-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2021; 11(2): 31-35
doi:10.5923/j.nursing.20211102.01
Received: Jun. 15, 2021; Accepted: Jul. 3, 2021; Published: Jul. 15, 2021

Financial Management and Evidence-Based Practice Culture among Nursing Managers in Ghana
Patience Boatemaa Antwi-Yamoah1, Fiskvik Boahemaa Antwi2, Simon Akwasi Osei2, Rachel Serwaah Antwi3
1Valley View University, Ghana
2Saint Louis University, Philippines
3University of the Southern Caribbean, Trinidad, and Tobago
Correspondence to: Patience Boatemaa Antwi-Yamoah, Valley View University, Ghana.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

In the healthcare sector, patients only receive approximately 50% of the treatment indicated by the evidence. Only 10%–15% of clinicians have integrated evidence-based practice (EBP), with a 10- to 20-year lag in translating research to practice. Most hospitals and practitioners do not use the existing evidence and standards for care in their practices due to cost. Nurse managers should possess effective financial management practices to adapt evidence-based practice. Therefore, this correlational study aims to identify the relationship between financial management practices and evidence-based practice culture. A significant difference in terms of financial management practices and years of experience was also considered. Sixty-four (64) nurse managers in selected hospitals in Accra, Ghana, were conveniently sampled to answer the structured questionnaire. The statistical treatment used was Pearson correlation and ANOVA. The results of the study showed that there was a high significant positive relationship between financial management practices and organizational evidence-based practice culture. In terms of years of managerial experience and financial management practices, the study yielded a significant difference. The results suggest that as the financial management practices increase among nurse managers, so does the evidence-based practice culture of the institution. Additionally, nurse managers with additional years of experience possess good financial management practices. The study recommends that nurse managers should engage in continuous professional development. Moreover, nurse managers with higher managerial experience should provide mentorship to novice nurse managers.
Keywords: Evidence-based practice, Financial management practices, EBP, Nurse managers
Cite this paper: Patience Boatemaa Antwi-Yamoah, Fiskvik Boahemaa Antwi, Simon Akwasi Osei, Rachel Serwaah Antwi, Financial Management and Evidence-Based Practice Culture among Nursing Managers in Ghana, International Journal of Nursing Science, Vol. 11 No. 2, 2021, pp. 31-35. doi: 10.5923/j.nursing.20211102.01.
1. Introduction
- In the healthcare sector, consumer pressure and rising patient expectations emphasize the importance of evidence-based practice among clinicians. According to research by Sharplin et al. (2019), patients only receive approximately 50% of the treatment indicated by the evidence. Only 10%–15% of clinicians have integrated evidence-based practice (EBP), with a 10- to 20-year lag in translating research to practice. The Institute of Medicine (IOM; 2008) set a goal of 90% clinical integration of EBP by 2020, implying that 90% of all medical interventions should be evidence-based. This goal, which is to provide the healthcare consumer with safe and high-quality results, can only be achieved through institutional reform and adopting an EBP culture. As a result, despite the growing emphasis on EBP, the majority of hospitals and practitioners do not use the existing evidence and standards for care in their practices due to cost. This emphasizes the importance of developing infrastructure that supports EBP and integrates it into practice settings (Sharplin et al., 2019).According to Warren et al. (2016), part of the challenge may be in obtaining buy-in and justifying the scarce resources needed to move the organization to the next level. Failure to embrace EBP can have serious consequences for patients, nurses, and the organization in terms of poor outcomes, which, in today's regulatory environment, might have a significant impact on the bottom line. Obtaining the resources and financing needed to set up an EBP environment, on the other hand, can be challenging. With this in mind, nurses in positions of leadership must advocate for the adoption of EBP. Furthermore, in order to do so effectively, nurse leaders should have effective financial management practices (Barría, 2014).Financial management skills are the process of implementing and administering financial control systems, collecting financial data, evaluating financial reports, and making sound financial control decisions based on the analysis (Waxman & Massarweh, 2018). The ability of nurse managers to execute financial management systems is a key factor in evidence-based sustainability. On the other hand, most nurse managers are appointed based on seniority and clinical expertise rather than the required qualifications, particularly financial management capabilities (Waxman & Massarweh, 2018).Naranjee et al. (2019) stated that most nurse managers, even after years of experience, lack confidence in their financial management skills and hence delegate all financial matters to hospital administrators and accountants. Even while nurse managers are in charge of the day-to-day operations at the unit level, where a bigger share of healthcare resources are spent, their ability to effectively oversee this critical responsibility can be the difference between a hospital's adoption of evidence-based practice. Additionally, Paarima et al. (2020) suggested that nurse managers with a thorough understanding of financial management will be able to engage employees in discussions about proficiency and cost efficiency in the unit where most healthcare services are given.Nurse managers in Ghana are responsible for supervising nurses and converting hospital plans and goals into action. Over 80% of the population's healthcare needs are met by public sector hospitals, which are funded by the government. Financial restrictions, limited budgets, bad management, insufficient resources, and decaying infrastructure, on the other hand, limit these institutions' ability to deliver efficient and evidence-based care (Heerdegen et al., 2020). As a result, nurse managers are managing nursing units with insufficient logistics, which has a negative impact on healthcare delivery. Nurse managers must have excellent financial management abilities in order to respond to these financial difficulties and provide cost-effective healthcare (Heerdegen et al., 2020).Paarima et al. (2020) conducted a study in Ghana to understand the financial management skills among 121 Ghanaian nurse managers. The study showed that nurse managers had a moderate level of knowledge and skills in financial management. Additionally, Age, gender, qualification, the experience of nurse managers significantly influenced their financial management. Hence, the authors recommended further mentorship programs and continuous education to enhance nurse managers' financial management practices.A qualitative study conducted by Naranjee et al. (2019) examined the financial management practices of nurse managers in South Africa. The study was conducted among five health districts, and 18 nurse managers were interviewed. The study showed that financial management was a primary function of nurse managers. However, they lacked the skills and competencies in financial planning, monitoring, and decision-making.In another perspective, a study conducted by Bai et al. (2017) examined the financial management practices of Chinese nurse managers and their challenges. The study showed that nurse managers are challenged by the lack of training in financial management and roles in the healthcare system. In making decisions about a patient's care, evidence-based practice is a deliberate, problem-solving approach to clinical practice that includes the best evidence, patient values and preferences, and a clinician's expertise. Clinical practice is based on sound evidence when evidence-based practice (EBP) is used, and patients benefit as a result. EBP also leads to more consistent clinical recommendations and practice throughout the healthcare system.To promote EBP adoption, time and resources must be invested in its implementation. Budgets need to address start-up and continuing costs, including employees, equipment, meetings, training to develop experts, training for doctors, and resources for assessment. It may be advantageous to capture such investments in order to establish the EBP's benefit. To keep the EBP improvement going, more training and reinfusion will be required. Personnel costs for meetings and training are frequently included in implementation costs.A study conducted by Fu et al. (2020) examined evidence-based practice competencies and culture among nurses in public hospitals. The study used a total sample of 1036 nurses in China. The study results showed that nurses' EBP competency was low and therefore affected their use of evidence-based practice were moderate. Therefore, this suggests that the EBP culture among nurses was not optimal, which poses a risk to patient care and safety.Aynalem et al., (2021) cross-sectional study investigated EBP sustainability through the level of evidence-based practice utilization among nurses. The study showed that evidence-based practice utilization among nurses was low. The authors concluded that the related factors that cause low EBP utilization among nurses included the lack of training and resources. Therefore, the authors concluded that improving organizational resources and nurses’ competencies are essential in promoting an evidence-based practice culture.To further understand the relationship between financial management practices and evidence-based practice, Kueny et al., (2015) qualitative study conducted among nurse managements investigated factors that facilitate or hinder EBP practice. The study showed that organizational culture, resources, and financing hinder or promote EBP culture.Sharplin et al. (2019) investigated the factors that facilitate or hinder the sustainability of EBP culture. The study implemented a mixed-method design among administrators in Australia. The study revealed that staff training structure and financial resources foster the sustainability of EBP culture. Li et al. (2018) conducted a systematic review by investigating the organizational features that influence EBP practice. The study results were categorized into 6 making organizational contextual features: leadership, communication, finance and resources, monitoring, and feedback. The authors have concluded that finance and resources are key integral aspects of the EBP culture sustainability.Although there have been studies investigating financial management practices and evidence-based practice culture, the studies have failed to understand the relationship between them. Additionally, there is a gap in the literature that focuses on determining the relationship between financial management practices and evidence-based practice culture. Therefore, this study aims to identify the relationship between financial management practices and evidence-based practice culture, specifically answering the following question:1. Is there a significant relationship between financial management practices and evidence-based practice culture among nurse managers?2. Is there a significant difference on financial management practices among nurse managers when years of experience are considered?
2. Methodology
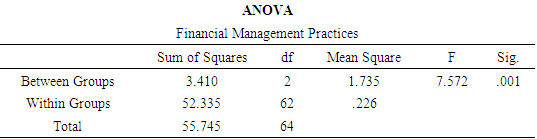
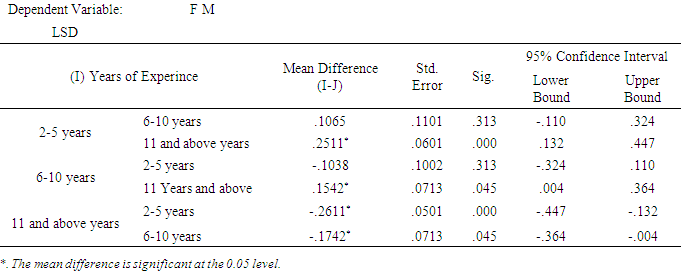
- The study used a correlational research design to examine financial management practices and evidence-based practice culture among nurse managers in Ghana. The researchers used a random sampling technique to sample 64 nurse managers in four selected hospitals in Ghana. The inclusion criteria are nurse managers who been a manager for a hospital for about two years. The exclusion criteria are nurse managers who have to manage a hospital for less than two years.Out of the 64 managers, 45 (70.3%) were male, 19(29.7%) were males. The working experiences of the respondents showed that from 2-5 years was 10 (16.67%), from 6-10 years was 20 (33.33%), and 11 years and above was 30 (50%). A 35-item 5-point Likert scale was used to assess financial management practices (‘1' = highly not typical of me, ‘5' = strongly typical of me). An evidence-based practice questionnaire developed by (Dominic and Penney Upton 2006) which consists of 24 items were used to examine the evidence-based practice culture of the nurse managers. The reliability measurement based on the internal consistency by using Cronbach Alpha resulted that financial management practices were .885 and evidence-based practice culture was .905.In determining the strength of the relationship Cohen (1998), absolute correlation valves where r=.10 to .29 meaning small or low, r=.30 to .49 are medium or moderate, and r=.50 to 1.0 is large or high interpreted were used.Two research assistant was employed from Ghana. Nurse managers were approached from the four selected hospitals in Accra. The research assistants explained the purpose and procedure of the study before distributing the questionnaires. The questionnaires were collected and sealed after completion. The research assistant encoded the raw data and sent them using the google form for statistical treatment. Nurses’ managers' privacy was protected by providing anonymous and voluntary participation. The purpose of the study was explained, and consent would be obtained before data collection. Participants had the right to withdraw from the study at any stage. Furthermore, the identification of the participants was not disclosed, and only aggregate data were presented. Ethical consideration was taken into account during the study from the four selected hospitals.The study used the Statistical Package for Social Sciences (SPSS) version 22 to analyze the data. Pearson Correlation Coefficients were used to determine the relationship based on their strength and direction of financial management practices, and evidence-based practice culture. ANOVA was used the to determine the significant difference on financial management practice when years of experience was considered.
3. Results
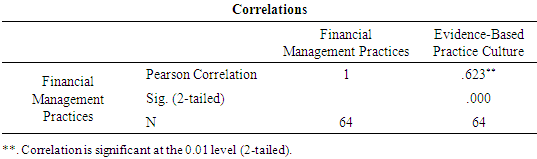
- Pearson correlation coefficient was used to examine the research question to determine the relationship between financial management practices and evidence-based practice culture. The relationship between financial management practices and evidence-based practice culture showed a high significant positive relationship (r=.623, p=0.000) at a 95% confidence interval. This means that as the evidence-based practice culture of the registered nurse managers increases, the financial management practices also increase. The results confirm Kueny et al. (2015), Li et al. (2018), and Sharplin et al. (2019) studies that suggest that financial management practices have a significant relationship towards evidence-based practice culture.
|
|
|
4. Discussion
- The study concluded that there is a high positive relationship between financial management practice and evidence-based culture. The results suggest that as the financial management practices increase among nurse managers, so does the evidence-based practice culture of the institution. In terms of years of managerial experience, nurse managers with higher managerial experience had good financial management practices. The sustainability of evidence-based practice culture and research utilization creates a clinical environment in which evidence supports clinical practice and administrative decisions, ensuring the highest quality of care by using evidence to promote optimal outcomes, reduce inappropriate variation in care, and promote patient and staff satisfaction. The financial resource is a key element that allows an evidence-based practice to be sustainable in the clinical practice. Nurse managers plays a critical role in promoting an evidence-based practice culture through their financial management practices. Therefore, this study concludes that in order to enhance and sustain the evidence-based practice cultures of health institutions, nurse managers should practice positive financial management practices. It is therefore critical for continuous professional development among nurse managers to include the development of financial management. Additionally, nurse managers with higher managerial experience should provide mentorship to novice nurse managers. Further research should investigate using qualitative research design on the challenges that nurse managers face in sustaining an evidence-based practice culture in the clinical setting.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML