Borlingegowda Viswanatha, Sahana Durganna, Rasika Ravikumar, Maliyappanahalli Siddappa Vijaya, Priyadarshini Vincent
Otorhinolaryngology department, Bangalore medical college & research institute, Bangalore, India
Correspondence to: Borlingegowda Viswanatha, Otorhinolaryngology department, Bangalore medical college & research institute, Bangalore, India.
| Email: |  |
Copyright © 2014 Scientific & Academic Publishing. All Rights Reserved.
Abstract
Background: Chronic otitis media (COM) is a commonly encountered infection of the middle ear. It is one of the most common diseases of the ear of all age groups. It is a disease of the poor and a major health problem in developing countries causing serious local damage and threatening complications especially in the unsafe type with cholesteatoma. Anomalous proliferation of the cholesteatoma epithelium is caused by extrinsic factors such as toxins or bacterial antigens combined with lytic enzymes, lymphokines and cytokines released from the inflammatory infiltrate. This could explain the close relationship between the aggressiveness of cholesteatoma and repeated bacterial superinfection, therefore it is very important to know the bacteria involved in order to control the regrowth of skin following surgery, reduce the aggressive potential of the cholesteatoma and limit the incidence of complications. Early and effective treatment based on the knowledge of causative micro-organisms and their antimicrobial sensitivity ensures prompt clinical recovery and possible complications can thus be avoided.Aims & Objectives: The aim of the study was to determine the microbial organisms associated with active squamous type of chronic otitis media with complications.Material & methods: A total of 81 patients with discharging ear with extracranial or intracranial complication were enrolled in the study. As some had bilateral ear discharge, the study had 100 discharging ears. Pus for culture and sensitivity was obtained separately from each ear using sterile cotton swabs and sent for aerobic and anaerobic culture.Results: Pure growth was obtained in 50 (61.7%) patients, mixed growth in 12 (14.8%) patients and no growth in 19 (23.5%) patients. The most common organism isolated was Pseudomonas (35.8%), followed by Proteus (16%) and Staphylococcus aureus (12.3%). Of 81 patients, 40 (49.4%) had extracranial complications, 22 (27.1%) had intracranial complications and 19 (23.5%) had both intracranial and extracranial complications. The most common organisms isolated in patients with extracranial complications were Pseudomonas (40.7%), Staphylococcus aureus (15.3%), Proteus (8.5%), Streptococci (6.9%), Klebsiella (5%), E.coli (3.4%), Peptostreptococci (1.7%) and Bacteroids with Non-hemolytic streptococci (1.7%). The most common organisms isolated from patients with intracranial complications were Proteus (26.8%), Pseudomonas (24.4%), Peptostreptococci (9.7%), Bacteroids (9.7%), Staphylococcus aureus (4.8%), E.coli (4.8%), Streptococci (4.8%) and Klebsiella (2.4%). The aerobic and anaerobic bacteria isolated were all sensitive to 3rd & 4th generation cephalosporins, fluoroquinolones and aminoglycosides. Few showed resistance to penicillins and 1st generation cephalosporins.Conclusion: Knowledge about the most common organisms causing chronic otitis media with complications can help to prevent the same and the antibiotic sensitivity pattern should guide in appropriate management of COM and halt the progression of complication at an early stage. In our study, we found that Pseudomonas and Proteus were the most common organisms involved in patients with complications.
Keywords:
Bacteriology, Active squamous type, Chronic otitis media, Complications
Cite this paper: Borlingegowda Viswanatha, Sahana Durganna, Rasika Ravikumar, Maliyappanahalli Siddappa Vijaya, Priyadarshini Vincent, Bacteriology of Active Squamous Type of Chronic Otitis Media with Complications, Research in Otolaryngology, Vol. 3 No. 2, 2014, pp. 9-15. doi: 10.5923/j.otolaryn.20140302.01.
1. Introduction
Chronic suppurative otitis media (CSOM) is defined as chronic inflammation of middle ear and mastoid cavity that may present with recurrent ear discharges or otorrhoea through a tympanic perforation. CSOM is usually classified into two types, tubotympanic and attico-antral depending on whether the disease process affects the pars tensa or pars flaccida of the tympanic membrane. Tubotympanic is called as a safe type or benign type as there is no serious complication whereas, attico-antral is called as the unsafe or dangerous type because of associated complication and may be life threatening at time [1].With the advent of Otomicroscopy, the older anatomical classification into tubo-tympanic and attico-antral types has been replaced by mucosal chronic otitis media and squamous chronic otitis media. The earlier denomination of safe and unsafe type is also considered obsolete as complications can occur in any type of chronic otitis media. Earlier chronic suppurative otitis media was the general term used for chronic middle ear infections. It has been replaced by the term chronic otitis media (COM) as it can also exist without suppuration. Chronic otitis media is thus classified as Active COM (earlier chronic suppurative otitis media), Inactive COM and Healed COM [2].According to one theory, anomalous proliferation of the cholesteatoma epithelium is caused by extrinsic factors such as toxins or bacterial antigens combined with lytic enzymes, lymphokines and cytokines released from the inflammatory infiltrate. This could explain the close relationship between the aggressiveness of cholesteatoma and repeated bacterial superinfection. The most frequently identified bacteria in cholesteatoma otitis are Pseudomonas aeruginosa, Staphylococcus aureus, Proteus and anaerobic gram-positive cocci (AGPC) [3].The knowledge of bacterial etiology of COM is very important for the clinicians for appropriate management of the cases, to prevent or minimise the occurrence of complications and prevent emergence of resistant strains [4].Recognizing the need for awareness of the current pattern of bacterial pathogens isolated from COM with complications in our setting, we conducted a study to identify the common bacterial isolates from patients diagnosed with chronic suppurative otitis media with extracranial or intracranial complication(s) at Sri Venkateshwara ENT Institute, Victoria hospital and to determine the antibiotic sensitivity pattern of these bacterial isolates to commonly used antimicrobials.Our results are shown in comparisons with other studies on bacteriology of chronic otitis media [5 -11] in table 1.Table 1. Comparison of results of various studies
 |
| |
|
2. Material and Methods
This study was carried out in Sri Venkateshwara ENT Institute, Victoria hospital, a tertiary care hospital, from January 2008 to 2013. Overall 81 patients, diagnosed to have chronic otitis media with extracranial or intracranial complications were included in the study. As some had bilateral ear discharge, the study had 100 discharging ears. Written informed consent was taken from all patients included in the study.Inclusion Criteria:1. Patients presenting with chronic ear discharge for more than 6-12 weeks.2. Patients with cholesteatoma formation on clinical examination, confirmed by Otomicroscopy and radiologic examination3. Patients with extracranial or intracranial complications of COM (mastoiditis, petrositis, facial nerve paralysis, Labyrinthine fistula, post auricular abscess or fistula, meningitis, lateral sinus thromblophlebitis, brain abscesses, otitic hydrocephalus etc).Exclusion Criteria1. Patients without any written informed consent.2. Patients with other serious medical conditions such as immunodeficiency states, malignancy 3. Patients with mucosal chronic otitis media and patients with inactive retraction pockets without cholesteatoma.4. Patients with history of previous surgery in the complaining ear.Material for analysis was collected by examination under microscope using a sterile cotton swab, taking care to avoid contamination of the skin of the external auditory canal. The samples were immediately sent to the microbiology laboratory for aerobic and anaerobic culture and necessary bacteriological processing. Separate swabs were taken from either ear in case of bilateral disease.The samples were immediately cultured in Blood Agar, Chocolate agar and Macconkey’s media for aerobic culture and in Robertsons Cooked Meat media for anaerobic culture. The culture plates were incubated at 37℃ for 24 to 48 hours. The isolates were identified by Gram’s staining and characteristic tests according to the conventional methods. An antibiotic sensitivity pattern was obtained by using Modified Kirby Bauer’s disc diffusion method.
3. Observation and Results
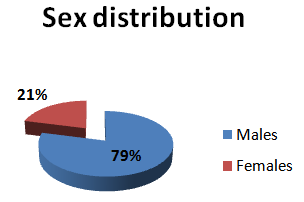
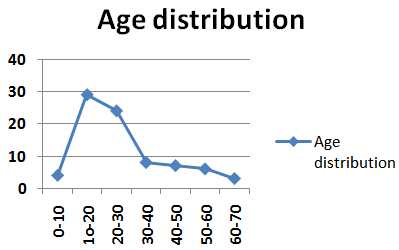
Of the 81 patients who had complications of COM, 71 had unilateral squamous disease (9 of them had mucosal disease in the opposite ear) while 10 had bilateral squamous disease. Most of the patients belonged to the younger age group between 10-19 years (35.8%) and 20-29 years (29.6%). Together, 10-30 years age group constituted 65.4% of our study group i.e. patients with complications of CSOM. The youngest patient was 5 years old while the oldest was 65 years old (Figure 1). Majority (64) of the patients were males with only 17 females in the study group (Figure 2).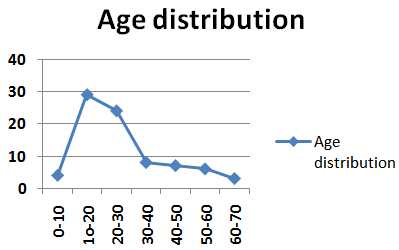 | Figure 1. Showing sex distribution |
 | Figure 2. Showing sex distribution |
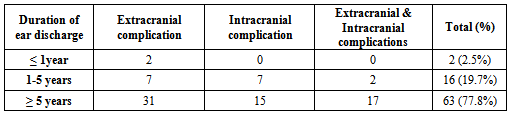
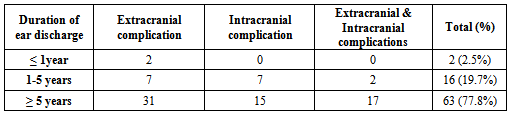
Of 81 patients, 40 (49.4%) had extracranial complications, 22 (27.1%) had intracranial complications and 19 (23.5%) had both intracranial and extracranial complications. We analyzed the effect of duration of ear discharge on the occurrence of complications (Table 2) and found out that 77.78% of the patients (with extracranial or intracranial complications or both) had duration of ear discharge for ≥ 5 years.Table 2. Showing distribution of duration of ear discharge
 |
| |
|
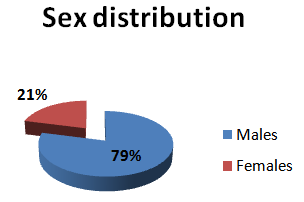
Pure growth was obtained in 50 (61.7%) patients, mixed growth in 12 (14.8%) patients and no growth in 19 (23.5%) patients (Figure 3). The most common organisms isolated were Pseudomonas aeruginosa (35.8%), Proteus mirabilis (16%) both being Gram negative and Staphylococcus aureus (12.3%) which is a Gram positive cocci (Figure 4). | Figure 3. Showing distribution of yield of culture |
 | Figure 4. Showing the predominance of gram negative isolates and significant proportion of anaerobes |
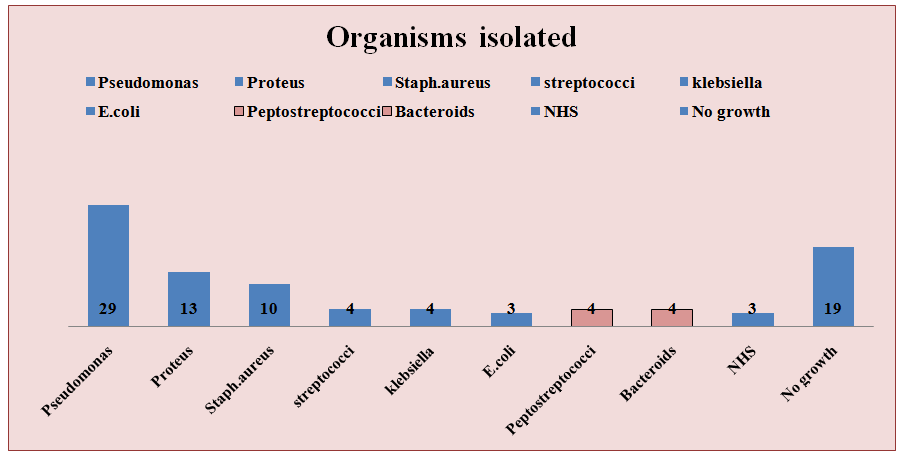
Other Gram positive organisms isolated were Streptococci (4.9%) excluding the Non Haemolytic Streptococci (NHS) (seen in 3.7%). Gram negative isolates also included E.coli (3.7%) and Klebsiella (4.9%). The anaerobic culture yielded Peptostreptococci in 4.9% and Bacteroids in 4.9% patients (Figure 5).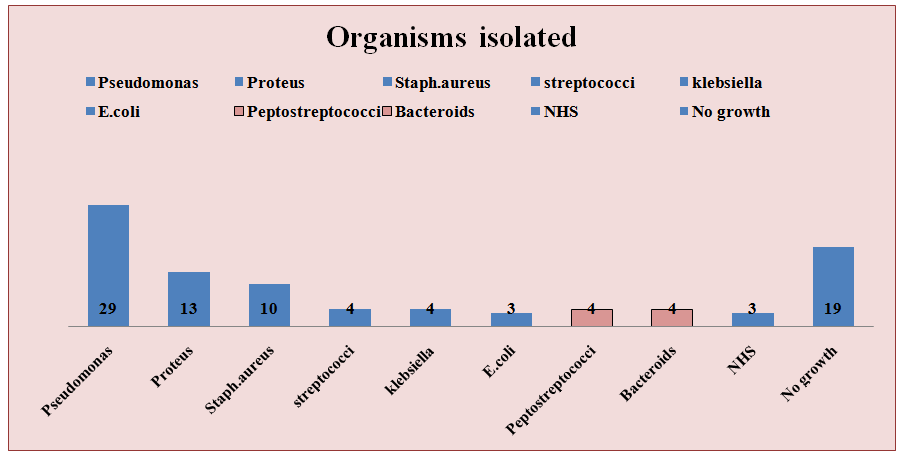 | Figure 5. Showing growth distribution of organism |
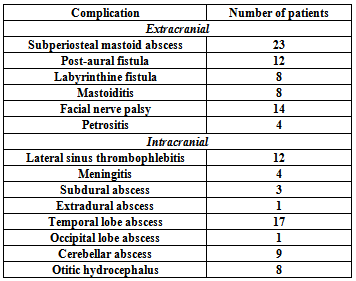
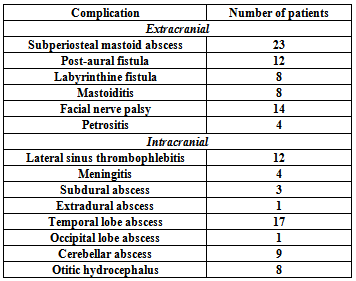
The extracranial complications observed were subperiosteal mastoid abscess, post-aural fistula, labyrinthine fistula, mastoiditis, facial nerve paralysis and petrositis. The intracranial complications included lateral sinus thrombophlebitis, temporal and occipital lobe abscess, cerebellar abscess, extradural abscess, subdural abscess, meningitis, and otitic hydrocephalus (Table 3).Table 3. Showing distribution of complications
 |
| |
|
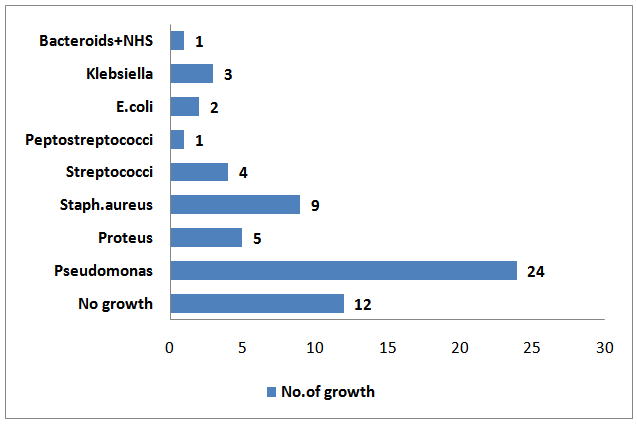
Some patients had more than one extracranial or intracranial complication while some had both extracranial and intracranial complications. In patients with bilateral discharging ear, same organism was isolated from both ears.The most common organisms isolated in patients with extracranial complications (Figure 6) were Pseudomonas (40.7%), Staphylococcus aureus (15.3%), Proteus (8.5%), Streptococci (6.9%), Klebsiella (5%), E.coli (3.4%), Peptostreptococci (1.7%) and Bacteroids with Non-hemolytic streptococci (1.7%). 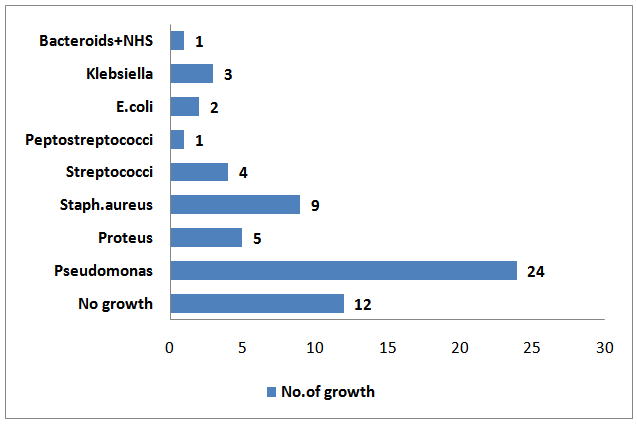 | Figure 6. Showing growth distribution in extracranial complications |
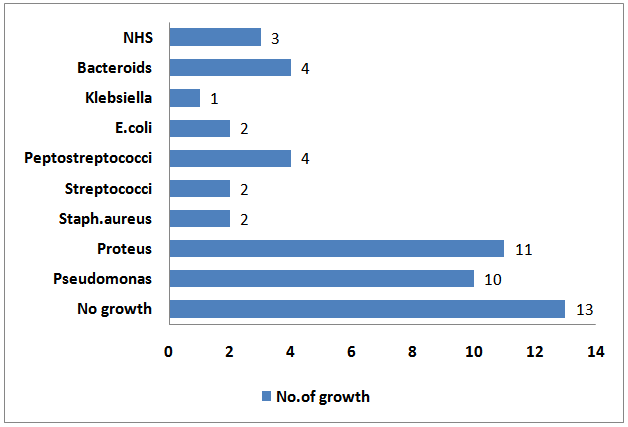
The most common organisms isolated from patients with intracranial complications (Figure 7) were Proteus (26.8%), Pseudomonas (24.4%), Peptostreptococci (9.7%), Bacteroids (9.7%), Staphylococcus aureus (4.8%), E.coli (4.8%), Streptococci (4.8%) and Klebsiella (2.4%).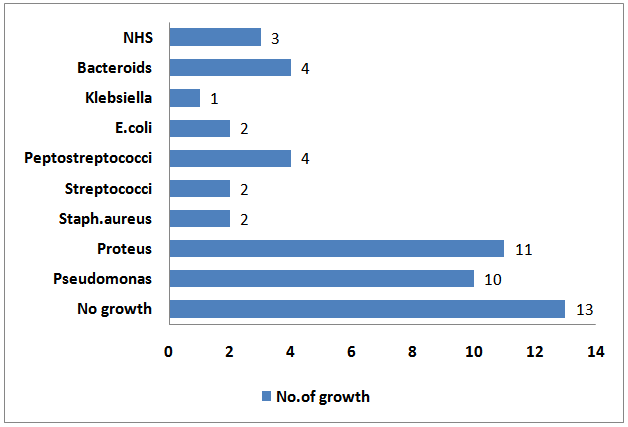 | Figure 7. Showing growth distribution in intracranial complication |
The aerobic and anaerobic bacteria isolated were all sensitive to 3rd & 4th generation cephalosporins, fluoroquinolones and aminoglycosides. Few showed resistance to penicillins and 1st generation cephalosporins.
4. Discussion
Chronic otitis media is classified as noncholesteatomatous or cholesteatomatous based on the presence or absence of cholesteatoma. Irreversible inflammatory alterations of the middle ear and the mastoid cavity are characteristic of chronic otitis media, but the mechanism of transition from acute to chronic infection has not yet been determined [12]. Patients who do not recover from acute infections show increase in mucosal oedema and effusion fluid, thus increasing the secretory capacity of mucosal glands. Due to mucosal oedema and discharge, the narrow passage of the aditus that connects the epitympanum of the middle ear and the mastoid cavity is blocked, and normal ventilation becomes impossible. At the same time, blood circulation decreases, thus inhibiting the availability of systemic and local antibiotics and anti-inflammatory agents. These alterations can induce a change in bacterial strains [13]. The frequency of mixed strains is higher in chronic than in acute otitis media, with both aerobic and anaerobic bacteria present in chronically infected individuals [7].Chronic otitis media (COM) is a major public-health problem, and India is one of the countries with high-prevalence where urgent attention is needed. It's a persistent disease with great risk of irreversible complications. COM is an important cause of preventable hearing loss particularly in the developing world and a reason of serious concern, particularly in children, because it may have long-term effects on early communication, language development, auditory processing, educational process, and physiological and cognitive development. Early, microbiological diagnosis ensures prompt and effective treatment to avoid such complications [1].COM, whether mucosal or squamous, is associated with mixed bacterial flora. In the past, cultures from CSOM grew only aerobic organisms. The isolation of anaerobic organisms from otogenic brain abscess and the fact that anaerobic organisms outnumber aerobic organisms in oral flora suggested that anaerobes are involved in middle ear infections. This idea led to the use of improved anaerobic bacteriologic techniques in the investigation of bacterial flora of COM. With these improved techniques of collection, transportation and inoculation of specimens, 20% to 50% of isolates in COM are likely to be anaerobic [5].In our study, majority (65.4%) of the patients were between 10 to 30 years of age. This was in slight contrast to other studies [3, 4, 14] in literature in which majority were below 20 years. This difference may be due to the latent time required for the onset of complications.Males comprised 79% of our study group. This may be because CSOM as such is more common in male population because of their exposed way of life [14]. Thus complications are also more likely to be seen in males.Of the 81 patients studied, 42 belonged to the lower class while 39 belonged to the middle class of socio-economic level. Traditionally CSOM has been described as the disease of the people of the poorer socio economic and disadvantaged sections, where there is overcrowding, more siblings under the age of five, malnourishment, poor sanitation and inadequate access to health care facilities; especially in children [15].In the present study, pure growth could be obtained in 61.7%, thus guiding towards appropriate management. This is comparable to the study done by V.K Poorey et al [14] but slightly less than the yield in the study by Prakash M et al [4].Among the culture isolates, 66% were Gram negative aerobes esp. Pseudomonas aeruginosa (35.8%) and Proteus mirabilis (16%). Staphylococcus aureus (12.3%) was the third most common organism isolated and comprised majority (58.8%) of the Gram positive aerobes isolated (23%) of total isolates.Anaerobic organisms were isolated in 11% and comprised of the Gram positive Peptostreptococci and Gram negative Bacteroids. These findings were comparable to the study by Ricciardiello et al in which Pseudomonas, Staphylococcus and Proteus were the most common isolates in that order [3]. In a study done by Prakash M et al Staphyloccus aureus was the most common organism followed by Pseudomonas [4].Pseudomonas aeruginosa (40.7%) was the most common organism isolated in patients with extracranial complications followed by Staphylococcus aureus (15.3%) and Proteus mirabilis (8.5%). In contrast, in patients with intracranial complications, both Proteus (26.8%) and Pseudomonas (24.4%) were almost equally isolated while Staphylococcus isolates were few (4.8%). Anaerobes were isolated in 19.5% of patients with intracranial complications but only in 3.3% of patients with extracranial complications. The present work is on bacteriology of active squamous type of otitis media with complications. There is lack of literature on the bacteriology of active squamous type of otitis media with complications and hence no data is available for comparison.The aerobic and anaerobic bacteria isolated were all sensitive to 3rd & 4th generation cephalosporins, fluoroquinolones and aminoglycosides. Few showed resistance to penicillins (MRSA was isolated in 2 patients) and 1st generation cephalosporins. Quinolones, especially ciprofloxacin was found to be effective in eradicating majority of the gram negative bacteria including Pseudomonas. Since pseudomonas is the predominant bacteria usually associated with COM therefore it can be concluded that ciprofloxacin ear drops can be tried as a first line of treatment of COM, in this part of India, though emergence of ciprofloxacin resistant pseudomonas in COM are being reported in other parts of the Asian continent [14].
5. Conclusions
• Complications of COM are most common in the 2nd & 3rd decade of life especially in male population and in the lower socioeconomic group.• Bacterial isolates can be cultured in majority of cases of COM. Same organisms are isolated from both ears in bilateral cases.• Gram negative organisms are the predominant cause of middle ear infection. Anerobes are frequently isolated in patients with intracranial complications.• Pseudomonas, Proteus and Staphylococcus are the most common organisms isolated. They were sensitive to the routine antibiotics.Knowledge about the most common organisms causing chronic otitis media with complications can help to prevent the same and the antibiotic sensitivity pattern should guide in appropriate management of COM and halt the progression of complication at an early stage. There is lack of literature on the bacteriology of active squamous type of otitis media with complications and hence no data was available for comparison. To the best of our knowledge this is the first report on bacteriology of active squamous type of otitis media with complications.
References
| [1] | Prakash R, Juyal D, Negi V,Pal S, Adekhandi S, Sharma M,Sharma N.Microbiology of Chronic Suppurative Otitis Media in a Tertiary Care Setup of Uttarakhand State, India. N Am J Med Sci. Apr 2013; 5(4): 282–287. |
| [2] | Browning GG, Merchant SN, Kelly G, Swan LR, et al. Chronic otitis media. In: George G Browning GG,Burton MJ,Clarke R et al, editors. Scott-Brown's Otorhinolaryngology, Head and Neck Surgery, 7th edition. Great Britain: Edward Arnold Publishers Ltd 200; Vol 3:3395-3445. |
| [3] | Ricciardiello F, Cavaliere M, Mesolella M, Iengo M. Notes on the microbiology of cholesteatoma: clinical findings and treatment. Acta otorhinolaryngologica italica 2009; 29:197-202. |
| [4] | Prakash M, Lakshmi K, Anuradha S, Swathi Gn. Asian J Pharm Clin Res. 2013;Vol 6, Suppl 3:210-212. |
| [5] | Olu IA, Shareef ZA, Ashraf B. Anerobes and fungi in chronic suppurative otitis media. The Annals of Otology, Rhinology & Laryngology; Aug 1997; 106(8):649-52. |
| [6] | Indudharan, R, Ashraful, J, Aiyar, Subramania. Antibiotics in chronic suppurative otitis media: A bacteriologic study. The Annals of Otology, Rhinology & Laryngology; May 1999; 108 (5):440-5. |
| [7] | Yeo SG,Park DC, Hong SM, Cha C,Kim MG. Bacteriology of chronic suppurative otitis media-a multicenter study. Acta Oto-laryngologica, 2007;127:1062-1067. |
| [8] | Albert RRA, Job, Anand J, George K, Richard J et al. Outcome of bacterial culture from mastoid granulations: is it relevant in chronic ear disease?. The Journal of Laryngology and Otology; Oct 2005; 119 (10): 774-8. |
| [9] | Ayson PN, Lopez JEG, Llanes EG. Chronic Suppurative Otitis Media: Bacteriology and drug sensitivity patterns at the Quirino Memorial Medical Centre (2004-2005): A Preliminary Study. Philippine Journal of otolaryngology-head and neck Surgery 2006; Volume 21(1-2): 20-23. |
| [10] | Maji PK, Chatterjee TK, Chatterjee S, Chakrabarty J, Mukhopadhyay BB. The investigation of bacteriology of chronic suppurative otitis media in patients attending a tertiary care hospital with special emphasis on seasonal variation. Indian J.Otolaryngol. Head Neck Surg. 2007; 59(2):128-31. |
| [11] | Shazia PS, Janardhan RR. Aerobic bacteriology of Chronic Suppurative Otitis Media (CSOM) in a teaching hospital. J. Microbiol. Biotech. Res. 2012; 2 (4):586-589. |
| [12] | DaCosta SS, Paparella MM, Schachern PA, Yoon TH, Kimberley BP. Temporal bone histopathology in chronically infected ears with intact and perforated tympanic membranes. Laryngoscope 1992; 102:1229-36. |
| [13] | Harker LA, Shelton C. Complication of temporal bone infections. In: Cummings CW, Flint PW, Harker LA, Haughey BH, Richardson MA, Robbins KT, et al, editors. Otolaryngology-Head and Neck Surgery, 4th edn. Philadelphia: Elsevier Mosby; 2005. p. 3015-6. |
| [14] | Poorey VK, lyer A. Study of bacterial flora in CSOM and its clinical significance. Indian Journal of Otolaryngology and Head and Neck Surgery.2002 Apr; 54 (2):91-5. |
| [15] | Tanmoy D, Debabrata R. A study of the bacteriological profile of chronic suppurative otitis media in Agartala. Indian J Otolaryngol Head Neck Surg 2012; Vol 64(4):326-329. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML