’s cysts are almost always asymptomatic. The diagnosis of this mass is usually incidental as a part of a nasal endoscopic examination or they may be detected on radiological examination. The aim of this review article is to present 3 cases [Tornwaldt’s cyst, Tornwaldt’s bursitis and Tornwaldt’s disease] along with review of literature.
Keywords: Tornwaldt’s cyst, Tornwaldt’s bursitis, Tornwaldt’s disease
Cite this paper: Maliyappanahalli Siddappa Vijayashree, Borlingegowda Viswanatha, Tornwaldt’s Cyst, Tornwaldt’s Bursitis and Tornwaldt’s Disease: A Review, Research in Otolaryngology, Vol. 3 No. 4, 2014, pp. 60-63. doi: 10.5923/j.otolaryn.20140304.03.
Article Outline
1. Introduction
- Tornwaldt’s cyst occurs in the midline bursa of the nasopharynx above the upper border of the superior constrictor muscle [1]. They develop as result of abnormal embriyologic development at the posterior wall of the nasopharynx [2]. A German physician, Gustavust L. Tornwaldt [3] published a 119-page monograph in which he described the development of nasopharyngeal cyst from the bursa. He described the clinical symptoms caused by the accumulation of fluid in these cysts and the infection of the cysts [1]. Tornwaldt’s cyst is a rare benign disorder induced by persistent notochord remnants. The contact between these remnants and pharyngeal ectoderm creates the condition for the in growth of respiratory epithelium, which forms the Tornwaldt’s bursa [4-6], which drains in to the nasopharyngeal cavity. This bursa develops in to a cyst only in when the orifice is partially or totally obstructed as result of infection or after adenoidectomy [4]. A Tornwaldt's cyst may progress to Tornwaldt's disease if it becomes infected or inflamed and produces symptoms such as Eustachian tube dysfunction, otitis media, halitosis, pharyngitis, and occipital headache. [2, 4, 7, 8, 9]. In this review article 3 cases [Tornwaldt’s cyst, Tornwaldt’s bursitis and Tornwaldt’s disease] is presented along with review of literature.
2. Case Reports
2.1. Case 1
- A 36 years old male patient was referred to otolaryngology department for the evaluation of a nasopharyngeal cystic mass found on CT scan. Patient had visited neurologist for treatment of migraine. Incidentally CT scan showed a small cystic mass in the nasopharynx [figure-1].
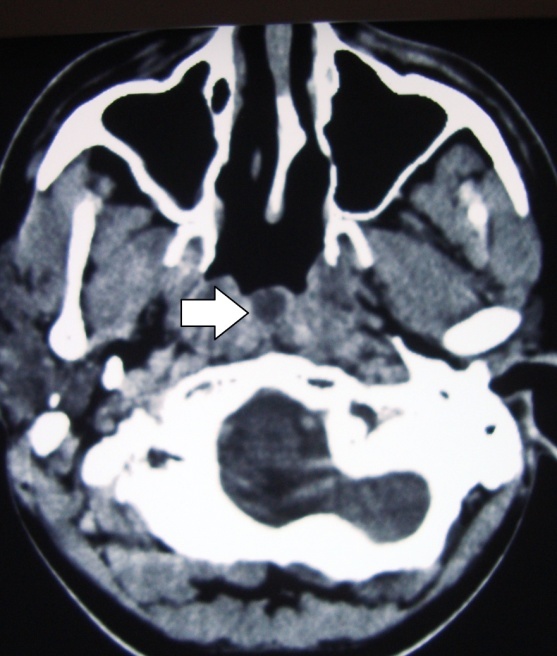 | Figure 1. CT scan picture showing a cystic mass (arrow) in the nasopharynx |
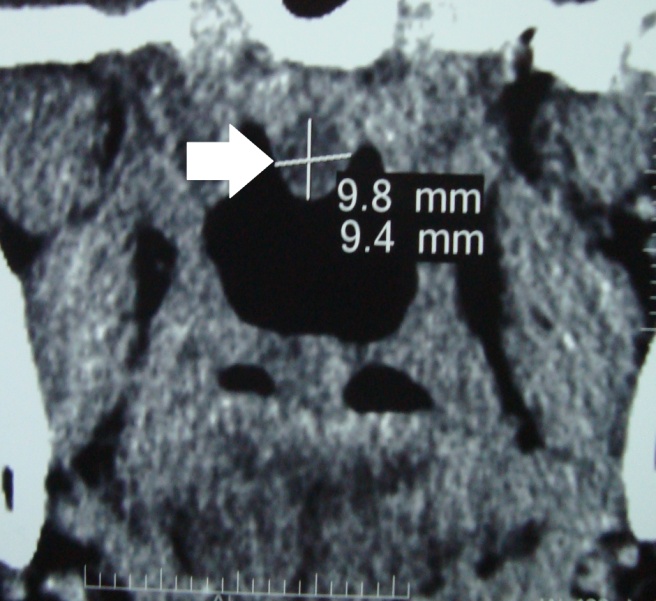 | Figure 2. CT scan picture showing a cystic mass (arrow) in the nasopharynx |
2.2. Case 2
- A 54-year old woman came with history of recurrent attacks of halitosis and occasional purulent discharge from the nasopharynx for the past six months. Patient used to get complete relief with antibiotics therapy. On ear nose and throat examination except for a small postnasal discharge there were no significant findings. Diagnostic nasal endoscopy showed a cystic mass in upper part of the posterior nasopharyngeal wall and there was a mucopurulent discharge from the large opening in the upper part of the mass. Discharge was sent for culture and sensitivity and there was no microbial growth. The endoscopic findings were suggestive of infected Tornwaldt’s bursitis. MRI showed an hour glass shaped lesion with a fluid level and it was in communication with the nasopharynx [figure-3].
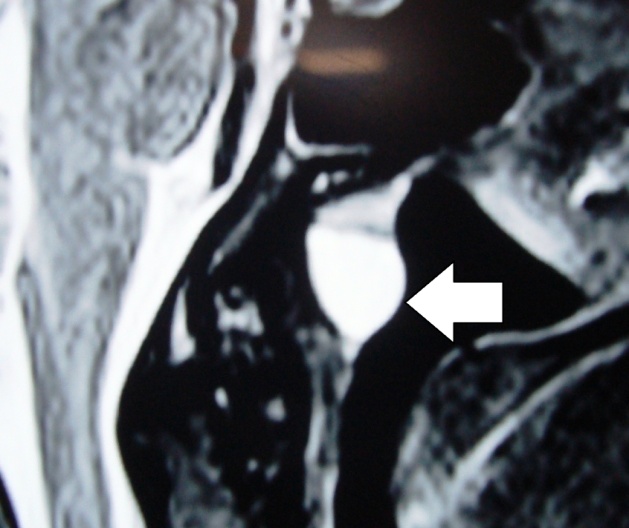 | Figure 3. MRI picture showing a cystic mass (arrow) in the nasopharynx and fluid level |
2.3. Case 3
- A twenty two year male patient presented with history of recurrent attacks of epistaxis through the left nostril for the past 3 months. During each attacks patient used to have small quantities of unprovocative nasal bleed on the left side and it used to subside without any medication. Nasal examination deviation of the nasal septum to the left and post nasal examination showed congestion in the postero-superior part of the nasopharyngeal wall. Ears and throat examinations findings were normal. Diagnostic nasal endoscopy showed a congested cystic mass in the midline of the upper part of the posterior nasopharyngeal wall [figure-4].
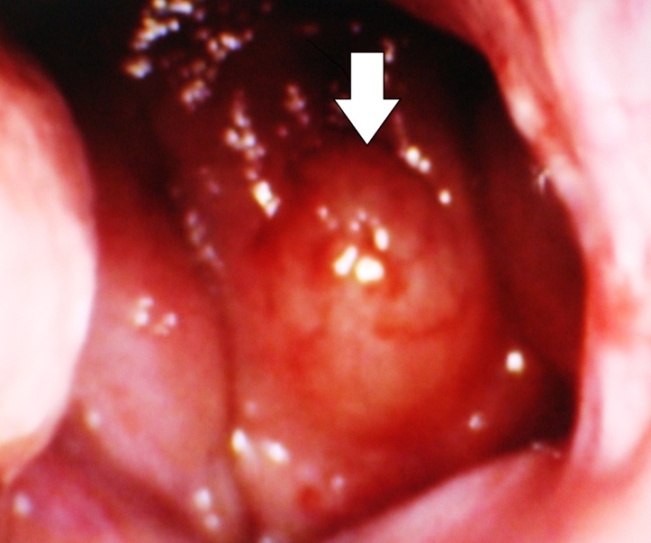 | Figure 4. Endoscopic picture showing a cystic mass (arrow) in the nasopharynx |
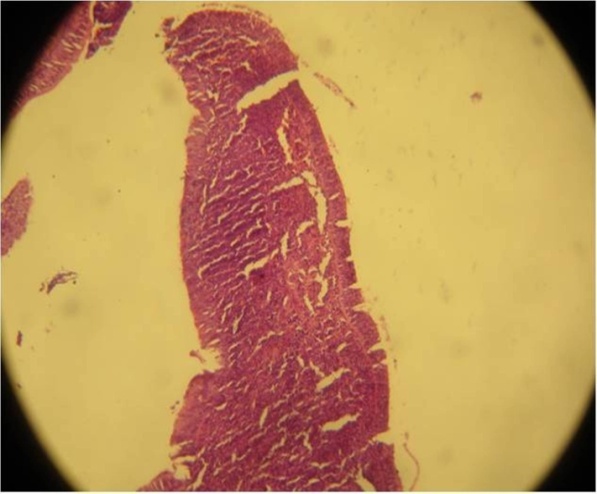 | Figure 5. Microphotograph of cyst wall showing respiratory epithelium |
3. Discussion
- Tornwaldt’s cyst occurs in the midline of the nasopharynx above the upper border of the superior constrictor muscle. They represent a communication between the notochordal remnant and the pharyngeal endoderm [1]. This cyst was noted in autopsy specimen by Mayer [10] in 1940. And it was established as a pathologic entity by a German physician, Gustavust L. Tornwaldt [3] in 1885. Huber [11] later described how irregular notochord regression in the sixth week of gestation leads to its formation. Usually Tornwaldt’s cyst is asymptomatic. Its incidence is 4% in autopsy specimens. On routine MRI done for other disorders showed incidence of 0.2% to 5% [4, 12].Tornwaldt's cysts are classified as crusting and cystic. The crusting types regularly and spontaneously drain into the nasopharynx; the cystic types do not drain because the drainage pathway is completely obstructed [2, 12]. In the present study first patient had clinically asymptomatic cyst, second patients had crusting type of cyst and third patient had cystic type.There is a controversy regarding the true aetiology of Tornwaldt's cyst. Classically it is described as a notochord remnant and some are of the opinion that it is an iatrogenic occlusion of normal structure after adenoidectomy or chronic inflammation [13]. A case of Tornwaldt's cyst formation has been reported after concurrent chemoradiotheraphy for nasopharyngeal carcinoma [14]. In the present study all the three patients had not undergone adenoidectomy.In authors institution more than 500 adenoidectomies have been done over the past 15 years. There are only three reported cases of Tornwaldt's disease/cyst and all the three patients had not undergone adenoidectomy. It is unlikely that adenoidectomy can be the cause of this rare entity.It is usually asymptomatic. Symptoms can arise due to the Tornwaldt's cyst or inflammation of the Tornwaldt's bursa or as a result of Tornwaldt's disease [1, 4]. Symptoms appear after the spontaneous drainage into the nasopharyngeal cavity or as a result of involvement of nervous plexus in the site. Symptoms are occipital headache, cervical myalgia, halitosis and middle ear effusion [4]. When Tornwaldt's cyst is enlarged and inflamed, patients may present with nasal obstruction, headache, postnasal discharge with foul smelling odour, Eustachian tubes obstruction causing otalgia, secretary otitis media [1]. They may also present with retro orbital pain [13]. In the present study second patient had symptoms due infection and inflammation of Tornwaldt’s bursa. Diagnostic nasal endoscopy showed a cystic mass in upper part of the posterior nasopharyngeal wall and there was a mucopurulent discharge from the large opening in the upper part of the mass. MRI showed an hour glass shaped lesion with a fluid level upper part of the posterior nasopharyngeal wall and it was in communication with the nasopharynx. To best of our knowledge this is the first reported case of Tornwaldt's bursitis. In third case patient presented with only recurrent episodes epistaxis and he did had any other symptoms. Review of literature did not show any case reports of Tornwaldt’s disease with epistaxis as a presenting symptom. To best of our knowledge this is the first reported case of Tornwaldt's disease which presented only with epistaxis.Nasal endoscopic examination is required for the clinical diagnosis. On endoscopic examination, cyst appears as solitary midline smooth surfaced mass on the posterior wall of the nasopharynx and size may vary from few millimetres to two centimetres. Sometimes an opening through which the cyst drains periodically may be visible [4]. In the present case series all the patients underwent diagnostic nasal endoscopy and only in the second patient wide opening over the cyst was visible.Tornwaldt's cyst appears as solid mass on CT scanning. It is hyper intense on T1-weighted and T2- weighted MRI [4]. This is because of high protein content or of the cyst or due to haemorrhage within the cyst.MRI is the best imaging study for diagnosing Tornwaldt's cyst. They do not enhance with intravenous contrast. In a study by Marcus Mundy et al [2], the average size of the Tornwaldt's cysts seen on MRI was found to be smaller than that of the cysts seen on CT. In our second case MRI was showed bursa with fluid inside. These findings were suggestive of the inflammation of the Tornwaldt’s bursa [Tornwaldt’s bursitis].Tornwaldt's cysts should be differentiated from the typical nasopharyngeal disorders such as Rathke’s pouch, adenoid retention cyst, meningocoele, meningoencephalocoele, branchial cleft cyst. Malignant tumours, shenochoanal polyps [1, 4].Tornwaldt's cysts are treated surgically. Asymptomatic cysts do not require any treatment and symptomatic cysts requires surgical treatment. Transnasal endoscopic marsupialization is the best way of surgical treatment because it provides precise visual control during the operative procedure [4]. This can be accomplished transnasally with a nasal endoscopes and microdebrider [1].
4. Conclusions
- Tornwaldt's cysts are uncommon clinical entity. Since they are uncommon it may go undiagnosed as the source of several common ENT complaints. MRI is the best imaging study for diagnosing Tornwaldt's cysts. Transnasal endoscopic marsupialization is the preferred way of treatment because it is safe, fast and provides good visualization during surgery.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML