-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2021; 11(1): 20-30
doi:10.5923/j.nursing.20211101.03
Received: Apr. 12, 2021; Accepted: Apr. 28, 2021; Published: May 15, 2021

Resilience and Burnout among Registered Nurses in Ghana during Covid- 19 Pandemic
Blesslove Pinamang Nimako
Saint Louis University, Baguio, Philippines
Correspondence to: Blesslove Pinamang Nimako, Saint Louis University, Baguio, Philippines.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

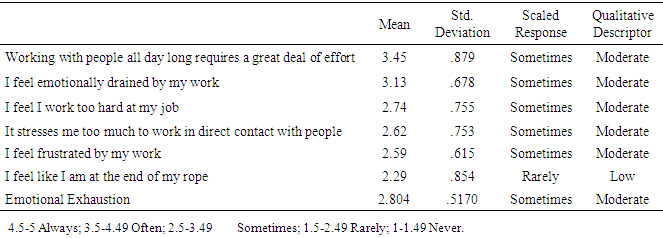
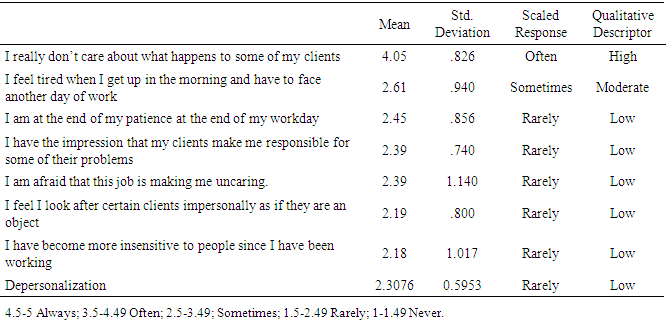
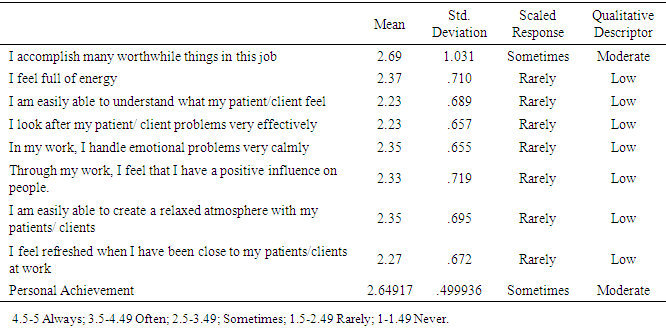
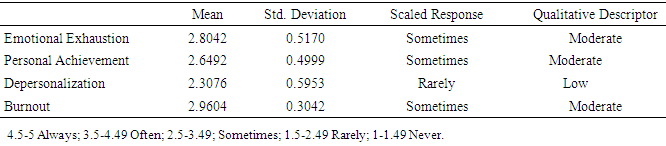
The COVID-19 pandemic wreaked havoc on healthcare systems, increasing the risk of psychological trauma among healthcare professionals, especially nurses. While mental health issues are an unavoidable part of life, they have become more severe and widespread among nurses as they battle COVID-19 on the pandemic's front lines. With having to carry the fear and burden associated with Covid- 19, and an increasing workload, nursing shortages, and long working hours, burnout is a significant concern among nurses. Initial evidence suggests that resilient nurses display distinctive qualities that help them adapt successfully to disturbances that threaten their function, viability, and development. This descriptive-correlational study aimed at examining the relationship between resilience and burnout among registered nurses in Ghana during the Covid- 19 pandemic. The study utilized 239 registered nurses from three selected hospitals who work in the Medical units, Surgical Units, Emergency units, and Intensive Care Units, using a purposive sampling technique. Data were collected through an online survey, using the 14- Item Resilience Scale (R.S.- 14) and the Maslach Burnout Inventory (M.B.I.) with the reliability of .888, and 0.840, respectively. Data were analyzed descriptively using means, standard deviations, Pearson Correlation, and ANOVA. Results showed that nurses have high resilience (M=3.9105, SD=0.4941) and moderate burnout (M=2.9604, SD=0.3042) level during the Covid-19 pandemic. Analysis of burnout’s sub-variables showed that nurses experience a moderate level of emotional exhaustion (M=2.804, SD=0.5170) and personal achievement (M=2.64917, SD=0.499936), while depersonalization (M=2.3076, SD= 0.5953) was low. The relationship between resilience and burnout showed a negative relationship (r= -.751, p= .026) at a 95% confidence interval, in that, as resilience increases, burnout decreases, and vice versa. Nurses working in the accident and emergency unit experienced a higher level of burnout than nurses in other clinical units, while those with clinical experience of 10 years and above experienced a high level of burnout than other groups. The study recommends that nurse managers and administrators provide opportunities for nurses to receive oriented training, learn new skills, and promote self-care, self-efficacy, and resilience among nurses through continuous professional development. Furthermore, to reduce nurse burnout, lower turnover rates, and improve nurse-patient outcomes, support systems in the nursing work environment should be strengthened; administrators should ensure a healthy workplace with an accurate nurse-patient ratio, appropriate workload, and appropriate working hours. Future research should look into the factors that lead to nurse burnout in Ghana, including individual, environmental, and COVID-19-related factors.
Keywords: Resilience, Burnout, Registered nurses, Emotional Exhaustion, Covid- 19 pandemic
Cite this paper: Blesslove Pinamang Nimako, Resilience and Burnout among Registered Nurses in Ghana during Covid- 19 Pandemic, International Journal of Nursing Science, Vol. 11 No. 1, 2021, pp. 20-30. doi: 10.5923/j.nursing.20211101.03.
Article Outline
1. Introduction
- The COVID-19 outbreak is a major global public health emergency that has put global and national healthcare systems to the test, overburdening and endangering healthcare professionals’ wellbeing, especially nurses. According to the World Health Organization (W.H.O., 2021), there have been more than 123 million confirmed cases and over 2.71 million confirmed deaths in 223 countries, with over 35,000 confirmed cases involving health care workers. There are also approximately 3 million confirmed cases of Covid- 19 and over 76 000 deaths (W.H.O., 2021) in Africa. In Ghana, reports from the Ghana Health Service (G.H.S., 2021) indicate more than 89,000 confirmed cases and over 700 deaths since the emergence of Covid- 19. According to the World Health Organization (2020), the high incidence of Covid-19 cases has overburdened the healthcare system, resulting in an unexpected global demand for healthcare and healthcare professionals. While mental health issues are an unavoidable part of life, they have become more severe and widespread among health care workers as they battle COVID-19 on the front lines during the pandemic. During a global epidemic of infectious disease, healthcare professionals play a crucial role in patients' clinical treatment, preventing infection transmission, and the restoration of health. As a result, they encounter significant challenges associated with healthcare delivery services, which can be disruptive to their mental health (Driggin et al., 2020).As nurses constitute the majority of the healthcare workforce, they provide roughly 3/4 of all healthcare services in the hospital. According to Yörük and Güler (2021), the nursing force is heavily burdened with the ever-growing stress associated with the Covid-19 pandemic due to the increasing demand for health care, an increasing number of patients they supervise, heavy and demanding workloads, long working hours, poor staffing ratios, lack of personal protective equipment, lack of communication between physicians and nurses, increasing nursing activities, and lack of organizational leadership within working environments for nurses (Al-Omari et al., 2020). As a result, compared to other healthcare workers, nurses face tremendous mental health problems and have the highest levels of psychological distress, depression, anxiety, and burnout, affecting nursing care, nursing performance, productivity, and patient outcomes (Walton, Murray & Christian, 2020). The World Health Organization (2019) defines burnout as a condition conceptualized due to persistent pressures in the workplace that workers do not handle effectively. Globally, previous studies have shown high burnout levels among nurses, and have reported that about 60% of nurses leave or have intentions to leave their profession due to physical burdens, high occupational stress, burnout, and emotional exhaustion (Hämmig, 2018; Moloney, Boxall, Parsons & Cheung, 2018; Khamisa, Peltzer, Ilic & Oldenburg, 2016). A cross-sectional survey of 50,273 nurses suggested that burnout is a significant problem among nurses in the United States, as respondents who reported leaving or considering leaving their job due to burnout and stressful work environment were 68.6% and 59.5%, respectively (Shah et al., 2021). A recent cross-sectional survey of 2,014 nurses by Hu et al. (2020) investigated frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China. This study showed that 91.2% of nurses reported moderate to high burnout levels in Wuhan. Similarly, Mastuo et al. (2020) found out that about 47% of nurses experienced high burnout levels during Covid- 19 outbreak in Japan. Odonkor and Frimpong (2020) assessed burnout among health care professionals in Ghana in a cross-sectional study among 365 respondents who worked in 12 major healthcare facilities. Among the health worker groups, nurses had the highest percentage score values for all burnout variables, with 88.6%. However, this study did not investigate burnout in the Covid- 19 pandemic context and focused on burnout among health care professionals, not registered nurses solely. In another study, Poku, Donkor, and Naab (2020) found out that out of the 232 registered nurses studied, 91.1% experienced moderate to high emotional exhaustion rate. However, this study did not investigate the other two dimensions of burnout; depersonalization and perceived personal achievement. Previous studies have shown substantial evidence that resilience has protective effects against burnout (Zou et al., 2016; Brown, Walters & Jones, 2019; Yu et al., 2019). However, the relationship between these phenomena has not been established during the Covid-19 pandemic in Ghana. Other significant limitations of previous studies include burnout studies conducted out of the context of the Covid-19 pandemic and another which examined only emotional exhaustion, one dimension of burnout. Furthermore, literature searches regarding resilience and burnout among registered nurses are significantly scanty in Ghana. Therefore, it is relevant and novel to conduct a study to establish the relationship among nurses, especially during the Covid- 19 pandemics where nursing workloads are demanding, and nursing work conditions are unpredictable in Ghana. Therefore, this study investigated the relationship between resilience and burnout among registered nurses in Ghana during Covid- 19 pandemic. Specifically, it answered the following questions;1. What is the level of resilience among registered nurses in Ghana during the Covid- 19 pandemic?2. What is the level of burnout among registered nurses in Ghana during Covid- 19 pandemics in terms of a) Emotional Exhaustion?b) Depersonalization?c) Perceived Personal Accomplishment?3. Is the relationship between resilience and burnout among registered nurses in Ghana during Covid- 19?4. Is there a significant difference in burnout among registered nurses in Ghana during Covid- 19 pandemics when considering; a) Clinical Area?b) Years of working experience?Hypothesis 1. There is no significant relationship between resilience and burnout among registered nurses in Ghana during Covid- 19 pandemics.2. There is no significant difference in burnout among registered nurses in Ghana when considering Units of assignment and years of working experience.
2. Literature Review
- Workplace adversity may be harmful, frustrating, or traumatic, putting nurses in challenging circumstances or causing them to suffer. Despite the many obstacles in healthcare delivery, resilience is a vital characteristic that allows nurses to thrive and cope with their work environments while maintaining safe and stable psychological functioning. (Brennan, 2017). The American Psychological Association (2014) describes resilience as one’s capacity to respond well in the face of hardship, trauma, disaster, challenges, or even primary stress sources. Oshio, Taku, Hirano, and Saeed (2018) define resilience as a trait that a person exhibits or possesses as a resilient attribute or feature in their personality, while Foster, Cuzzillo, and Furness (2018) describe resilience as a mechanism by which people establish strategies to resolve adversity.According to Collette and Ungar (2020), resilience is a complex process of positive adaptation which involves an individual’s ability to adapt effectively to disruptions that threaten system operation, viability, or growth. Various forms of resilience include psychological resilience, emotional resilience, and physical resilience. Psychological resilience characterizes the capacity to withstand or adjust to uncertainty mentally, and it entails the implementation of a variety of meta-cognitive and emotional processes to protect people from the adverse effects of stress (Yörük & Güler, 2021). Kuntz, Malinen, and Näswall (2017) posit that emotionally resilient people understand what they are feeling and why, and as a result, can maintain realistic optimism even in the face of a crisis, and are proactive in utilizing both internal and external resources to manage stressors and emotions in a healthy, positive manner. When dealing with illness, accidents, or other physical demands, physical resilience refers to the body’s ability to adjust to difficulties, retain endurance and power, and heal rapidly and efficiently (Näswall et al., 2019). Resilience has been researched most widely as an individual psychological construct, according to evidence reviews in the broader field of nursing, with conceptualizations ranging from resilience as a capacity or community of personal characteristics to resilience as a phenomenon between individuals and their environment (Delgado et al., 2017). Individual and intrapersonal attributes known to enhance nurses’ resilience include self-control, faith, spirituality, hope, coping, self-confidence, compassion, awareness, and self-efficacy (Ang et al., 2019).Traynor (2017), on the other hand, acknowledges that resilience requires critical interactions between nurses and their work environments and includes organizational support and resources, social networks, and services. Several research studies show that work-life balance, cognitive reframing, a clear sense of professional identity, accessing resources, and supportive relationships with others are effective resilience-building techniques in nursing (Foster et al., 2019; Rivard & Brown, 2019; Delgado et al., 2017). According to Tuck, Manssuer, and Philip (2020), nurses engaged in primary care are overloaded by the complexity of the clinical challenges and other patients’ conflicts. Despite the challenges, resilient nurses can maintain a positive attitude toward their patients, perform their duties realistically, and have effective stress-reduction strategies. Smith and Yang (2017) posit that there is a link between resilience and general wellbeing, personal quality of life, working relationships, psychological wellbeing, and job satisfaction.According to Mcdermott et al. (2020), greater resilience levels may help boost or enhance positive intrapersonal and interpersonal strengths. In contrast, low resilience is associated with mental outcomes such as depression, burnout, exhaustion, and psychological distress. A cross-sectional study of 1356 nurses by Ren et al. (2018) from 11 general hospitals in Guangzhou, China, showed that nurses had low resilience and could not effectively cope with job challenges and recover from adversity. Researchers, therefore, recommended the need to reduce job stress, enhance training, and strengthen self-efficacy. In the study of Jose, Dhandapani, and Cyriac (2020), researchers found out that nurses in the emergency unit experienced a moderate-to-severe level of burnout in emotional exhaustion and depersonalization during the Covid pandemic, but a mild-to-moderate level of burnout in reduced personal accomplishment and showed a moderate to a high level of resilience. This study concluded a significant negative correlation between resilience and burnout among frontline nurses during the Covid pandemic. In a recent study, Roberts et al. (2021) found that about 18.9% of nurses in the U.K. have low resilience during the Covid- 19 pandemic, and further revealed that younger nurses with less experience have higher levels of anxiety and depression and had lower resilience. Burnout syndrome is conceptualized as a condition exacerbated by prolonged susceptibility to stress at work that negatively affects wellbeing and quality of life, patient outcomes, and performance. According to Gribben and Semple (2020), due to the demanding nature and high emotional demands of nursing work, about one-third of nurses report exhaustion and burnout in their workplaces. In the early 1970s, Dr. Herbert Freudenberger coined the term “burnout” and described it as a long-term response to work-related emotional and interpersonal stress. Maslach & Leiter (2017) categorizes burnout under three sub-dimension; emotional exhaustion, depersonalization, and lack of personal accomplishment. The most investigated dimension, emotional exhaustion, involves being physically and emotionally drained and exhausted intensely, resulting from repetitive work, personal demands, and ongoing tensions (Kinman & Leggetter, 2016). Maslach & Leiter, 1981 described depersonalization as a cold and skeptical demonstration of separation from the service recipient (patients) by deliberately ignoring the attributes that make them unique and engaging individuals. Gharakhani & Zaferanchi (2019) describe reduced personal accomplishment as the propensity to judge the value of one’s work negatively, feeling inadequate in terms of the capacity to perform one’s job, and a generalized low professional self-esteem.According to research studies, burnout among nurses is intrinsically linked to work-related factors and secondarily to personality factors (Shanafelt et al., 2017; Bianchi, 2018; Dounavi, Fennell & Early, 2019). Work-related factors contributing to burnout include heavy workloads, rewards and incentives, conflicts between the nurse and organizational values (Wang et al., 2020), nurse-physician conflicts, lack of feedback and support, nurse-patients conflict, ineffective teamwork communication, and work-family conflicts (Brown, Walters & Jones, 2019). Personal-related factors that influence burnout include age, gender, hardiness, coping skills, self-efficacy, years of working experience, and educational level (Yu et al., 2019).In a cross-sectional study, Putra (2019), among a sample of 485 nurses in medical and surgical units in Indonesia, showed high levels of burnout among 24.3% in terms of emotional exhaustion, 24.5% depersonalization, and 34.8% had reduced personal accomplishment. Correlation analysis further found marital status and working experience as factors associated with burnout. Cañadas-De la Fuente et al. (2015) also reported average to high burnout levels among 676 nurses in Spain, and risk factors of burnout included age, gender, marital status, and type of shift work. In Greece, a cross-sectional survey by Lahana et al. (2017) among 180 nurses showed that female nurses had a higher personal accomplishment score than men. Comparatively, it has been established that there is a significant negative relationship between burnout symptoms and resilience, which sheds light on the role of resilience in influencing burnout. In China, Kim and Choi (2016) found out high prevalence of burnout among emergency nurses, which was associated with job stress, limited hospital resources, and inadequate support from family. Similarly, Intensive Care Unit (I.C.U.) and emergency departments, a study by Cishahayo, Nankundwa, Sego, and Bhengu (2017) showed high emotional exhaustion (48.3%), high depersonalization (25%), and low personal accomplishment (50%).Similarly, in a total of 366 Chinese female nurses, Zou et al. (2016) investigated the association between resilience, burnout, and psychological distress, where results showed that 85. 5% of nurses experienced psychological distress. While resilience correlated negatively to psychological distress and burnout, burnout was positively associated with psychological distress.
3. Methodology
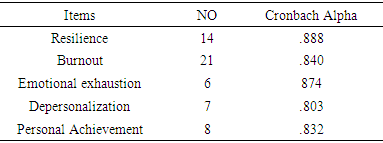
- This quantitative study utilized a descriptive- correlational design to examine resilience and burnout among registered nurses in Ghana during the Covid-19 pandemic. The study used 239 registered nurses from three selected hospitals in Ghana who were purposively sampled to answer questionnaires through google forms. Inclusion criteria for respondents were; a) must be a registered nurse, b) must work in a Medical unit, Surgical unit, Emergency unit, Intensive Care Units, and c) must have at least one year of working experience. Exclusion criteria were a) nurse supervisors and administrators, b) nursing students and attendants, and c) nurses with less than a year of working experience.The study adopted the 14- Item Resilience Scale (R.S.- 14) to measure nurses’ resilience level, an instrument developed by Wagnild & Collins (2009). The brief 14-item version of the original instrument is rated on a 5-point Likert scale and comprises 14 items ranging from 1 (Never) to 5 (Always). The RS-14 comprises five items referring to “self-reliance” (4,6,10,12 and 13), three items referring to “meaningfulness” (1, 3, and 7), two items referring to “equanimity” (5 and 14), two items referring to “perseverance” (2 and 9) and two items referring to “existential aloneness” (8 and 11).
|
|
|
4. Results and Discussion
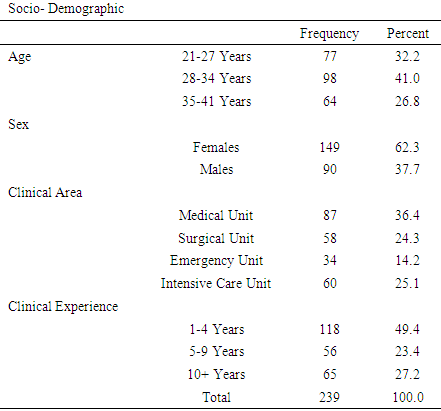
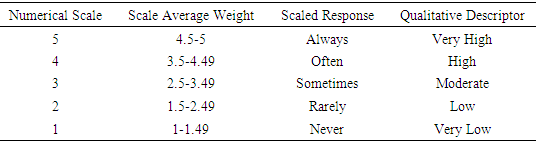
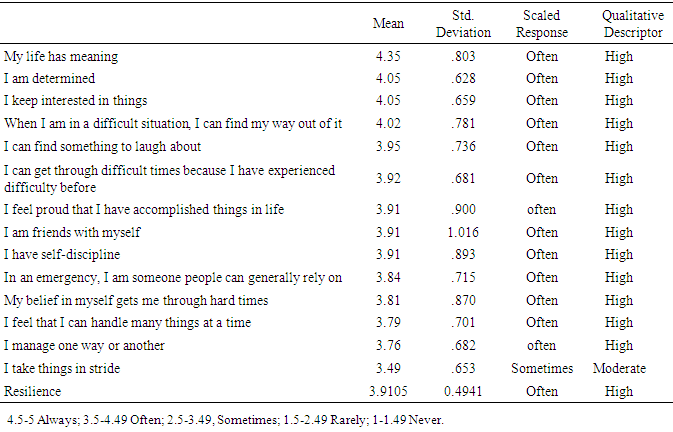
- The sociodemographic characteristics of respondents are presented in Table 1. In the present study, most of the respondents (41%) were between the ages of 28 and 34years. While 149 (62.3%) of them were females, most of them (39.4%) worked in the medical unit, and the majority (49.4%) had 1-4 years’ clinical experience. Resilience was quantified using 14 questions. In Table 4, the overall scaled response for resilience was often a qualitative descriptor as high (M=3.9105, SD=0.4941). In a detailed analysis, the highest scored item was “my life has meaning,” with a scaled response of always and qualitative descriptor as high (M=4.35, SD=0.803). The lowest scored item was I take things in stride, with a scaled response of sometimes and qualitative descriptor as average (M=3.49, SD=.653). This implies that nurses have a high level of resilience during the Covid-19 pandemic. These results contradict the study of Jose, Dhandapani, and Cyriac (2020), where nurses reported a moderate to a high level of resilience.
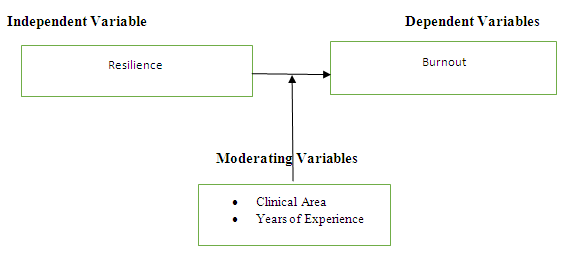 | Figure 1. Conceptual framework on Resilience and Burnout |
|
|
|
|
|
4.1. Relationship between Resilience and Burnout
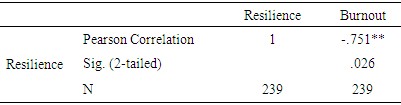
- Pearson correlation coefficient was used to examine the relationship between resilience and professional burnout. In Table 9, the relationship between resilience and professional burnout showed a negative relationship (r= -.751, p= .026) at a 95% confidence interval. This means that the higher the resilience, the lower the professional burnout of the registered nurses. The study fails to rejects the null hypothesis that there is no significant relationship between resilience and professional burnout. The study is consistent with Jose, Dhandapani, and Cyriac (2020), which showed a negative relationship between resilience and burnout among frontline nurses during Covid- 19 pandemic.
|
4.2. Difference in Burnout when Considering Clinical Area
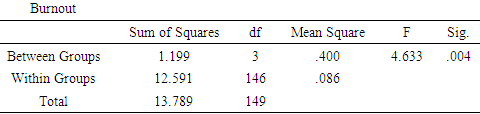
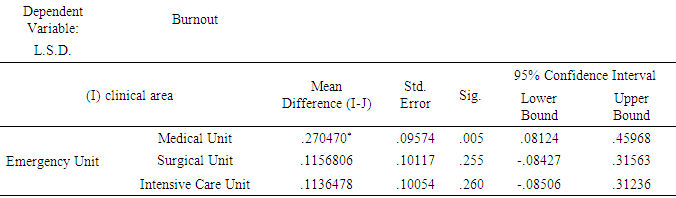
- A one-way between-group analysis of variance was performed to investigate the clinical area's impact on burnout, illustrated in Table 10 and Table 11. Participants were divided into four groups based on their clinical specialty. Group 1 is the medical unit, Group 2 is the surgical unit, Group 3 is the emergency unit, and Group 4 is the intensive care unit. There was a statistically significant difference at the p> 0.004 level in the clinical area's burnout score: F= 4.633. Despite reaching statistically significant, the actual difference in mean scores between the groups was small. The effect size, calculated using eta squared, was 0.104. Post- hoc comparison using the LSD test indicated that the mean score for Emergency unit (M=3.1342, SD=0.2222) significantly different from intensive unit (M= 3.0206, SD= 0.2900), surgical unit (M= 3.0185, SD= 0.3657) and medical unit (M=2.8637, SD=0.2593). The study rejects the null hypothesis that there is no significant difference in professional burnout when considering the clinical area.
|
|
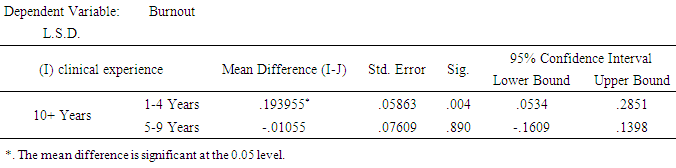
4.3. Difference in Burnout when Considering Clinical Experience
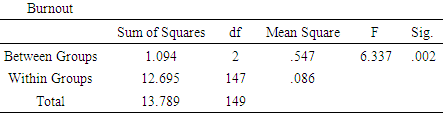
- A one-way between-group analysis of variance was conducted to explore the impact of clinical experience on burnout. Participants were divided into three groups according to their clinical experience. Group 1: 1 to 4 years; Group 2: 5 to 9 years; and Group 3: 10 years and above. As shown in Table 12 and Table 13, there was a statistically significant difference at the p> 0.002 level in burnout score: F= 6.337. Despite reaching statistically significant, the actual difference in mean score between the groups was moderate. The effect size, calculated using eta squared, was 0.086. Post- hoc comparison using the LSD test indicated that the mean score for 5-9 years (M=3.0696, SD=0.3395) significantly different from 10years and above (M= 3.0590, SD= 0.2077), and 1-4 years (M= 2.8898, SD= 0.3080). Therefore, the study rejects the null hypothesis that there is no significant difference in professional burnout when considering clinical experience.
|
|
5. Conclusions and Recommendations
- The study aimed to look into the relationship between resilience and burnout among registered nurses during the Covid-19 pandemic. According to the results, registered nurses have a high level of resilience and a moderate degree of burnout during the Covid- 19 pandemic. Compared to other countries, burnout levels may have been moderate because Covid-19 cases are not as prevalent in Ghana, and the workload may not be as extensive as in countries where Covid-19 cases are prevalent. The study also showed a negative relationship between resilience and burnout, implying that when nurses’ resilience level increases, their burnout decreases. Conversely, as resilience decreases, burnout levels increase among nurses. The study’s results also revealed that nurses working in accident and emergency units had a higher level of burnout in the clinical area than those in medical, surgical, and intensive care units. Furthermore, nurses with 10 years or more of clinical working experience were more burned out than those with 1 to 4 and 5 to 9 years of clinical experience.The study recommends that nurse managers and administrators provide opportunities for nurses to receive training and learn new skills to promote self-care, self-efficacy, and resilience among nurses through continuous professional development. Furthermore, to reduce nurse burnout, support systems in the nursing work environment should be strengthened, and administrators should ensure a healthy workplace with an accurate nurse-patient ratio, appropriate workload, and appropriate working hours. Future research should look into the factors that lead to nurse burnout in Ghana, including individual, environmental, and COVID-19-related or pandemic-related factors.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML