-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2024; 14(1): 22-32
doi:10.5923/j.nursing.20241401.02
Received: Aug. 25, 2024; Accepted: Sep. 20, 2024; Published: Oct. 26, 2024

Effect of Medication Administration Simulation on the Clinical Confidence and Competence of Nursing Students: A Systematic Review
Zhiela Marie E. Abiva, Mari Elaine P. Lorica, Sabina L. Pariñas
Department of Nursing, Mariano Marcos State University, City of Batac, Philippines
Correspondence to: Zhiela Marie E. Abiva, Department of Nursing, Mariano Marcos State University, City of Batac, Philippines.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Simulation-based learning (SBL) has effectively developed student nurses' clinical competence and confidence. However, systematic evidence on the effect of the different levels of simulation fidelity on student nurses' clinical competence and confidence still needs to be discovered. This motivated the researchers to systematically review randomized controlled trials, quasi-experimental studies, and literature reviews to examine the evidence on using low, medium, and high-fidelity simulation on the outcomes measure. CINAHL, Health Source: Nursing/Academic Edition, Biomedical Reference Collection: Basic, Medline and Google Scholar were utilized as electronic databases during the search. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Melnyk and Fineout Overholt’s (2019) rating system were used to provide a structured framework, and Joanna Briggs Institute’s Critical Appraisal Tool was used in appraising the selected articles. Fourteen studies were included and were primarily conducted in USA countries and focused on various routes of medication administration. The outcomes of the studies support the evidence that simulation is an effective strategy for improving nursing student clinical competence and confidence in safe medication administration.Standardization of simulation scenario quality, evidence-based study design, and valid and reliable outcome measurements would benefit the discipline.
Keywords: Fidelity simulation, Medication administration, Nursing students
Cite this paper: Zhiela Marie E. Abiva, Mari Elaine P. Lorica, Sabina L. Pariñas, Effect of Medication Administration Simulation on the Clinical Confidence and Competence of Nursing Students: A Systematic Review, International Journal of Nursing Science, Vol. 14 No. 1, 2024, pp. 22-32. doi: 10.5923/j.nursing.20241401.02.
Article Outline
1. Introduction
- The Joint Commission on Accreditation of Healthcare Organizations emphasizes clinical competence as the most essential criterion required from each healthcare provider [1] as it is crucial in improving the quality of service in the healthcare system [2]. Competence is vital for nurses to maintain their clinical confidence [2]; a successful execution of a skill, known as performance accomplishment, is reported to enhance confidence in the ability to perform the skill in the future [3]. Thus, clinical confidence plays a crucial role in the adequate performance of nurses in the clinical area [3]. Thus, nurses lacking confidence in their profession may compromise the delivery of safe and effective healthcare, such as administering medications. Notably, the administration stage in the medication continuum is correlated with a high incidence of medication errors [4], which leads to injury, morbidity, and mortality. Due to the significant impact on patient safety, nurses must start cultivating these competencies during their foundational training, considering that nurses hold a significant role in medication management, particularly medication administration [5].Nursing education aims to develop skilled nurses capable of delivering professional care in the dynamic and evolving field of nursing practice [6] or nurses who are both competent and confident in the clinical setting [3]. Throughout nursing education, students are anticipated to progressively enhance their knowledge, skill set, and attitude, ultimately culminating in acquiring behaviors that align with the secure and autonomous implementation of this Entrustable Professional Activity (EPA) upon graduation [7,8]. Nonetheless, an inquiry conducted among nurse leaders reveals a sense of discontentment about the medication proficiency exhibited by recently graduated nurses [9], and students themselves express a sense of inadequacy in terms of their preparedness to administer medications in a secure manner [10]. Lack of experience, anxiety, and fear have been identified as the primary factors contributing to medication errors among nursing students [5]. The scarcity of practical opportunities required to solidify psychomotor proficiencies and cognitive prerequisites essential for cultivating a sense of assurance and proficiency in the realm of secure medication administration is attributable to constrained faculty-to-student ratios and facility limitations [9,11]. These limitations impede practice opportunities throughout nursing school, which are necessary to gain medication administration proficiency [10]. These constraints hinder the availability of practice instances throughout the nursing education curriculum that are imperative for attaining a commendable level of proficiency in medication administration.The World Health Organization Patient Safety Curriculum Guide emphasizes prioritizing patient safety in nursing learners [12], and nurse educators must equip students with the requisite proficiency, encompassing medication administration [13]. The clinical practicum is important for nursing students as it allows them to apply their acquired clinical skills and integrate theoretical knowledge into practical experience [3]. Active pedagogical methodologies serve alternative co-participatory roles within instructional and learning frameworks; as such, a realistic simulation strategy reproducing clinical environments close to the real one stands out for improving knowledge, skills, and attitudes [14]. Simulation techniques in nursing programs have gained traction and achieved widespread recognition on a global scale [15,16]. It has been a long-accepted form of clinical replacement for nursing in different countries. It provides active learning through guided experiences and aims to reproduce reality in a controlled, interactive context, addressing essential aspects of actual practice in a risk-free environment. Simulation is integral to nursing education because it provides a safe, timely, and prescriptive way to meet learning objectives at the simulation, course, and academic program levels [17]. In a non-threatening environment, students optimize the impact of their learning with the ability to replicate critical and joint problems by experiencing errors and self-reflection on their actions to provide multiple treatment options to be explored without injury or discomfort to an actual patient or to manipulate time as a factor for in managing nursing care [18] and can cause increased financial costs for the healthcare system [19]. The integration of simulation in nursing education would advance skill acquisition and patient safety [20]. In order to be effective, scenario design must consider the level of fidelity in which the student is immersed. Different reviews found the use of simulation as an effective method in enhancing nursing learner’s overall learning outcomes, increasing knowledge, skill performance, and confidence [21-27], although the evidence about its effectiveness is inconsistent [28]. There is also concern that simulation and skills training facilities are insufficient and underutilized [29] or has not been implemented to its fullest extent [30-32]. An integrative review of [33] focused on the contribution of realistic high, medium, or low fidelity simulation to the promotion of the acquisition of skills on patient safety. A meta-analysis conducted by [34] focused on medication error and determined the impact of low fidelity simulation on medication knowledge and competency performance.Though there is a paucity of the benefits of simulation in several nursing education contexts, including the enhancement of skills and confidence in the medication administration process, by revisiting and investigating the effect of different levels of simulation fidelity on nursing learners' clinical competence and confidence in safe medication administration, this study contributes to the ongoing discussion on the optimal design and implementation of simulation-based training programs.
2. Methodology
2.1. Design and Study Criteria
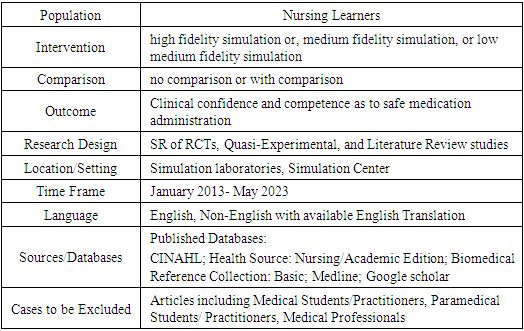
- The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) were utilized for the study. A systematic review of the literature was conducted to answer the PIO (Population, Intervention, and Outcomes) question: "What is the effect of low, medium, and high-fidelity simulation (I) in the clinical confidence and competence (O) of nursing students (P) as to safe medication administration?" The primary outcome was to explore various studies to determine the effect of the different fidelity levels of simulation on improving the safe administration practice of nursing learners. The inclusion and exclusion criteria can be gleaned in Table 1.
|
2.2. Search Strategy
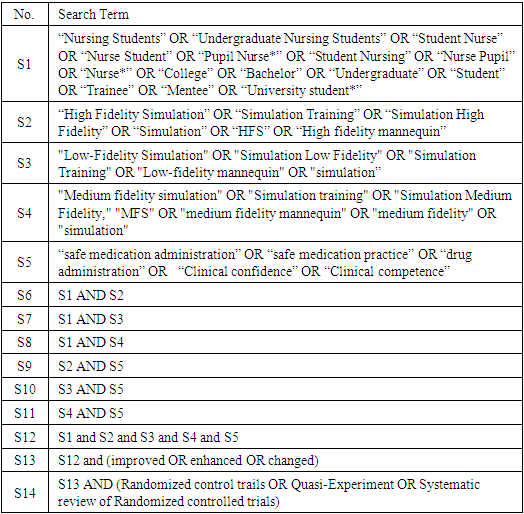
- The published databases searched for the relevant evidence published in databases such as CINAHL, Health Source: Nursing/Academic Edition, Biomedical Reference Collection: Basic, Medline, and Google Scholar to answer the foreground question," What is the Effect of low, medium, and high-fidelity simulation in the clinical confidence of nursing students as to safe medication administration". The initial keywords, as reflected in Table 2, were "nursing students," "high-fidelity simulation," "low-fidelity simulation," "medium fidelity" and “safe medication administration''. Similar words and alternative words that were also identified from the keywords were "nursing students," "undergraduate nursing students," "student nurse," "nurse student," "pupil nurse*," "student nursing," "nurse pupil", "nurse*", "college", "bachelor", "undergraduate", "student", "trainee", "mentee", "university student*" are words that will be expounded from "nursing students”. “Simulation Training”, “Simulation High Fidelity”, “Simulation”, “High Fidelity Mannequin” and “HFS” were alternative words derived from “high fidelity simulation”. Alternative words for “low fidelity simulation” were “Simulation Low Fidelity," "LFS," "Low Fidelity Mannequin," simulation," and "Simulation Training." "Simulation training," "Simulation Medium Fidelity," "MFS," "medium fidelity mannequin," "medium" are words that will be used to expound "medium fidelity simulation." "Clinical confidence," "safe medication practice," "drug administration," "clinical confidence," and "confidence" will be used to expound "safe medication administration.
|
2.3. Study Selection
- Two authors screened all titles and abstracts based on the inclusion and exclusion criteria in Table 2 right after the search on the selected databases had been done. If, by the title, it was determined that the evidence might be included, then the abstract was read. After selection, the three authors reviewed full texts to exclude articles that did not meet the eligibility criteria.The search identified a total number of 9,895 290 potentially relevant articles from databases. Two hundred fifty-one articles were recorded for the title screening. Articles were excluded due to ineligible titles. Thus, 82 articles were recorded for abstract screening. Ineligible abstracts were excluded. Thus, only 60 were recorded for full-text screening. Duplicates were removed from the combined database. Thus, 36 articles were recorded for full-text screening. Generally, 36 articles met the inclusion criteria and proceeded to full-text screening and assessment. Articles selected for full-text screening from different databases were excluded for the following reasons: four other interventions such as computer-based simulation and virtual simulation); five other outcomes, such as knowledge and confidence; two are of different types of studies, such as surveys and mixed method studies; and eleven articles did not have medication administration as the nursing skill. Overall, 14 articles were included for a systematic review of the literature, as seen in Figure 1.
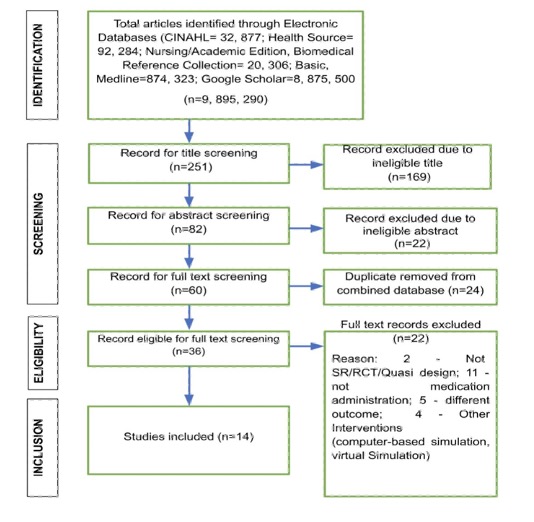 | Figure 1. PRISMA Diagram |
2.4. Data Extraction and Review of the Selected Studies
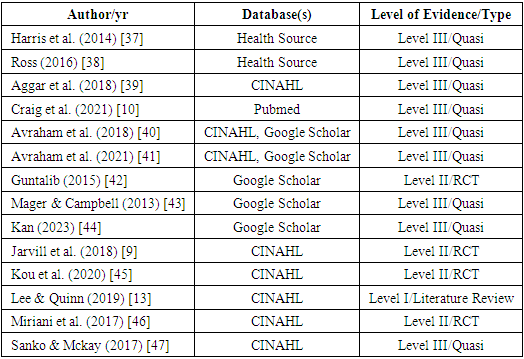
- The three researchers of the study served as the reviewers of the data obtained. The methodological quality of eligible studies was evaluated using the Johanna Briggs Institute critical assessment tool [35] for the evidence to be arduously appraised. Melnyk and Fineout Overholt’s rating system evidence hierarchy was utilized to level the evidence [36]. This hierarchy rates evidence for intervention questions as level I, being the highest level, which represents evidence obtained from SRs or meta-analyses that include randomized controlled trials down to level VII, being the lowest level. The risk of bias was evaluated based on sample size and treatment, randomization, study design, outcome measures, and the quality of the instruments and statistical analyses used for the measurement of outcome variables. A summary of the evidence and the appraisal tool used can be found in Table 3.
|
3. Results
3.1. Study Characteristics
- A total of 14 studies qualified for inclusion, with ten quasi-experimental studies, three randomized controlled trials, and one literature review. The studies were conducted in six countries: United States of America (n=8), Israel (n=2), Australia (n=1), Malaysia (n=1), Turkey (n=1), and Taiwan (n=1). Participants were undergraduate nursing students across all levels from the first year to the fourth year (n=2,860). The simulation fidelity included in this review is high and low. Three studies [38,39,41] used a low-fidelity type of simulation as their intervention. One study [9] used high-fidelity simulation in the intervention. Three studies [10,13,46] used both low and high-fidelity simulation in their intervention. The other two studies used mannequins specific to simulated mannequins [40] and manikin/ mannequin-based scenarios [47]. One study [42] used human patient simulators in the intervention. At the same time, the other three studies [37,43,45] did not specify the level of fidelity in their simulations as their interventions. No instances of medium-fidelity mannequins being utilized have been documented. Nine studies incorporated various routes of medication administration to determine the desired outcome, which consisted of inhalation, intravenous, intramuscular, subcutaneous, oral, inhalation, drops, and through a feeding tube. Three studies utilized one route of administration to determine the desired outcome. Two studies [41,44] did not specify the route of administration. Other studies also included the use pre-fill medication boxes [43] and medication dispensing cart [46] as a component of safe medication administration. The studies that were included exhibited a favorable level of methodological rigor using the Joanna Briggs Institutes (JBI) Critical Appraisal Tool in the review. The subsequent assessments conducted within these studies were comprehensive, and data collection and analysis were performed utilizing dependable and suitable methodologies. The quasi-experimental studies that were incorporated demonstrated transparent cause-and-effect sequences, featured a minimum of one comparative group, and ensured equal treatment for both the intervention and control groups. In randomized controlled trials, there were thorough follow-up assessments and comparable treatment groups at the outset, and both the intervention and control groups received identical treatment except for the specific intervention under investigation. In the literature review, the synthesis presented is appropriate for the review question.
3.2. Clinical Competence in Medication Administration
- Twelve studies evaluated the clinical competence in medication administration among nursing students using varied measurement tools such as competency-based assessment tool (CBAT), MA Preparedness Questionnaire (MAPQ), Medication Administration Evaluation Scale (MAES), Satisfaction with Simulation Experience (SSE), Safe Administration of Medication (SAM) Scale, Medication Administration Safety Assessment Tool (MASAT), Modified Gladstone Scale of Medication Errors, Task Specific Checklist, Medication Safety Knowledge Assessment (MSKA), Medication Safety Critical Element Checklist (MSCEC), Medication administration error checklist, Healthcare Professionals Patient Safety Assessment (HPPSA), Medication Administration Competence and Confidence Scale (MACCS) and Medication Administration Observation Tool (MAOT).Outcomes of the different studies consistently affirm the effectiveness of simulation as a valuable approach to enhance student learning. The incorporation of high-fidelity individual simulations has notably bolstered nursing students' competence in the safe administration of medications, while the integration of technology and online learning within simulation exercises has contributed to a demonstrable increase in medication safety competence [9,13,46]. Furthermore, the utilization of manikin-based scenarios within simulation-enhanced pharmacology has yielded positive outcomes, leading to notable enhancements in safe medication administration [47].Simulation holds promise for enhancing student performance in medication administration exams [37]. Additionally, the implementation of the SAM scale is widely regarded as an effective tool for augmenting both knowledge and performance [43]. Furthermore, various studies have demonstrated that the incorporation of diverse forms and levels of simulation can contribute to the improvement of clinical competency among nursing students.
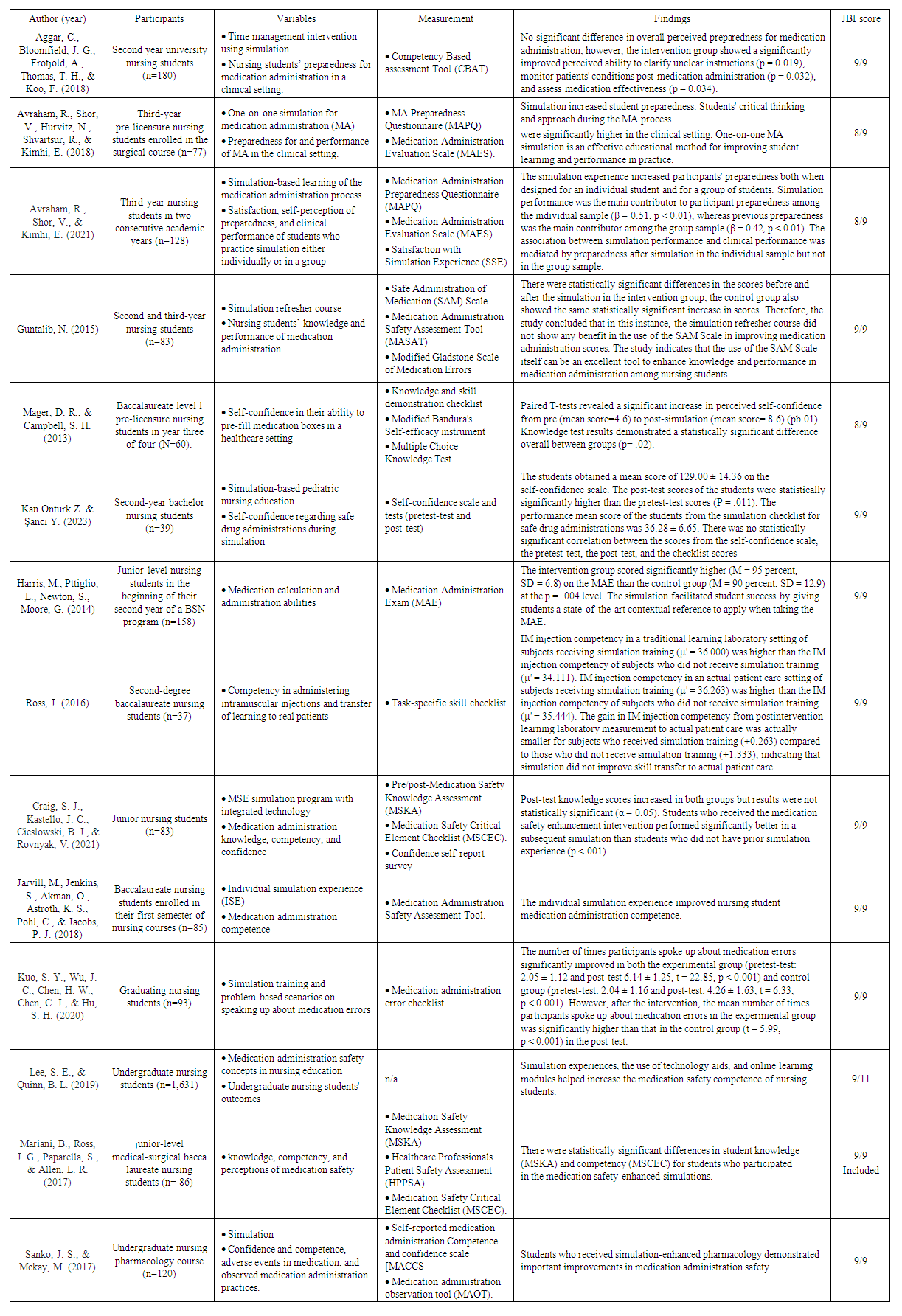 | Table 4 |
3.3. Clinical Confidence in Medication Administration
- Four studies evaluated clinical confidence, but two of them evaluated both the clinical competence and confidence of nursing students in medication administration. There are different measurement tools being utilized by the evaluated studies, such as Self-Confidence regarding safe drug administration during simulation, medication administration knowledge, competency and confidence, self-reported medication administration competence and confidence scale (MACCS), and self-confidence reporting tool C-scale.Competence and confidence scores were compared in the study of [47]. To highlight the confidence score, study results revealed that the intervention group demonstrated an improvement in confidence, and the control group data showed a decrease in confidence over time. In the study [10], the intervention group indicated greater confidence than the control group; thus, there was some evidence of a difference between the two groups (p = .082 and p = .098, respectively). The study [44] revealed that there was no statistically significant correlation between the scores from the self-confidence scale, the pretest pre-test, the post-test, and the checklist scores.
4. Discussion
- This review synthesized and summarized the findings of 14 studies that employed either a randomized controlled trial, quasi-experimental design, or literature review each including at least one comparison group. The studies have been primarily conducted in advanced countries with advanced economies, including the United States of America, Israel, Australia, Turkey, and Taiwan, as described by the World Population Review [48]. The result conforms to [49] that simulation has been commonly integrated into nursing education due to its effectiveness and sporadically in low-resource settings [50].This study aims to examine the effectiveness of the different levels of simulation fidelity on student nurses' clinical competence and confidence in medication administration. Most studies indicated that simulation positively influenced clinical competence and confidence, with observed effects being statistically significant, particularly when compared to a control group. Although one study showed no significant difference in overall perceived preparedness for medication administration, there was a significant improvement in specific medication administration skills, such as the perceived ability to clarify unclear instructions, monitor patients' conditions post-medication administration, and assess medication effectiveness [36]. Research indicates that implementing a structured simulation program on medication administration can markedly enhance students' competency in administering medication safely [10]. The review's findings align with those of [51,52], demonstrating that simulation-based learning enhances nursing students' clinical skills and self-confidence in various nursing competencies. This approach should be strongly considered for its potential to elevate nursing students' proficiency in the safe administration of medications. Incorporating simulation methodologies into the curriculum offers invaluable opportunities for nursing students to hone their skills in safe medication practices. Moreover, the diversity of simulation scenarios empowers students to cultivate a broader skill set, encompassing not only medication administration but also the ability to clarify instructions, vigilantly monitor patient conditions, and assess the effectiveness of interventions. Enhancing students' confidence has been linked to increased assurance in their ability to execute clinical tasks effectively [53].Although designs and methods varied considerably, and a wide range of instruments have been used with differing levels of validity and reliability to measure the outcomes, there are consistent results. Moreover, irrespective of the fidelity or type of simulation employed, simulation has a positive impact on clinical competence and confidence, demonstrating greater effectiveness compared to alternative methods which is consistent with systematic review conducted by others [54,55].The review's generalizability may be limited due to the specific settings, populations, or educational contexts of the included studies. To address these limitation and provide a more comprehensive understanding of simulation-based teaching's effectiveness in nursing education on medication administration, further research is necessary.Implications for education This review presents consistent evidence to recognize different fidelity of simulations combined with quality simulation scenarios, evidence-based study design, and valid and reliable outcome measurements significantly improve learning outcomes, competence, and confidence in medication administration. It is imperative as a highly impactful approach in nursing education.Implications for research Future research undertakings should focus on conducting more rigorous multisite pre-test and post-test experimental studies on various nursing competencies and learning outcomes with reliable and valid instruments, quality simulation scenarios, and evidence-based study design. Research undertakings should also include medium fidelity simulation for the evaluation of its effectiveness on clinical competence and confidence on medication administration.
5. Conclusions
- Given the study's findings, simulation-based education's effect on nursing students' clinical competence and confidence in medication administration is consistently positive. Simulation applications with progressive low, medium, and high fidelity are suggested to be incorporated into the teaching and learning method for nursing students. In addition, it is believed that deploying simulation applications that contain more extensive medication administration capabilities would assist knowledge and skill integration and improve student attitudes toward holistic patient safety. Reviewing student feedback on simulation can help uncover the positive and negative aspects of the simulation from the student's perspective and enable the technique to be refined by their views. Additionally, despite the majority of research demonstrating a significant impact of interventions on outcomes, the results from the known studies should be regarded with caution due to methodological restrictions. Standardizing simulation scenario quality, evidence-based study design, and valid and reliable outcome measurements would benefit the discipline. Exploration is needed to determine the transferability of the clinical competence and confidence gained from simulation-based education to the clinical area and actual patients.
ACKNOWLEDGEMENTS
- The researchers would like to express heartfelt gratitude to Mariano Marcos State University, especially to the office of our President, Dr. Shirley C. Agrupis, the office of the Vice President for Research, Development, and Innovation, Dr. Nathaniel R. Alibuyog. To the members of the Research Directorate, headed by Dr. Dionisio S. Bucao and the previous research director, Dr. Bjorn S. Santos, for their earnest support and guidance for this research journey. Likewise, the researchers would like also to acknowledge the support of the Nursing Department in the College of Health Sciences of the same university. And lastly, to God, our ultimate Creator and the Maker of this very promising product of endeavor.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML