-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2020; 10(3): 62-73
doi:10.5923/j.nursing.20201003.02
Received: Sep. 22, 2020; Accepted: Nov. 3, 2020; Published: Nov. 28, 2020

The Role of the Nurse Administrator in Healthcare Services and Healthcare Built Environment in Southern Nigeria
Gloria Tonye Dikibo
Nursing, Texila American University (Distance and Blended Learning) Tamilnadu India, Port Harcourt, Rivers State, Nigeria
Correspondence to: Gloria Tonye Dikibo , Nursing, Texila American University (Distance and Blended Learning) Tamilnadu India, Port Harcourt, Rivers State, Nigeria.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

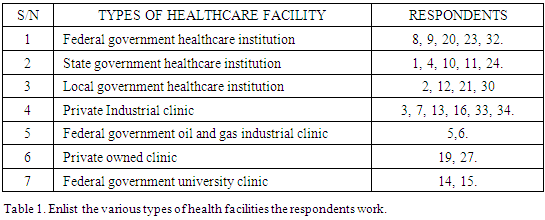
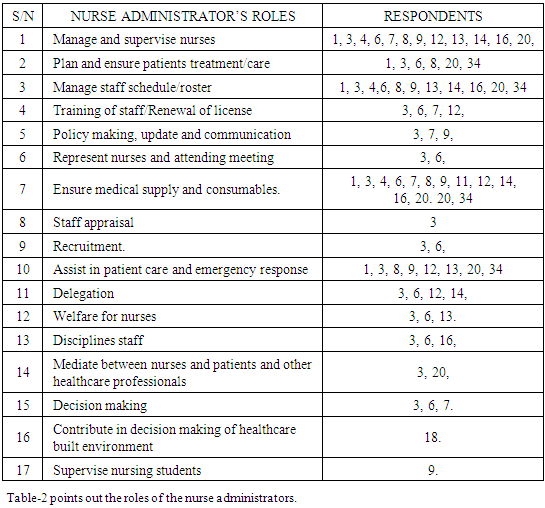
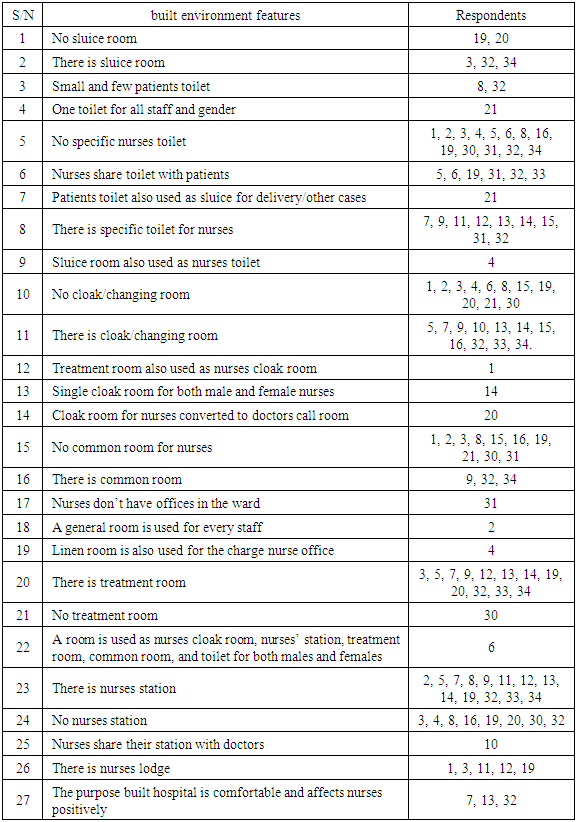
The concept of healthcare built environments has been underrated which is responsible for deplorable design of most healthcare facilities in Southern Nigeria. The Role of the Nurse Administrator in Healthcare Services and Healthcare Built Environment in Southern Nigeria is a descriptive and observational capstone project, a study conducted using telephone interview method with self- structured open-ended questions for a cross -section of nurses in the clinical, educational and administrative areas in the three states (Bayelsa, Edo and Rivers state) of Southern Nigeria. Total respondents were thirty-five (35), nurses 30 (85.7%) (28 (93%) females and 2 (6.7%) males); medical doctors 3 (8.6%), civil engineer 1 (2.9%) and architect 1 (2.9%) all males. Data collated for healthcare built environment used by nurses revealed: 46.4% are without specific built nurses’ toilet, 39.2% are without cloak room, 21.4% use patients toilet, 28.6% are without nurses’ station, and only 10.7% nurses stated they are comfortable with the purpose built and ideal healthcare environment and how it has affected them positively. For Nurse Administrators’ role 7.1% represent the nurses and attend meetings, 10.7% are involved in decision making, 3.6% contributed in healthcare built environment design and only 6.7% of the nurses have actually influenced built environment planning design. s. Research has also shown a strong link between the design of healthcare settings and outcomes experienced by patients, staff, and families. Hence the need to create the awareness and include nurse administrators and clinical nurses as frontlines to ensure their voices are heard in influencing decision among other professionals in creating innovative design in healthcare built environment to enhance workflow processes, work environment outcome, patient and provider safety and outcome.
Keywords: Nurse Administrator, Role, Healthcare built environment, Healthcare services
Cite this paper: Gloria Tonye Dikibo , The Role of the Nurse Administrator in Healthcare Services and Healthcare Built Environment in Southern Nigeria, International Journal of Nursing Science, Vol. 10 No. 3, 2020, pp. 62-73. doi: 10.5923/j.nursing.20201003.02.
Article Outline
1. Introduction
- As part of corporate social responsibility, a renowned federal government organization built a health facility to promote maternal and child health for one of their host community in southern Nigeria; and prior the opening ceremony in 2018 employed the services of an obstetrician/gynaecologist to confirm the architectural design of the built environment. However, the obstetrician requested and was be accompanied by a nurse. At the end of the facility tour, it was discovered, that most of the units and settings missed out in the construction are units related to nursing department, such as, first stage room, sluice, treatment room, examination room, nurses office/station and convenience. This experience spurred the project title, the role of the nurse administrator in healthcare care services and healthcare built environments in a cross section of states in, Southern Nigeria.The research was conducted using, direct observation research, and interview method with thirty- five (35) respondents. The self-structured interview question used for nurse respondents covers demographic data, the role the nurse administrator in the healthcare services, the role of nurse administrator in healthcare built environments, the operational built environment design and condition of the facility in which they are working in respect to nurses’ station, nurses rest room, patient physical examination room, treatment room, cloak room, sluice room and common room. Some healthcare facilities were visited to see the type of built environment. Nurses of various ranks in the clinical and other fields working in different health institutions from federal government teaching hospitals, state general hospitals, local government primary healthcare centers, private and multinational company’s industrial clinics, military hospital, school health centers/sickbays, foreign base owned industrial clinic, private owned clinics and the ministry of health were interviewed, on the role of the nurse administrator in health care services and the healthcare built environment design as it relates to nursing and healthcare delivery.
1.1. Aim of the Study
- Elicited data on the role of the nurse administrator in healthcare built environment; is intended to determine the need to create awareness among nurses on this role as frontlines and also the need to ensure their voices are heard among other environment of care professionals, and staffs in the evidence based design planning and construction of the healthcare built environment to improve safety for patient and provider, clinical outcomes for patients and job satisfaction for nursing staff.
2. Methodology
- The study is descriptive and observational, using self - structured interview questions for a cross - section of nurses in the clinical, educational and administrative areas and direct observation.
2.1. Interview
- The interview was in two segments. The first segment is expected to provide demographic answers to years of experience, sex, age, educational qualification, area of specialty and service; while the second segment was guided open ended questions that allowed the respondents to enlist the nurse administrator roles and to describe their healthcare structural architectural design setting in terms of nurses station, cloak room, treatment room, toilet, and offices.Telephone interview was used with the highlighted questions: What is the role of the nurse administrator in the healthcare facility? Is the architectural design layout planning considerate of nurses in terms of nurses station, nurses common room, rest room, cloak room, treatment / utility rooms, and sluice room in the healthcare facility? Are nurse administrators consulted for their input in the design planning and are they members of the architectural design planning team of the healthcare facility? What are the types of healthcare services rendered in the facility? The study was conducted with nursing staff and leaders randomly across private owned clinics, primary health care centers, state general hospitals, federal hospitals industrial clinics, and ministry of health in south-south Nigeria, to elicit the role of the nurse administrator in health care services and healthcare built environment design planning.
2.2. Direct Observation
- A model primary health care center in Port Harcourt metropolis, an industrial clinic Accident and Emergency unit in Rivers state, a primary healthcare center in Bayelsa and industrial clinic at Edo state in Southern Nigeria were the samples for direct observation research. Thirty (30) nurses working at different healthcare institutions across the three southern states of Nigeria were randomly interviewed with informed consent, alongside a civil engineer, an architect, and three medical doctors, making a total of 35 respondents.Observation and interview for this study were conducted in August 2019 and May-June 2020 respectively. Collated data was analyzed, arranged and presented in quoted words, percentages, pictorials, tables and graphs, for better elucidation and interpretation. Registered Nurses, Registered Midwives, nurses with clinical work experience, nurses working in healthcare facilities where patients are hospitalized, healthcare facilities where nursing care is rendered 24 hours and 7 days in a week; healthcare facilities and institutions with nurse administrators, ministry of health, Civil engineer that has built healthcare facility, architect who has designed healthcare facility, practicing medical doctors, Healthcare facilities/institutions in Bayelsa, Edo and Rivers state, (three southern states Nigeria) owned and managed by government in the federal, state and local government levels; multinational Industrial clinics managed by foreigners and those co -managed by the locals. Facilities built or owned privately by medical doctors.The study and purpose of the interview were explained to respondents and their confidentially assured before they consented.
2.3. Respondents Interview Response
- -1-(Rivers): A Registered Nurse and Midwife with 25 years’ work experience, female, within 40 -45 years of age, works in a local government general hospital that operates general out-patient and in-patient, clinic, surgery, maternal and child health without immunization. She listed nurse administrator (Chief Nursing Officer-[CNO]) roles: “oversee nurses, ensures every shift is covered and nursing care/treatment rendered accordingly, provides consumables and “mans” the family planning clinic”. For facility architectural design : “The building is an old pattern, no rest room for nurses, no cloak or common room, and the treatment room is converted to a place where nurses keep their belongings”. Presently the staff quarters are being renovated. The CNO is also carried along.”2(Rivers) This second respondent is within 40 and 45 years, a registered nurse and midwife, female, with work experience of 19 years, works in a local government primary health center. Services rendered are within the scope of maternal and child health-immunization, maternity and family planning. For response about healthcare setting, "Apart from the station for assessment of vital signs, no purpose built common room for nurses, but there is a general room for every staff of the health center.”-3-(Edo) The respondent is within 30-35 years, a female registered midwife with more than 10 years of working experience, in an industrial/family clinic that provides occupational health, maternal and child health services (immunization, antenatal, postnatal, family planning and reproductive health), family health nursing with referral system. Response to role of nurse administrator, addressed as the Nurse manager are consultation and referral system, deploys and overseas staff to and fro various sites, delegations and supervision of job descriptions and nursing procedures, roster preparation/work schedule, objective setting and performance appraisal, maintenance of quality and continual improvement, requisition and supply of consumables and medical equipment, recruitment and staff welfare. Health campaigns and sensitization, communication of healthcare policy, staff training and recommendation for trainings, attend meeting and collects monthly statistics and report from all sites. “Response for healthcare setting design: “No purpose built nurses station, cloakroom, or rest room for nurses, unlike the consulting rooms for the medical doctor and nurse manager with restrooms. However, there are nurses lodge very close to the clinic.”Respondent -4-(-Rivers), is a female registered nurse and midwife with Bachelor of Nursing Science, age bracket 40-45 years, work experience of more than 19 years; working in a state specialist and teaching hospital. Her response during the interview was “we were working in a very critical unit, and the design setting of the unit is negatively affecting us. “No nurses’ station apart from an improvised table at the corner of the unit, it is mandatory we change into our work scrubs, but no changing room or cloak room to effect that, no toilet for nurses. The linen room is used as the nurse in charge of the unit office as well as the cloak room and common room where we eat and keep our belongings. No nurses toilet, at such the sluice room is also used as toilet.”Respondent -5-(-Rivers), a female registered nurse and midwife with BNSC, a staff of a national oil & gas company industrial clinic.20 years working experience and age bracket 40-45 years. Healthcare services rendered are occupational health, health promotion, emergency response, and disaster management, curative and referral system. Her response for the role of the head nurse in the facility includes “Requisition and supply of consumables, staff/shift management, attending safety meetings and emergency response.” For architectural setting design, she answered, “No nurses’ rest room so they use that of the patients, but there is cloak room, the nursing station is very far from the consulting room and medical record room.-6-(Rivers) The sixth respondent is within 45 - 50 years, a registered nurse and midwife, female, with 18 years of work experience. She works in a national oil and gas industrial and family clinic, with family planning, immunization, general out patient, general in patients, acute care unit, selected specialist clinic and referral system services. Her answer to the role of the manager in her facility is: “Requisition and supply of consumables and staff PPEs (personal protective equipment), in-service training for staff, recommendation of external trainings for staff and renewal of license, recruitment, deployment, general supervision, decision making, meeting with staff, ensure patients welfare and safety, represent the nurses in multidisciplinary meetings and collect monthly statistics/report from all the nursing units.” For health care infrastructure design, her response was –“The ER nurses do not have cloak room and common room for nurses, a cupboard was later built for nurses to keep their belongings, no rest room for nurses as they share with patients. One of the rejected private rooms with plumbing malfunction was converted to nurses station, cloak room, common room, rest room and treatment room for the general ward nurses.”-7-(Rivers) The seventh respondent, a female registered public health nurse and midwife and nurse, has a wide range of 20 years work experience, and falls within 40-45 years of age. She works in a foreign non-governmental Organization (NGO) industrial/occupational health service delivery institution, in charge of general out patient, adult immunization, and occupational health. During the interview she responded that “the nurse administrator is addressed as the clinical manager, who is involved in decision making, staff training, renewal of license, and policy updates.” For healthcare design setting she affirmed, ”their facility is purpose built with nurses’ station. Locker/cloak room, and rest room and everything is within their comfort.”Respondent -8-(Rivers), worked with a federal military healthcare parastatal operating general out patient, maternal and child health, in patients and surgeries. She is registered nurse and midwife, in view of BNSC; 17 years on the job and within the age of 35-40 years. According to her “the head nurse is addressed as matron and she acts in the capacity of provision of consumables, patients updates, prepares the staff roster, in charge of general supervision and gets order from the commander.” She further complained of in her words, “patients convenience that are small in sizes and few in number, no nurses room, no cloak room or rest room; the nurses station is just a table kept at one end of the open ward.” The 9th respondent (Edo) is a female registered nurse, midwife and public health nurse and family planning provider. She is within 40-45 years of age, has worked 20 years as a nurse, presently working in a medical ward in federal teaching hospital where the interview was conducted. In her response she stated “my leader is addressed as the ward manager, she does many things like supervising the nursing staff, nursing students, prepares roster and ensures each shift is covered, she is concerned with staff welfare, coaches and corrects nurses, does ward round, attend to patients sometimes, ensures proper patient care is delivered, supplies work materials and PPE, disseminates information and communicates adequately with staff. She uses group chat as well to notify when there upcoming activities like promotion exercise. For design setting, she is pleased with what they have “two changing room with lockers, two staff toilets, treatment room, nurses station, nurses office/common room.”The 10th respondent (Rivers) is a female registered nurse and midwife, working as a nurse for 19 years and within 40-45 years of age. She worked in an intensive-care unit of a state teaching hospital and stated “the substandard building of the unit is terrible and the government has already commissioned it, no room for nurses, no rest room either, the only work station is for both nurses and doctors, and doctors would want the nurses to release their seats when they come around, a very small room provided as cloak room does not have lockers and no form of ventilation when the air conditioner is off. The whole windows of the unit are sealed and there is no steady and regular power supply.”11-(Rivers). This respondent has 22 years work experience, and works as a senior nursing sister in one of the local government general hospitals. She is a registered nurse and midwife with a BNSC and within 40-45 years. In her interview she stated “the facility has nurses station, nurses restroom and staff quarters, although the structures are old fashion and some dilapidated and needs to be refurbished.” Furthermore she stated: “the Deputy Director (DD) who is nurse leader supplies consumables and does not make training input.” The healthcare services rendered are maternal and child health, HIV clinic, out - patient and in the patient clinic, surgery and immunization that is carried out by community health workers."Respondent -12-(Edo), she is the head nurse(matron) in charge of a primary health care center, a registered nurse and midwife and a family planning provider with more than 30 years working experience, and within 50-55 years of age. The facility engages in maternal and child health, vaccination and outreaches, HIV screening and follow-up, outpatient clinic, inpatient clinic, referral system, collaborate with WHO representatives, volunteers and trackers. Her roles are: attending meeting and training for vaccination update, documentation and family planning, locate traditional birth attendants and encouraged them to identify with the body that trains them on safe practice, she delegates staff for the same training, and she collects consumables and other commodities for use in the health center. Answers provided during the interview, “the healthcare center setting design is okay, as there is the matron’s office, nurses station and restroom and staff quarters.”Respondent -13-(Rivers), she works in a multinational oil and gas industrial and family clinic, a registered nurse midwife with associate degree. She is 40-45 years and 20 years on the job. The interviewee response includes “the head of the nursing unit is the nursing department head, her roles are roster preparation, staff welfare, supervision, and giving a helping hand where necessary.” For the infrastructure setting layout, she said, “the facility is purpose built, with nurses station, cloak room, nurses toilet, treatment room, nurses resting room and is well ventilated which has affected the nurses positively.”14-(Bayelsa) The respondent is from a government owned university sickbay providing school health, maternity and minor surgeries services to students and lecturers; a female registered nurse, midwife and public health nurse with BNSC, with more than 15 years of working experience and within 40-45 years. According to her ”the nurse leader is a CNO, who oversees other staff, delegate assignment, prepares roster and supply consumables.” For infrastructure design she noted, “The sickbay has nurses station, emergency case treatment room, convenience, and a cloakroom a single cloak room for both males and females.” -15-(Bayelsa) In this interview, the interviewee was engaged at home thus the following response: “The sickbay has nurses room, treatment room, sluice room and changing room.” She is a female registered nurse, midwife, public health nurse (PHN) with BNSC, that has put more than 16 years in the job. Her age also falls between 40-45 years.-(Rivers), The 16th respondent is a female registered nurse, midwife and public health nurse, with 19 years on the job experience and within 40-45 years of age. She works with a multinational industrial and family health clinic in the oil and gas sector. In response; “The head of nurse role is to spearhead the nursing staff, make roster, disciplines and provides consumables,” The healthcare design “has no nurses’ room, no common room, but there is changing room and kitchenette.-17-(Rivers)- She is a senior nurse administrator within 55-60 years, one time coordinator, Mandatory Continuous Professional Development Programme (MCPDP) in the state ministry of health and faculty of nursing in the state university. Her response during the interview was, “I hadn't been contacted for any assignment in healthcare design setting while in my acting capacity as Director of Nursing Services." -18-(Bayelsa)- This respondent was a former DNS (Director of Nursing Services), and presently a permanent secretary in the ministry of health. She affirmed the challenges of nurses with the health care structural design and the need for nurse administrators to speak up in the interview, “I am familiar with this case, and there were two occasions two multinational oil gas industry were building health facility, and the moment she came to the picture, she spotted there was no sluice room, and the project was suspended for six months, as nurses we should not just sit at a place we need to work up to ensure our voices are heard and we get what is rightly ours,” She also stated how she used her position and role to make positive changes in the educational sector like introduction of internship in school.-19-(Rivers) These responses was from a private healthcare facility staff. A female registered nurse and midwife, 48 years old with 22 years of working experience addressed as a matron (nurse administrator) of the facility. The purpose built facility does not have changing room, no toilet and common room for nurses. The treatment / examination room is the same that serves as the nurses’ station with a table and chairs.Respondent 20 (Bayelsa)is a nurse administrator as head of the ward, in a federal healthcare facility; she is within 40-45 years of age, has a well - rounded working experience of 18 years, a Registered nurse and midwife, midwife educator, public health nurse, with BNSC and MSN. According to her, her roles are, “supervising nurses, making roster, ensure nurses take care of patients, request for work equipment and material like sphygmomanometer, and weighing scale, mediating between nurses, doctors and patient in terms of misunderstanding and conflict, participate, in general, patient care, compound duty and preparation of patients for surgery sometimes.” For structural design the respondent mentions her ward does not have a changing room, the treatment room serves as changing room for nurses, nurses station is by the hallway with a table and some chairs. In another unit, a changing room for nurses was converted to call room for doctors.-21-(Rivers) In a Model primary healthcare center in the state capital, a voluntary midwife with 2 years working experience, within 35-40 years of age responded to her interview questions as follows: “The available rest room is for every staff, irrespective of the department and sex, no common room for nurses, the patient examination room is where nurses keep their belongings, no sluice room, but patients toilet is used as sluice for both delivery and other cases.”-22-(Bayelsa)- A representative of Nursing and Midwifery council of Nigeria to Rivers state. A male registered nurse with BNSC and a nurse administrator, within 45-50 years, with 19 years of work experience. In his response to the interview, he stressed that the nurse administrators are not involved neither carried along in the healthcare facility structural design setting, hence they don’t function in that capacity. He also stated that contracts are awarded and these health facilities are built. He however saw the need to create the awareness of this role in nurses through nurses’ forum.-23-(Rivers)- Head of nursing in a federal teaching hospital, when contacted was in a meeting and interview not conducted as further bookings failed.-24-(Rivers)- Director of Nursing services in a state teaching hospital, contacted on two occasions, none the less interview did not hold.-25th respondent is in Rivers state, lecturer, school of Nursing in the state level. A Female Registered Nurse and Midwife with BNSC and Masters. She falls within 45-50 years of age and 22 years working experience. Her response to introduction of students in decision making of healthcare infrastructure design planning was “the curriculum in nursing leadership is shallow and does not contain such topics, however during the next meeting/workshop with the council, this topic will be brought up to be discussed extensively”.-26-(Bayelsa) A practicing Plastic Surgeon, in a federal healthcare center, when asked about the role of nurses in the structural design and planning of the healthcare facility, revealed that “in Nigeria, doctors are also not consulted before coming up with the built medical facilities, as 98% of the healthcare facilities are awarded contracts. They only come to see a completed project, just like the very one where he is working.”-27-(Rivers)- This respondent owns a private clinic, he is a practicing anesthesiologist with a federal university teaching hospital. When asked about the role of nurse administrator/nurses in his built environment, his response was,” officially I did not consult any nurse for their input in the design, but I informally asked a nurse for her opinion in the areas that concern nurses.”Respondent -28-(Rivers) An architect and lecturer in the state Polytechnic, who is experienced in healthcare built environment, during his interview stated that, ” for every built environment the professionals or end users are ideally consulted in the planning and design. The architects, engineers, and users of the built environment had to meet for briefing before the design plan; prior to the briefing, the professionals –Hospital administrators, medical doctors, nurses pharmacist, laboratory scientist and others, are consulted through various means like observation, interviews and so on, to be conversant with the ideal facility needed and the usage; this information form basis for the briefing. Other items to be discussed during briefing are electrical fittings, plumber work, sound, and so on that will be considered of the designer.” He also noted, “built environments that do not meet ideal standards are those built without consulting the professionals involved in its usage, and this lead to the built environment without toilets, nurses station, sluice room, major theater facility” He confirmed most healthcare built environment are built without adequate consultation as the government awards contract to contractors who may see the ideal process rigorous.-29-(Edo) The respondent have been nine years on his job as civil engineer, involved in erecting healthcare built environment. According to him “all erected structures are solely the design plan of the individual who awarded the contract for healthcare facilities, as such are built accordingly.” Furthermore, he stated that, “medical doctors to the best of my knowledge are the only professionals in the healthcare consulted to provide data on the facility type and items needed, which is used in building.” He also confirmed that nurses had not been consulted. He advised there should be a standard design for healthcare built environments. -30-(Bayelsa) This respondent is a male registered nurse with BNSC and MSN, within 40-45 years of age. He has been working as a nurse for seventeen (17) years, presently at a local government primary healthcare center. His response to the healthcare built environments in relation to nurses, states that “There is no treatment room, no nurses station, no cloak room, no staff toilet, no nurses’ common room.”-31-(Rivers) A female registered nurse and midwife with BNSC with a federal tertiary teaching hospital. She is within 40-45 years and eighteen (18) years on nursing job. When asked about the architectural structural design of the facility she works in relation to nursing, her response was “previously before COVID-19, in my unit, no toilet and no call/common room for nurses, one room for office and everything; another room for storage of supplies, no place to relax at least in this case where your patients are different and you are different, not like the general ward where you have to stay with your patients in the same room. With COVID-19 pandemic we moved, and here we have toilet for staff, but no call room for nurses, however construction is ongoing to make provision for call rooms for nurses and doctors. There was no initial plan for this provision until I requested for room for my nurse in charge, nurses room and room for potters. Cloak room is not going to be one as we have a male nurse. Nurses don’t have offices in the wards, but right inside the wards there is doctor’s call room fully furnished with a fridge, provision of bed sheets and cleaners to take care, and these are people who don’t always stay around and nurses who do not have a place to spend their break period. The doctors come along without the nurses, and when they finish making arrangements, they do “cut and nail” for the nurses. They kept nurses station by patient door in an isolation unit, as you are coming out with your PPE (personal protective equipment) from patients room you are already contaminating the nurses’ station. No toilet for nurses in the A & E unit (accident & emergency). Nurses use the same toilet with patients. You can imagine dragging toilet with patients.32-(Rivers) She has 19 years work experience as a registered nurse and midwife, specialized in intensive care with BNSC. Working with a federal teaching hospital, this respondent stated during the interview how 32 - bedded ward has only two toilets and two bathrooms, and there are a lot of structural faults, as no nurses’ toilet in most wards, they use the patients toilet in the side ward, only few wards have nurses toilet attached to their changing room. There are no built nurses’ stations, and tables are just kept in the corner of the wards and called nurses station. That is, however, not the case in the intensive-care unit, as there is nurses station, staff toilets, cloak room, common room, sluice room and treatment room and -33-(Rivers) in this interview, the respondent highlighted how staff and out patients use the same toilet facility in the corridor, but inpatients have their toilets in the wards. They have designated nurses’ station, treatment room, store, linen room, cloak room. A female registered nurse and midwife with BNSC, and MSN in view, 19 years on the job and in a multinational industrial and family clinic.-34-(Rivers) The respondent during her interview, said the matron takes charge of the nurses, patients, roster, store and supplies and consumables which are imported as it is a multi- national oil and gas industrial and family clinic; but not in charge of drugs. For built environment design as it relates to nurses, there are no specific built toilets for nurses as they use the general toilets provided for both out - patients and staff in the corridor. The facility has a cloak room, treatment room, and sluice room, nursery for much younger children, common room and nurses’ station. This interviewee is a registered nurse midwife with BNSC and has been on the job for 19 years.-35-(Rivers) this respondent is a practicing gynaecologist with a federal government healthcare institution. He also owns a private clinic. During the interview he pointed out he did not consult any nurse before building his clinic, as it was built based on what he has been seeing in private healthcare institutions.
3. Results
|
|
|
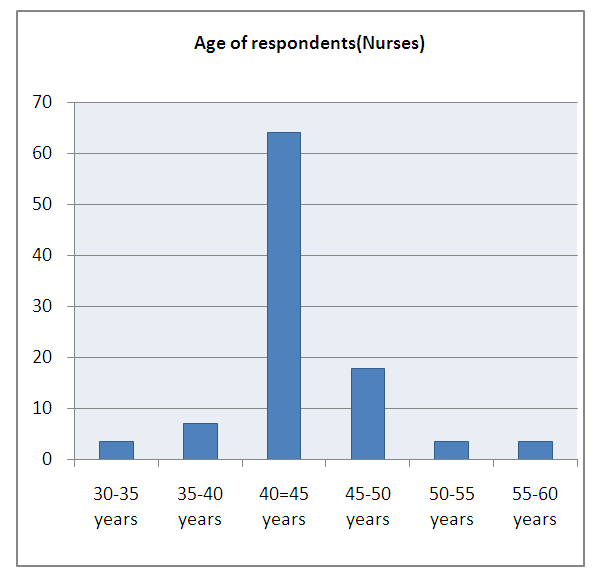 | Graph 1. Age of nurses participants |
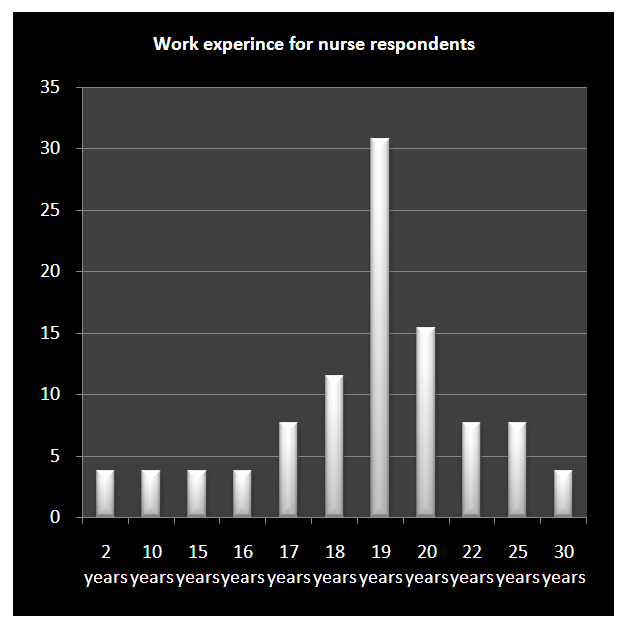 | Graph 2. Years of experience of nurse respondents |
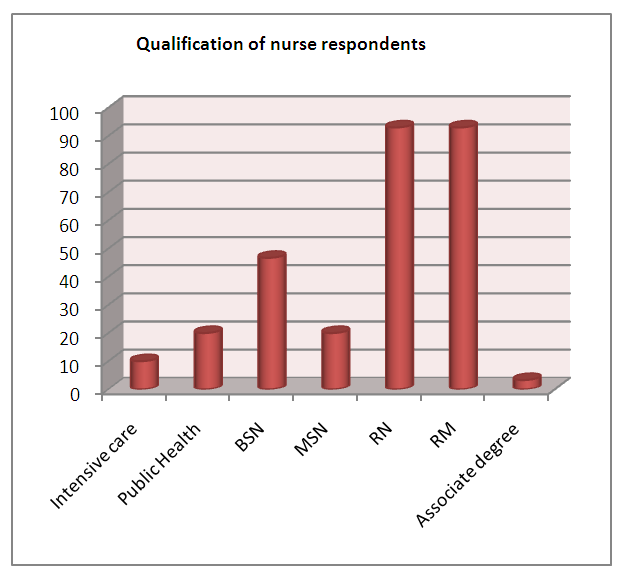 | Graph 3. Qualification of Nurses |
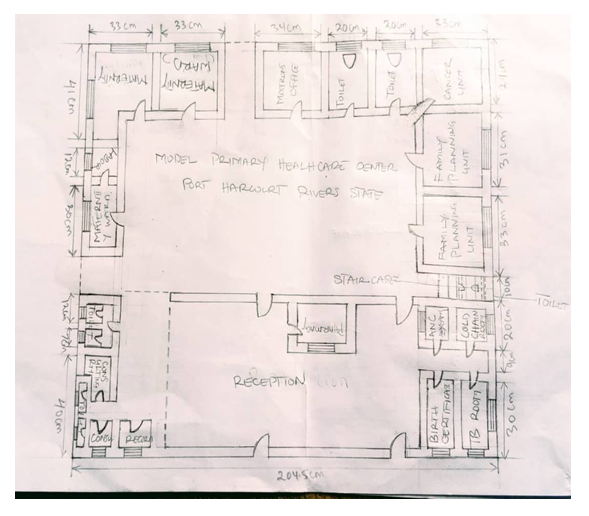 | Figure 1. Diagram plan for Model Primary Healthcare Center Port Harcourt Rivers State |
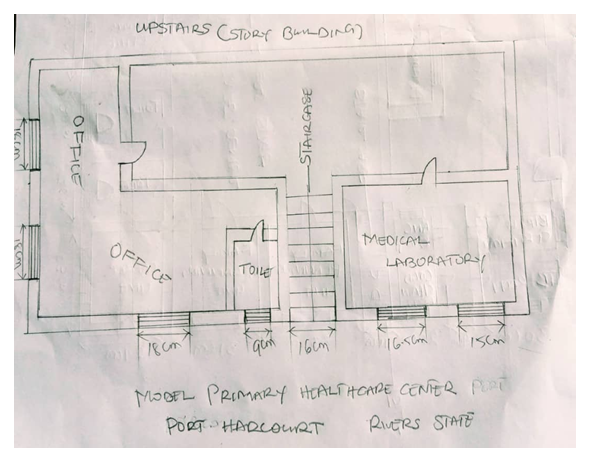 | Figure 1a. Diagram plan Model Primary Healthcare Center Port Harcourt Rivers State |
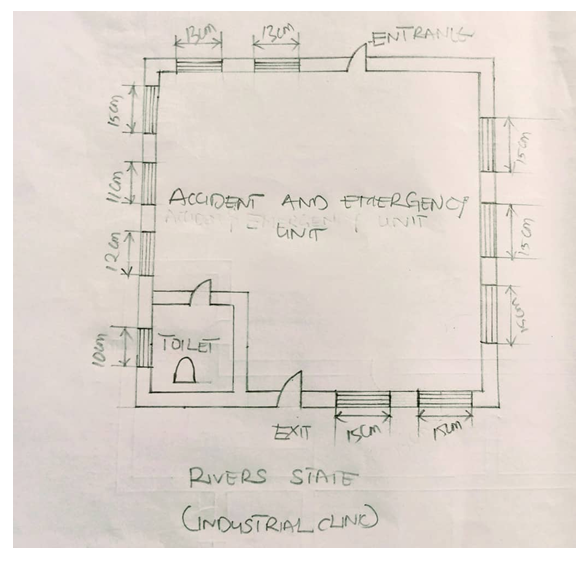 | Figure 2. Diagram plan for an industrial clinic Accident and Emergency unit Rivers state |
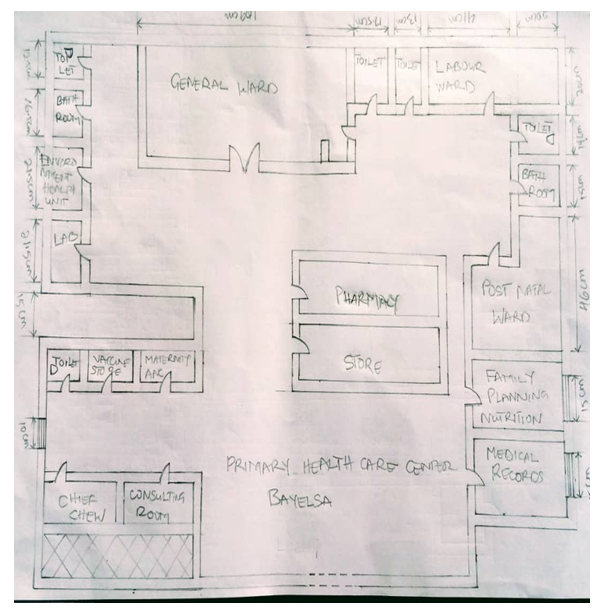 | Figure 3. Diagram plan for a Primary Healthcare center Bayelsa State |
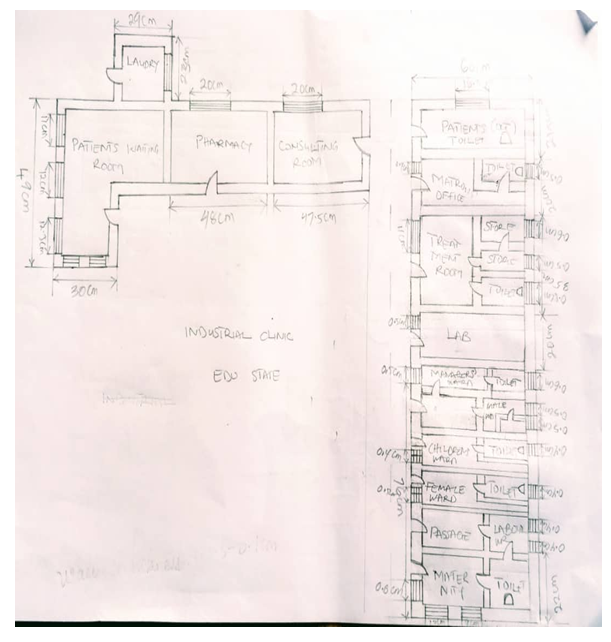 | Figure 4. Diagram plan for an Industrial clinic Edo State |
4. Discussion
- 46.7% of respondents have Bachelor of Nursing science (BNSC), while 20% have Master Science in Nursing (MSN) Nursing leadership and administration can be referred to as a number of managements, supervisory and executive title [16]; this is seen in the responses of respondents—3, 4, 7, 9, 11, 12, 13, 14,16, and 19 addressing the nurse leaders as: Nurse manager, in-charge, clinical manager, ward manager, deputy director, nursing department head, chief nursing officer (CNO), head of nurse and matron. The nurse administrators in this project function from Federal and state teaching hospitals, primary health centers, industrial clinics, staff and family clinics, private clinics and schools; which is in consonant with the statement of [17] that nursing administration can take many forms such as hospital, clinic, school, and other institutions.Respondent -4- lamented about the adverse effect of the deplorable healthcare built environment on the nurses in her unit and how it affects their job. The healthcare system should be a place of healing for everyone [29].[33] Disclosed that healthcare design projects are major organizational change to be ever experienced by healthcare and nursing executives in the course of their Career. Only one nurse administrator in this study (Respondent -18), and a clinical nurse (respondent 31) actually contributed and influenced the decision of the built environment. The nurse administrator spoke up for two healthcare structure building project that has already started and almost halfway, which was later brought to a halt for a period of six months before the observation and changes were effected. The clinical nurse demanded for ideal working space in an isolation ward and renovation commenced. Another Chief Nursing Officer was “carried along” in the ongoing renovation of staff quarters (Respondent 1). From respondent -22-. “The nurse administrators are not involved neither carried along in the healthcare facility structural design setting; hence, they don’t function in that capacity. This does not comply with [33] where it is stated, “Most recently, there have been several influences in the healthcare industry which have secured clinical nurses’ involvement in healthcare design. Clinical nurses, as well as nurse leaders, must be considered as interprofessional partners with designers in creating innovative design solutions that will improve workflow processes, efficiency and effectiveness of clinical practice, patient and provider safety, work environments for providers, and most importantly patient outcomes. Educational webinars including nursing students on exhibition on Health Facility Planning, Design & Construction; publication of a book –Nurses as Leaders in Healthcare Design and educating clinical nurses and other nurse leaders in the phases of the design process and opportunities to influence the design [32] are activities carried to create awareness and engage nurses. Nevertheless, there is still work to be done to ensure clinical nurses participation in the design of healthcare environments. This corresponds with the lecturer response(Respondent 25) “the curriculum in nursing leadership is shallow and does not contain such topics, however during the next examination meeting/workshop with the council, this topic will be discussed extensively.” Respondent 22, however, saw the need to create the awareness of this role in nurses through nurses’ forum. One of the reasons for lack of involvement in decision making in healthcare structural design could be delay in introducing the concept of the role of nurses in healthcare infrastructure design planning in the curriculum of nursing students. Thus the need for more studies as health care design teams are increasingly looking to health environments research to help inform design decision making. Jamie Morgan [32] in bringing nurses voice to healthcare design revealed nurses concerns on excessive walking distances, from the charting space, medication room supply rooms, and line of sight to patients and other caregivers. These concerns validated aided architectural decisions to increase patient visibility and visibility of peer nurses in inpatient unit designs.Response 27 and 29 respectively describe the outcome in response 31 which is the present state of most health facilities in Nigeria; “officially I did not consult any nurse for their input in the design.” and “medical doctors to the best of my knowledge are the professionals in the healthcare only consulted to provide data on the facility type and items needed, which is used in building. ”Response 29 explains the reason in response 31“, but right inside the wards there is doctor’s call room fully furnished with the fridge, provision of bed sheets and cleaners to take care, and these are people who don’t always stay around.” However [33] states that Clinical nurses are likely the most knowledgeable and experienced of all healthcare providers about the needs of patients, since they are in attendance and provide care for patients 24/7, all other healthcare professionals have short duration contact with patients for various therapies, treatments, diagnostic procedures, and medical consultations. However, this is not operational as clinical nurses or nurse administrators are not part of the built environment design. In the same vein Nurse leaders, must be considered as interprofessional partners with designers in creating innovative design solutions that improve workflow processes, efficiency and effectiveness of clinical practice, patient and provider safety, work environments for providers, and most importantly patient outcomes this is in agreement with response -28- The architects, engineers, and users of the built environment had to meet for briefing before the design plan; prior to the briefing, the professionals –hospital administrators, medical doctors, nurses pharmacist, laboratory scientist and others, are consulted through various means like observation and interviews and so on, to be conversant with the ideal facility needed and usage; this information form basis for the briefing. This project exponent the intricacies, that nurses have been putting up on their job all these years in their career. When nurses are unable to decide and speak up for their comfort and satisfaction, the possibility of speaking up for their patients will also be insignificant.
5. Limitation
- Lack of time to visit all facilities concerned in the study, in order to have first-hand information through observation study. Inability to meet up with busy schedules of some nurse administrators at the federal and state level for interviews.; Three out of the six states in the geo-political zone south-south Nigeria were used instead of six. The role of the nurse administrator in healthcare infrastructural design was narrowed to nursing department in this study. Architects, hospital administrators, the ministry of works, committee on built environments in healthcare were not part of the study. The interview was conducted by the researcher alone.
6. Conclusions
- Over the years the concept of evidence base in healthcare built environments has been underrated which is responsible for the present deplorable look of most healthcare facilities in southern Nigeria as 46.4% of the respondents not having specific built toilet, 21.4% sharing toilets with patients, 39.2% not having cloak room, and only 10.7% comfortable with their built healthcare environment and stated how it affected them positively. The ideal healthcare built environments is not merely a physical structure, but an environment of healing and care meeting all necessary conditions to ensure patients and staff safety, prevention of infection and promotion of staff satisfaction in the course of rendering quality healthcare service. Nurse leaders’ roles in healthcare services are quite elaborate and but inadequate compared to previous studies, where 42.9% manage and supervise nurses, 46.4% provide medical supplies and consumables, for decision making 10.7% and the role in healthcare built environment (3.6%). This study revealed nurses are not consulted and do not participate in healthcare built environment design planning in southern Nigeria, as only two out of 30 cross - section of nurses have influenced decision making in the healthcare built environment. Focusing on improving patient, environment, and workforce safety and quality has increased the need to create optimal physical environments. Research has also shown a strong link between the design of health care settings and outcomes experienced by patients, staff, and families. Hence the need to create the awareness and include nurse administrators and clinical nurses as frontlines in healthcare built environment design planning to influence decision in evidence based built environments of care.
ACKNOWLEDGEMENTS
- I appreciate all the nurses in the clinical, educational and administration; medical doctors, architect and civil engineer who responded to the interview, despite their schedule; I am grateful to my colleagues for their enthusiasm and motivation to complete this project which is timely.My gratitude goes to the Faculty Nursing sciences and student mentors of Texila American University (TAU) for their patience in the conclusion of this “Capstone Project.”The support and encouragement from my family and friends cannot be overemphasized. I will remain indebted to them.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML