-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2025; 15(2): 17-31
doi:10.5923/j.nursing.20251502.01
Received: Dec. 22, 2024; Accepted: Jan. 16, 2025; Published: Nov. 5, 2025

Investigation of the Attitude of the Nursing Staff Towards Telemedicine and Health IT Applications
Stavros Kormas 1, Panagiotis Andriopoulos 2
1RN, MSc, PhD(c) General Hospital of Kalamata
2Associate Professor, Department of Nursing, University of Peloponnese
Correspondence to: Stavros Kormas , RN, MSc, PhD(c) General Hospital of Kalamata.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction: Society has gone through a rapid development due to the progress of Information Technology. The efficacy of Technology and Information applications affects the development of the economy and industry. The consequence of all above is the emergence of effects in the Health sector and of course consequently also in Health Professionals. Health services rely no longer on information systems programs, which bring only benefit. Purpose: The promotion of the applications of Health Information Technology and Telemedicine in the work of Nurses. Methodology: A search for scientific articles, published in the English language on the topic of the use of digital health systems and applications during the last six years, was carried out in the electronic databases Pubmed and Springerlink. Results: According to the findings searched n=81 studies. The majority of e-Health applications work in devices with a daily use such as Smartphone and portable tablets. Remote nursing monitoring can bring a sense of stability in patients and satisfaction of Health Professionals regarding the provision of care. A remote nursing care program, to be accepted by nursing staff and patients, should be characterized by affordability and high protection of personal data. Conclusions: Hospital centers, in the past created barriers hindering the introduction of telehealth services, while in recent years they have sought to implement strategies for their adoption. The implementation of telenursing programs will reduce costs in health systems. Health units tend to implement telemedicine programs locally by using their own resources.
Keywords: Nursing staff, Telemedicine, Health informatics
Cite this paper: Stavros Kormas , Panagiotis Andriopoulos , Investigation of the Attitude of the Nursing Staff Towards Telemedicine and Health IT Applications, International Journal of Nursing Science, Vol. 15 No. 2, 2025, pp. 17-31. doi: 10.5923/j.nursing.20251502.01.
Article Outline
1. Key Points
- • Health IT applications can improve the daily work of healthcare personnel and, thereby, contribute to the well-being of individual patients.• Restrictions and difficulties arise for Health Professionals when using applications.• Guidelines - actions with which the Health Professional can improve the performance of tasks in the future, by using specific applications.
2. Preamble
- The evolution of Informatics and Technology over the last 20 years has contributed to the progress of several scientific disciplines. The Medicine and the Nursing have always been intertwined with the evolution of technology. Thus, the field of Health Informatics and the origination of Telemedicine were unevitable components. People now have the ability to record important information about their health, without having to come into direct contact with their personal physician, as well as without having to visit a central hospital or any health center. The etymology of “Telemedicine” derives from the combination of the words: "Tele" and "Medicine”. Studying the theoretical background of Telemedicine, someone will find that several definitions have been given, which attempt to answer the question: "What is Telemedicine and how is it defined?". According to the research study carried out by Sood, et al., which approaches the analysis of definitions of Telemedicine, 104 different definitions are documented (1). The World Health Organization (WHO) refers that: "Telemedicine is the remote provision of healthcare services by all Health Professionals who use information and communication technologies for the purpose of exchanging valid information regarding the prevention, diagnosis, and treatment of diseases and injuries, with a view to upgrade the health of individuals and their communities" (2). The primary issue for a Hospital Information System is the evolution of the treatment and care of patient-citizens, in combination with the modernization of functioning of the Hospital Administration. The Information System of a modern hospital unit structurally consists of the following elements:• Human Resources-Executives: (Physicians - Nurses - Other Paramedical and Radiological personnel - Administrative personnel- Technical service, etc.).• Hardware: Information and Technology equipment.• Software: It concerns all the programs and applications on the basis of which Computers and Information Technology Units operate.• Database: It includes all the necessary data and information that determine the development and performance of a hospital at operational and management level (3).
3. Purpose of This Work
- The ultimate purpose is to promote scientific studies concerning the emergence of telemedicine applications, the evolution of health information systems and remote medical and nursing treatment. In addition, the position of the Health Professional is approached and more specifically the role of Nurses in modern innovations in Health Informatics within the work environment.
4. Methodology
- A search was conducted in the PubMed and Springerlink databases in English language by using logical operators such as OR and AND, in combination with the entry of conceptual filters such as: "Telemedicine", "e-Health", "Mobile Health", "Health Professionals", "Professionals Nurses". The period for data collection was set from 2018 to 2024, as the transition of wireless systems from the 4th to the 5th generation (4G to 5G) took place in 2018, while according to data from the European Commission for the exchange of electronic health records, over 90% of prescriptions were issued electronically, resulting in an increase in the exchange of electronic records between countries (European Commission, 2022). Regarding the exclusion criteria, studies that are in an early stage without documentation and not completed, book publications, review presentations, as well as studies published in a language other than the English were not included.
5. Outcomes
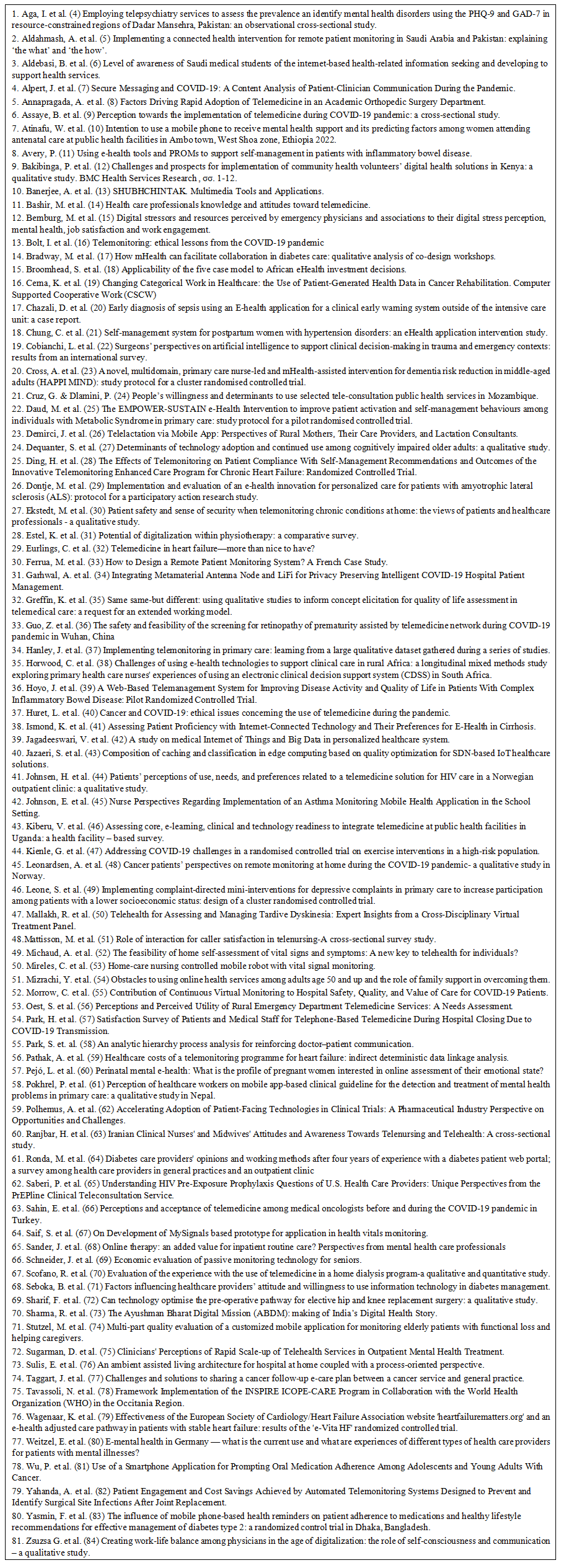
- During the first step of the search, the input filters that were entered were the words-phrases "Telemedicine", "e-Health", "Mobile Health", "Health Professionals", "Professionals Nurses", resulted in the following outcomes, issued by the electronic databases:PubMed → n=273 Entries. During the search process and in combination with the application of additional filters in 5 stages of the searches, the repository database produced n=41 records out of the total of n=273 records.Springerlink → n=532 Entries. In the implementation of the same research strategy after 2 stages of search, from n=532 records, n=240 records were produced. A thorough analysis of titles, abstracts and conclusions followed, reaching n=81 of the total records to be studied.
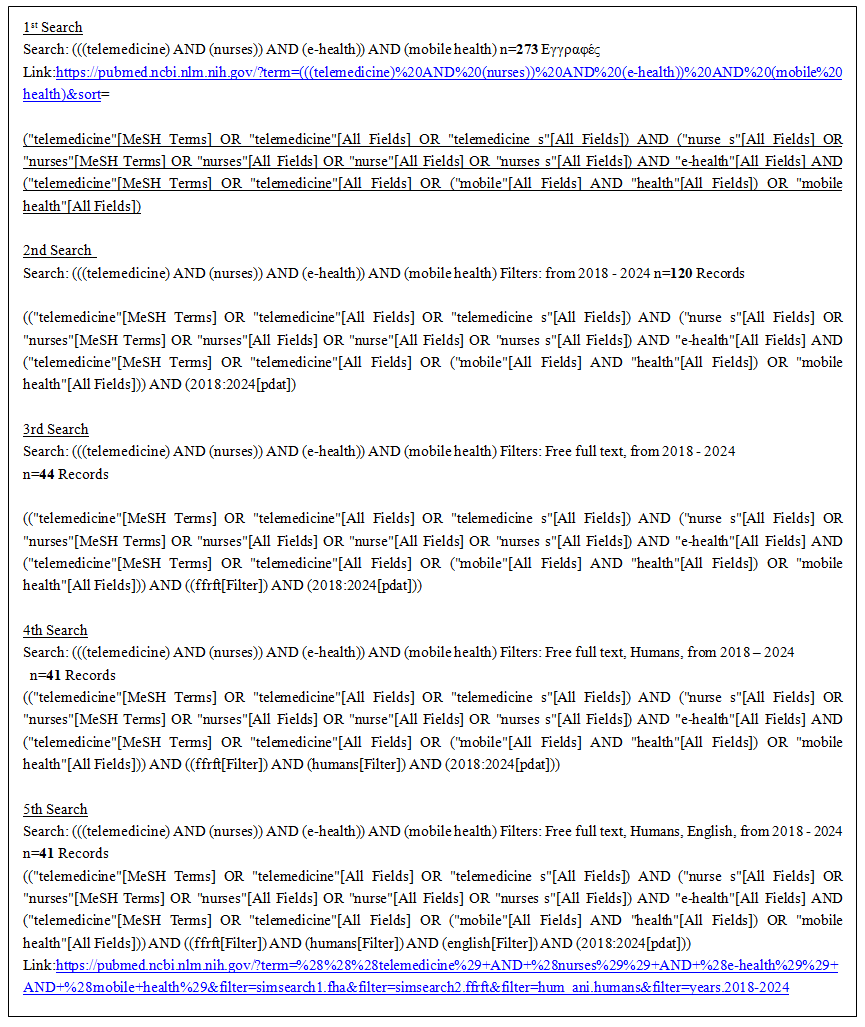 | Figure 1. PubMed Digital Health |
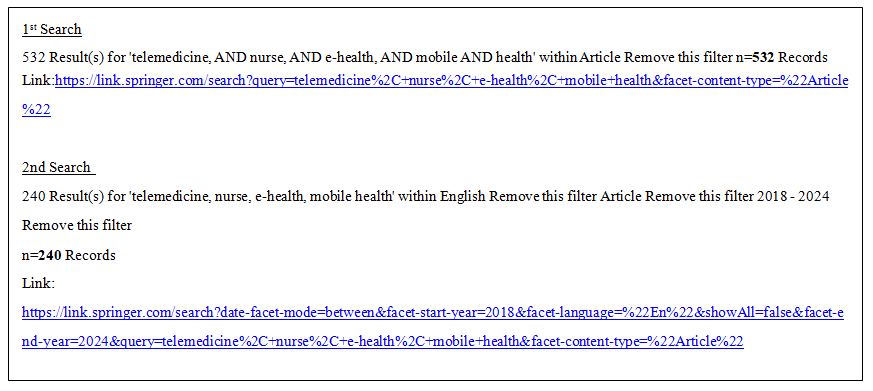 | Figure 2. Springerlink Digital Search |
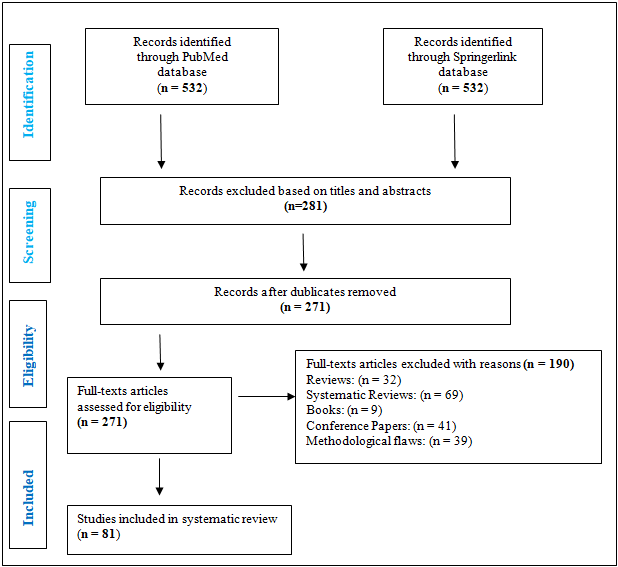 | Figure 3. The development of evolution scale |
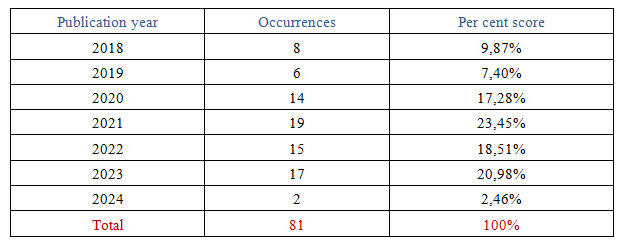 | Figure 4. Articles by author year |
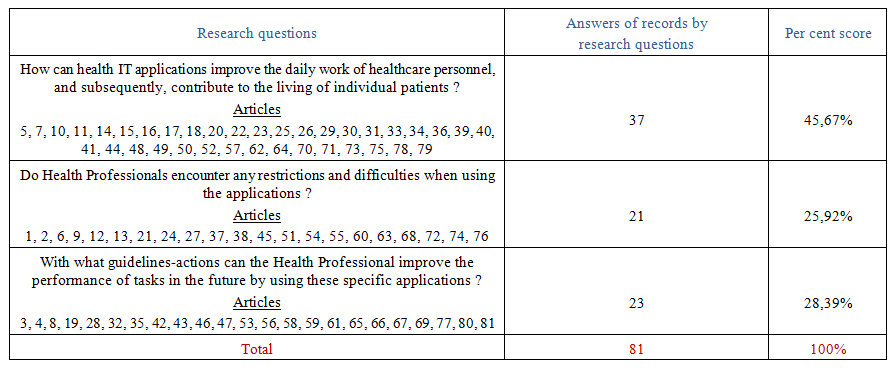 | Figure 5. Articles by Research questions |
 | Figure 6. Titles of articles |
6. Conclusions
- A remote nursing care program, in order to be accepted by medical and nursing staff as well as by citizen-patients, should be characterized by affordability and high protection of personal data. In practical terms, a positive portrayal of e-health applications was documented. Regarding the manner in which the methodological analysis was conducted, the research questions-hypotheses that were raised, were approached satisfactorily, as Health Informatics decisively influences the work of healthcare personnel on a daily basis. A large number of services related to the longed-for creation of the individual Electronic Health Record, the hemodynamic recording of the patient's data on a 24-hour basis, the scheduling of receipt and administration of pharmaceuticals, the recording of individual's mobility inside and outside the home, combined with remote medical and nursing communication, create a sense of stability in patients, as well as a satisfaction in Health Professionals regarding the provision of care. It is also worth noting that according to the information from the studies to be investigated, the incoming of the COVID-19 pandemic further developed with Telenursing the bipolar Patient-Healthcare Professional relationship. Health Informatics can be characterized not only as an interesting scientific field, but also as perennially relevant and rapidly evolving, aiming to strengthen the health sector. Patients and Healthcare Professionals expressed positive opinions regarding this specific subject of investigation. Following the conclusions, analyzed the selected articles in terms of the three research questions.Regarding the implementation of digital health, Annapragada A. et al. [8] applied an e-health solution among n=33 employees of an orthopedic surgery clinic. Following its use, more than 20% of participants reported an increased usage trend, particularly in the period after the COVID-19 pandemic. Atinafu W. et al. [10] used a structured questionnaire on n=699 women in the prenatal stage to assess the potential onset of mental health issues. According to the results, 77.3% of the sample, approximately n=530 women, expressed a willingness to use a mobile phone to receive mental health support. Banerjee A. et al. [13] focus on the SHUBHCHINTAK application, which is designed for data collection, obstacle recording, and feedback creation, with the active participation of patients and healthcare professionals. After real-time data collection and analysis, the researchers report that it is more efficient compared to existing state-of-the-art solutions. Bashir M. et al. [14] observe that the impact of telemedicine applications on individuals' daily lives and the execution of healthcare professionals' duties is such that the majority of n=370 employees, at a rate of 63.7%, possess limited knowledge, particularly the nursing staff compared to the medical staff. Bradway M. et al. [17] studied a shared PGD system that remotely schedules the individual care of patients with Diabetes Mellitus. A group of n=15 individuals with Type 1 or Type 2 Diabetes provided feedback on their experiences and needs regarding the above application, emphasizing the need for the adoption of this specific technology. Broomhead S. et al. [18] developed an investment framework for e-health based on five perspectives and also serving as a decision-making tool. It was found that countries with high per capita GDP and healthcare expenditure maintain advanced e-health. Cerna K. et al. [19] with the support of the App-PHGD application, processed the categorization of medical data from patients in the pelvic cancer recovery stage, hoping for a more active patient-nurse role. They believe that the nursing staff, in collaboration with patients, can gain joint electronic access rights to the data. Ghazali D. et al. [20] describe the Sensium E-health application in cases outside of the Intensive Care Unit, notifying the staff of any changes in the patient's vital signs. Nurses and doctors received notifications about these abnormal changes via email and also through a mobile app (iPhone or iPad). Chung C. et al. [21] also focused on the field of obstetrics, conducting a trial using smartphone devices with n=39 women with postpartum hypertension. Although only a few telemedicine programs have been implemented for the postpartum period, the majority, 94.9%, express a positive opinion. Cross A. et al. [23] investigated the potential onset of dementia in individuals aged 45–65, promoting the HAPPI MIND application, which will support multi-domain interventions, guided by nurses. The participants received brief interventions related to cognitive function, quality of life, and individual risk factors for dementia. Daud M. et al. [25] focused on the EMPOWER-SUSTAIN Self-Management e-Health application, which serves patients' personal care. By recording the opinions of n=232 patients, it was found to be somewhat complex; however, it is considered to have the potential to deliver significant benefits to their self-care. Dermirci J. et al. [26] developed a mobile Telemedicine application known as DTC, in a sample of n=17 mothers, who were quite satisfied as they addressed issues related to distance and breastfeeding support. Ding H. et al. [28] referred to the ITEC-CHF application, which helps patients manage their body weight by improving their personal care, medication adherence, and dietary organization. Dontje M. et al. [29] highlight the ALS Home-monitoring and Coaching program, in collaboration with n=71 patients and n=76 healthcare professionals, aiming to optimize the quality of life for patients with motor neuron disease. As a result, this application became more comprehensible during rehabilitation periods. Eurlings C. et al. [32] discuss the CardioMEMS application, suitable for the management of heart failure, following the implantation of a device in the pulmonary artery via the right ventricle. The aim is to improve care and reduce costs, although the achievement of both goals is not guaranteed. Ferrua M. et al. [33] aiming to support the remote monitoring of cancer patients, designed the CAPRI RPMS program, which promotes interoperable collaboration among healthcare professionals who received messages from patients and, after processing, provided the appropriate advice. Garhwal A. et al. [34] highlight the function of the Metamaterial antenna hub and wireless light (LiFi) for smart management and privacy protection in hospitals for COVID-19 patients. These systems can transmit data to specific endpoint nodes; however, achieving this in healthcare facilities requires the installation of a specific type of antenna. Guo Z. et al. [36] studied the progression of pre-symptomatic screening for early retinopathy through a telemedicine network during the COVID-19 pandemic, involving n=267 infants through online appointments. The online appointments reduced the number of direct interactions between patients and doctors compared to regular appointments, with a percentage of 58.1% versus 22.1%. Hanley J. et al. [37] describe the Telescot program, which includes a series of telemonitoring trials and studies for long-term conditions in primary health care. A total of n=181 patients and n=109 healthcare professionals participated, recording regular measurements of hemodynamic parameters. As a result, this remote monitoring program was well-received by patients. Hoyo J. et al. [39] evaluated the TECCU-NOMHADCHRONIC program, which aims to improve the quality of life in patients with complex inflammatory bowel disease. A total of n=63 patients received messages and educational advice from nurse coordinators. Almost 90.5% (19/21) of the patients adhered to the intervention, considering it a reliable strategy for improving health outcomes. Jagadeeswari V. et al. [42] explored the contribution of recent technologies to healthcare systems, such as cloud computing and fog computing, suitable for IoT devices and data storage, noting that wireless communication technologies have rapidly evolved and are now widely available to handle the complexities of remote healthcare. Jazaeri S. et al. [43] propose a method for collecting and processing medical information by pairing patients together with IoT health devices combined with SDN technology, offering significant opportunities for network optimization and medical data management. The proposed method increases storage capacity while simultaneously reduces data retrieval latency. Johnsen H. et al. [44] recorded the opinions of n=12 HIV-positive patients regarding the telemedicine services for managing their daily health issues, participating in video conferences through the national health network platform helsenorge.no. Some participants had difficulty accessing the platform. Additionally, healthcare professionals must ensure that individual preferences and needs are taken into account to make remote medical care more personalized and focused on the patient. Kienle G. et al. [47] through the ENTAIER program, studied the mobility of n=550 elderly individuals. A team of physiotherapists observed the movements of the participants to analyze challenges and potential obstacles that need to be addressed. The recording of mobility, particularly during the lockdown period, was deemed crucial. However, they noted certain challenges related to technology, not only from the perspective of the elderly but also from that of healthcare professionals. Mattison M. et al. [51] observe that the ability of patients who use telenursing services improves their emotional well-being. Out of the n=466 individuals who sought similar medical advisory services, 23.4% visited emergency departments, while 25.5% switched their primary health care physician. Michaud A. et al. [52] initiated the HYTECC study, involving n=47 individuals with a positive SARS-CoV-2 PCR test, who systematically measured their hemodynamic records. As a result, several innovative applications emerged during the pandemic crisis. Mireles C. et al. [53] describe a mobile robotic nursing device designed to monitor vital signs in patients receiving home care and discovered that robotic nursing assistance offers a well-structured system that allows patients to move freely while meeting all required tasks within the home environment. Morrow C. et al. [55] explored the contribution of virtual monitoring for patients affected by COVID-19, focusing on safety, quality, and care. As a result, 5,042 interpersonal interactions were avoided, with an average of 153 calls per day. Pejo L. et al. [60] highlight the importance of electronic mental health during the perinatal period. After analyzing the opinions of n=281 women, 31.3% of the sample had received remote psychological therapy, expressing positive views towards future use. Saberi P. et al. [65] provided inquiries through the telemedicine service PrEPline to n=1,754 HIV-positive individuals regarding HIV prevention. The questions submitted concerned specific prevention strategies, laboratory test results, as well as medication programs. The participants emphasized the importance of accessibility to teleconsultation services and programs. Saif S. et al. [67] examine the development of the MySignals prototype program for monitoring vital signs in a small sample of just n=5 participants, recording approximately n=5000 hemodynamic measurements. The training for proper sensor placement was deemed essential to ensure the safe management of health data. Sharma R. et al. [73] explore the Ayushman Bharat digital platform, designed for the protection of individual healthcare data. They observed that the platform's architecture facilitates interoperable collaboration between the National Health System and the private sector. Stutzel M. et al. [74] describe the development of the Mobile System for Elderly Monitoring (SMAI), involving n=47 older adults facing neurocognitive disorders associated with dementia. The system demonstrated a satisfactory level of usability, although some technical issues with the interfaces emerged, that could be swiftly modified to better motivate users to engage in activities. Sulis E. et al. [76] highlight a healthcare and living program known as Ambient Assisted Living (AAL) for managing home-based hospital care services. This particular program enhances care processes, providing patients with greater autonomy during recovery while simultaneously reduces healthcare and social costs. Tavassoli N. et al. [78] showcase the INSPIRE ICOPE - CARE robotic monitoring program, initiated by the World Health Organization (WHO), aiming to provide appropriate living conditions for elderly individuals. Approximately n=200,000 older adults aged 60 and above were monitored. Using a specific algorithm, healthcare professionals were able to intervene quickly in cases of emergency alerts. Although the program offered excellent support, the role of nurses in coordinating the telemedicine process needs to be redefined. Wu P. et al. [81] in collaboration with the National Cancer Institute of Salt Lake City, USA, promoted the use of a smartphone application aimed at ensuring adherence to oral medication intake in n=23 adolescents and young adults (15-29 years old) with cancer. It was found that the application was easy to set up and use for prompting medication intake. Yahanda A. et al. [82] designed two telemedicine monitoring interventions, EpxDecolonization and EpxWound, with the participation of n=1,392 and n=1,753 patients respectively, aiming at perioperative care and joint rehabilitation after surgery. These interventions provided high patient satisfaction during their use.Regarding future prospects for improving patients' daily self-care in connection with the evolution of healthcare professionals, Aga I. et al. [4] distributed standardized research tools (PHQ-9 and GAD-7) to n=2660 patients in order to document mental health disorders in regions where the field of e-health is underdeveloped. The majority of the sample was negatively affected, exhibiting strong signs of depression and anxiety, which were identified through telepsychiatry sessions. Nevertheless, digital health can assist healthcare professionals in developing effective, future-oriented initiatives related to mental health. Aldahmash A. et al. [5] focused on the implementation of the RAHAH telemedicine platform, designed for the treatment and education of patients requiring long-term medical care. The study involved n=22 patients participating in telemedicine monitoring sessions. RAHAH proves to be a significant intervention in the healthcare sector, demonstrating the potential to advance telemedicine, particularly in low-income countries. Assaye B. et al. [9] investigate the perceptions of n=737 healthcare professionals regarding telemedicine applications during the COVID-19 pandemic, as well as the benefits of e-health in the post-pandemic period. A total of 60.9% of professionals had a positive perception of the implementation of telemedicine. Furthermore, a hospital supported by specialized health IT personnel is more likely to adopt e-health applications. Bakibinga P. et al. [12] explored the prospects of digital health solutions in economically disadvantaged regions. This initiative included trials of a mobile health decision-support application, with voluntary participation from n=35 individuals. The participants identified specific issues related to the future adoption of digital technology in their region, primarily focusing on the sociopolitical environment, attitudes and behaviors, healthcare system challenges, and inadequate infrastructure. Bernburg M. et al. [15] aim to identify digital stressors experienced by healthcare professionals while also documenting potential preventive measures to better address these issues. The study involved n=204 healthcare workers who participated via an online questionnaire. Among the sample, 85% reported using digital health technologies. Notably, 55.2% stated that they had never experienced a stressful situation related to these technologies, and data security concerns did not appear to be perceived as a significant issue. Bolt I. et al. [16] explored the role of telemedicine during the COVID-19 pandemic, focusing on the ethical dilemmas faced by n=5 patients and n=9 healthcare professionals in their respective contexts. From the patients' perspective, barriers related to accessibility, quality of care, and autonomy were identified. On the other hand, healthcare professionals acknowledged the benefits of telemonitoring but expressed concerns about its applicability to a wide range of medical conditions. Cruz G. & Dlamini P. [24] examined the willingness of n=403 individuals to use public telemedicine services and identified key factors related to their willingness for frequent use of e-health programs. The majority of participants (69%) report that they would be very willing to use the proposed public telemedicine health services, but only when experiencing mild health issues. Dequanter S. et al. [27] focused on the factors influencing the adoption and use of technology by n=16 elderly individuals with cognitive-mental impairments, as well as the ways in which the adjustment gap in the evolution of digital health can be bridged. The adequate adoption of technology must now be primarily based on the needs of individuals, especially for specific groups of people with cognitive disorders. The support from the social environment will serve as a catalyst for the continuous use of technology among these elderly individuals. Ekstedt M. et al. [30] analyzed the views exchanged between n=23 patients with chronic conditions and n=9 healthcare professionals regarding data protection during the telemedicine monitoring process at home. According to these views, the future course of security and the protection of medical information exchange should be based on mutual understanding and responsibility among all parties involved. Huret L. et al. [40] investigated the ethical issues that arose from the use of telemedicine during the pandemic and how healthcare professionals' work might be affected in the post-COVID-19 era. The study drew data from interviews with n=8 oncology department workers. The interviews revealed significant variability among physicians regarding their views on telemedicine before and after the pandemic. Ismond K. et al. [41] evaluate the awareness of n=117 patients with liver cirrhosis regarding e-health, frequency of internet access, emerging digital technology, and online programs through teleconferencing. Most participants stated that they could participate in teleconferencing with appropriate training and expressed interest in an online personalized health management program. Leonardsen A. et al. [48] conducted a study aimed at capturing the views of n=11 cancer patients regarding remote home monitoring during the COVID-19 pandemic and how it might influence expectations for healthcare services for cancer patients. Patients report that remote monitoring would not fully replace in-person consultations. However, they highlight certain advantages, such as time savings and reduced physical strain. Mizrachi Y. et al. [54] documented the potential difficulties that may arise for n=31 individuals aged 50 and over when using online health services, as well as the support provided by the family environment and its potential supportive role. Participants can express new innovations that could facilitate the broader adoption of online health services, while the family environment can offer technical assistance, motivation, and encouragement for the future. Park H. et al. [57] examine the satisfaction of patients and healthcare workers regarding the impact of telemedicine during the COVID-19 pandemic by sending questionnaires to n=6,840 patients and n=320 healthcare professionals. Although a lower response rate was recorded, patient satisfaction with telemedicine was higher compared to the satisfaction of healthcare staff. Park S. et al. [58] focused on identifying barriers in online doctor-patient communication and highlighting potential future challenges, involving n=21 participants. Healthcare professionals emphasized that professionalism and reliability were more important than impartiality and mutual understanding in their communication with patients. In contrast, patients considered mutual understanding and fairness more significant than professionalism and reliability. Ranjbar H. et al. [63] conducted a study involving n=523 healthcare professionals. The research focused on their daily internet usage and overall attitudes toward tele-nursing. 36.9% of the sample agreed or strongly agreed that, over the years, tele-nursing could improve the effectiveness of the nursing staff. Sahin E. et al. [66] explore the perceptions and acceptance of telemedicine among n=110 Oncology Physicians before, during, and after the peak of the COVID-19 pandemic. A total of 31.3% believe that the frequency of patient monitoring increased during the pandemic and expecte it to rise further in the post-pandemic period. Seboka B. et al. [71] investigated the attitudes of n=406 healthcare professionals towards the use of information technologies for managing patients with diabetes. 64% of the respondents had a positive attitude towards remote monitoring, expressing their willingness to use specific methods in the future. Sugarman D. et al. [75] recorded the views of n=107 healthcare professionals working in the mental health sector regarding the development of telemedicine services in mental health, conducting video conferences with psychiatric patients. The majority, 67–88%, agreed that telemedicine could foster close relationships with patients in the future. Taggart J. et al. [77] analyze the impact of e-health on cancer patients, involving nurse coordinators, with the aim of promoting the exchange of medical information through programs such as HealtheNet and My Health Record. Researchers identify gaps in the operation of interactive e-care designs. Challenges occur at both practical and economic levels regarding the future implementation of similar programs. Wagenaar K. et al. [79] evaluated the work of the European Society of Cardiology/Heart Failure Association (heartfailurematters.org) for the future trends of personalized care, through the support of the "e-Vita HF" e-health platform. Of the n=450 patients who participated, 73.5% expressed a satisfactory opinion. However, patients with heart failure feel that they experienced short-term improvement, rather than long-term benefits.Regarding the hesitations and barriers that may arise for healthcare professionals and patients in using telemedicine applications, Aldebasi B et al. [6] focused on capturing the opinions of n=440 medical students regarding awareness of health information through the internet, problem-solving, and task support. Overall knowledge about e-health was found to be unsatisfactory, with an average percentage score of 71.6%, while 43.6% of students reported a satisfactory level. The acceptance of e-health was also deemed unsatisfactory, at 70.7%, as was the acceptance of usage methods, at 65.7%. Alpert J et al. [7] examined the potential barriers to the exchange of medical data among healthcare professionals by analyzing over n=4,200 secure messages derived from n=1,454 discussions between patients and clinical physicians. The study found that while message exchange can convey information from reliable sources, its effective implementation is more feasible for certain patient populations. Avery P et al. [11] focused on the self-management of n=15 patients with inflammatory bowel disease. The study examined the challenges potentially associated with using e-health programs. Participants, through a digital questionnaire, expressed the view that data management could be performed remotely, thereby reducing the need for in-person visits and waiting times at outpatient clinics. Cobianchi L et al. [22] explored the implementation of Artificial Intelligence in the field of surgery, assessing the opinions of n=650 surgeons regarding their knowledge and perceptions while managing emergency cases relying on digital health. Regarding the acceptance of Artificial Intelligence and telemedicine applications, 69% of the sample reported familiarity, while n=199 admitted a lack of awareness. The study highlights a gap in knowledge and the presence of skepticism concerning aspects related to Artificial intelligence and e-health. Estel K et al. [31] explored the attitudes of n=488 physiotherapists toward digitalization and the extent to which digital tools have been integrated into their daily work, using the Survey Monkey platform. 50.4% of participants expressed interest in digitalization and indicated they would use it if it provided solid benefits. Regarding the use of smartphone applications for professional purposes, only 27.7% (n=135) reported using them, as concerns about data security have been raised. Greffin K et al. [35] aimed to highlight the quality of life in telemedicine care within the spectrum of mental health by conducting interviews with n=63 patients suffering from chronic mental and other illnesses. The study focuses on the lack of uniformity in telemedicine applications, with particular emphasis on safety of use. Horwood C et al. [38] explored digital Clinical Decision Support Systems (CDSS) through online interviews with n=24 healthcare professionals who had recently completed training in the eIMCI program. Most nurses reported having minimal computer experience and skills prior to participating in the program. Johnson E et al. [45] analyze the perspectives of n=53 school nurses regarding the use of a telemedicine platform for groups of students with specific conditions. Among the findings, 46% of the school nurses reported that families faced limited access to home Wi-Fi. Kiberu V et al. [46] focused on the evaluation of digital training at both clinical and technological level for the integration of telemedicine, using a sample of n=406 healthcare professionals. Over 40% of the workers in health centers were not familiar with telemedicine. Leone S et al. [49] documented the challenges faced by n=228 patients dealing with depression while receiving online interventions. The study emphasized the importance of enhancing the knowledge of nursing staff regarding the implementation of e-health programs for the prevention and management of depression in primary health care settings. Mallakh R et al. [50] evaluated the management of future challenges in telemedicine through the participation of n=12 healthcare professionals who took part in individual semi-structured interviews. Technical issues, such as poor connectivity, video quality, and camera placement, were identified as potential barriers to the effective diagnosis and management of medical data. Oest S et al. [56] examined the acceptance of telemedicine among n=90 employees working in Emergency Departments in rural areas, as well as those in university departments in similar regions. Acceptance perceptions of telemedicine varied by specialty, but there were no significant differences in acceptance based on the field of employment. However, rural hospitals demonstrate a low level of understanding regarding the potential capabilities of digital health. Pathak A et al. [59] analyzed data regarding the costs associated with implementing the OSICAT-ECO telemedicine program for patients with heart failure. The study found no significant overall cost-saving benefits from telemedicine. However, patients with severe heart failure experience a 15% cost reduction, primarily related to hospitalization and healthcare staff fees. Pokhrel P et al. [61] examined the benefits of digital health applications in addressing mental disorders, as well as the potential barriers associated with their use, by recording the opinions of n=43 primary healthcare workers. Among the respondents, 63% had experience using m-Health approaches in their clinical practice, while the majority (n=41) of healthcare workers owned a smartphone. Polhemus A et al. [62] gathered the perspectives of n=600 healthcare professionals regarding the conditions for acceptance, as well as the challenges and opportunities arising from health technologies. 89% of respondents reported prior experience using a health application. However, several potential barriers were identified, particularly related to patients' experience and adherence to these technologies. Ronda M et al. [64] investigate the views and working methods of healthcare providers for diabetes care with the participation of n=128 healthcare professionals. Participants are hesitant and do not recommend the use of telemedicine tools for all patients. Patient health records are primarily managed as a resource for doctors rather than as a tool for patients. Scofano R et al. [70] document the perspectives of n=17 patients with kidney disease regarding potential issues that could arise in their environment before, during, and after a hemodialysis session, with additional input from n=12 nurses. The most significant challenge reported by patients in using technology was the low data transmission speed, which hindered or reduced the quality of communication. Schneider J et al. [69] focused on promoting digital passive monitoring for n=1000 elderly individuals, developing a conceptual model to estimate potential cost savings. The model recorded savings of approximately $425 per person per month following the implementation of telemedicine-based passive monitoring. This translates to an annual saving of $5069 per person and over $5.1 million for a sample population of n=1000 individuals. Sander J et al. [68] investigated the attitudes of n=176 healthcare professionals working in mental health settings, regarding the barriers and facilitators of online interventions, along with the potential benefits that could arise from the online mental health platform, Moodbuster. The majority of participants (77%) described their personal experience with online therapy as poor. Only 36% would recommend online therapy to their patients receiving psychiatric or psychotherapeutic treatment, provided it is available. Sharif F et al. [72] conducted interviews with n=16 patients with orthopedic issues, focusing on the different technologies that could be used to benefit their condition during the preoperative period. Patients should have access to an interface with a virtual electronic screening form. Healthcare professionals identify issues with each type of technology, and some online interventions are considered outdated. Weitzel E et al. [80] captured the experiences of n=425 healthcare professionals working with patients with mental illnesses, who responded to a questionnaire on digital interventions in the field of mental health. More than 90% of the sample rated the digital health programming for their patients as moderate to very high. Yasmin F et al. [83] explored the potential of mobile devices to support n=273 patients with type 2 diabetes in adhering to their medication regimen and promoting a healthy lifestyle. 90% of the participants reported adherence to their medication. However, some patients indicated that they missed medications and hospital visits due to financial constraints. Zsuzsa G et al. [84] documented the work-life balance challenges faced by n=31 healthcare professionals when using telemedicine programs. The balance between physicians' private and professional lives remains a constant emerging research topic, as new factors constantly influence these parameters.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML