-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2020; 10(2): 46-50
doi:10.5923/j.nursing.20201002.03
Received: Aug. 23, 2020; Accepted: Sep. 2, 2020; Published: Sep. 15, 2020

The Assessment of Nurses’ Knowledge and Barriers Regarding Non-Pharmacological Pain Management for High-Risk Neonates
Azza Mohamed Fathy Attia, Nabila Hassan Ali Abdella
Department of Pediatric Nursing, Faculty of Nursing, Port Said University, Egypt
Correspondence to: Azza Mohamed Fathy Attia, Department of Pediatric Nursing, Faculty of Nursing, Port Said University, Egypt.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Many barriers impact non-pharmacological pain management in the neonatal, such as lack of knowledge, protocol policy, work overload, professional and personal experience. The study aimed to investigate nurses' knowledge and barriers regarding non-pharmacological pain management for high- risk neonates. Design: A cross-sectional descriptive study was utilized with a sample of all nurses (40) in neonatal intensive care units(NICU) in Port Said hospitals.The data were collected using a questionnaire sheet. The results illustrated that about more than half of study nurses (62.5 %) had an unsatisfactory level of knowledge with statistically significant relation between training courses, have children and nurses' knowledge. Among the barriers found it the lack of training on neonatal pain, absence of pain protocols and record pain control measures, 75% of study nurses were a high workload, and 87.5 of them have insufficient time. The study recommended that periodic educational program for nurses working at NICU is mandatory, to rise and update the knowledge of nurses, care protocols for pain assessment and management should be incorporated and manual of critical care procedures.
Keywords: Non-pharmacological pain management, Neonates, Neonatal intensive care unite
Cite this paper: Azza Mohamed Fathy Attia, Nabila Hassan Ali Abdella, The Assessment of Nurses’ Knowledge and Barriers Regarding Non-Pharmacological Pain Management for High-Risk Neonates, International Journal of Nursing Science, Vol. 10 No. 2, 2020, pp. 46-50. doi: 10.5923/j.nursing.20201002.03.
Article Outline
1. Introduction
- Neonatal pain management is a challenging work to neonatal caregivers as when neonates had pain unable to talk or verbalize [1]. Thus, pain management is in the neonatal nurses' hands and is a vital issue in neonatal nursing [2]. Also, neonates are hospitalized in a comparatively hostile environment of the NICU, in which neonates undergo various tissue-damaging procedures as a part of clinical care, and each neonate may receive 50 - 120 medical procedures in 24 hours, which are painful [3].Optimal pain management needs effective assessment of pain, that can be difficult to be done in neonates due to absence of self-report [4]. As reported by international guidelines for pain management, the pain has been identified as the “fifth vital sign” that must be assessed in clinical practice [5]. The pain assessment instrument used must be multidimensional, involving assessments for physiologic and behavioral pain indicators [6].Neonatal care nurses had a vital role in pain management of neonates as they aimed to decrease the pain experience and increase the neonate’s ability to deal with and recover from the many NICU painful skills [7]. It is more challenging to avoid neonates painful skills. Thus, researches revealed that non-pharmacological ways are cost-effective, well-tolerated by neonates, help in treating mild to moderate pain, and these ways have proven effective with or without pharmacologic ways [7]. Non-pharmacological ways involve skin-to-skin contact, sweet solutions, non-nutritive suck with and without sweet solutions, position, swaddling, facilitated tuck, kangaroo care, human stimuli [8] & [7]. The nurses need to understand barriers that affect the effective pain management provision for neonates to decrease unnecessary pain suffering [9].Significance of the StudyLack of knowledge among nurses, towards neonatal pain suffering has been identified to be the main barriers in pain assessment [10]. To give competent and effective neonatal nursing care, nurses should assess pain and know that neonatal pain occurs, apply various pain management ways and know barriers and try to pass these to decrease the gap between the knowledge and skills [11].ObjectiveTo investigate nurses' knowledge and barriers regarding non-pharmacological pain management for high-risk neonates.
2. Subjects and Method
- Design and setting:A cross-sectional descriptive study was utilized in carrying out the study in neonatal intensive care units (NICU) at Port Said general hospitals (Elsalam, Port Fouad, ElNaser) and El-Tadamon health insurance). Sample: Convenience sample (40) of all the nurses working in these setting in NICU.Data collection tools:Data were gathered by a structured interviewing questionnaire which includes three parts as the following;Part 1: This part was concerned with the socio-demographic characteristics of the studied nurses as; age, education, marital status, having children, Years of experience in NICU, and number of courses attended about pain in neonates.Part 2: Assessed nurses' knowledge regarding non-pharmacological pain management for high-risk neonates in NICU. The questionnaire includes seven items (99 questions) with a total score of 99. The studied nurses' answers were compared with a model key, where (1) score was given for every point stated right and (0) was given for incorrect answer or "don did not know" level of knowledge satisfactory (≥60%) and unsatisfactory (<60%).Part 3: Measured the barriers that impact pain management in neonatal intensive care units. The nurse selects "yes" or" no"(The last question was the description of five barriers related to the pain management process of the high-risk neonates in the NICU, in order of priority.)Data collection procedureA letter of approval was sent to the directors of each study hospital, which included the aim of the study. Written consent was obtained from each of the nurses who participated in the study. The researchers clarified the aim of the study to each of the nurses who participated in the study. Nurses were interviewed separately, and the researcher filled the questionnaire sheet. The time that was spent in completing the questionnaire sheet was 25-35 minutes. The researchers, while collecting the data, provided health education for the nurses' weaknesses about non-pharmacological pain management. Collection of data was carried out for one month from the beginning of January 2019-to the beginning of febrile 2019. Ethical considerations:The study aims and expected outcomes were explained to the study sample, who be assured that all the data would be used for the research aim only. They were informed that the study was harmless and their agreement to participate is a prerequisite to be involved in the study.Data analysis: -The data obtained through the questionnaires were checked for accuracy and entered immediately into the computer using Statistical Package for the Social Sciences version 21 and Microsoft® Excel® software. Both descriptive and inferential statistical analysis was performed. Differences between proportions were tested using Chi-square test.
3. Result
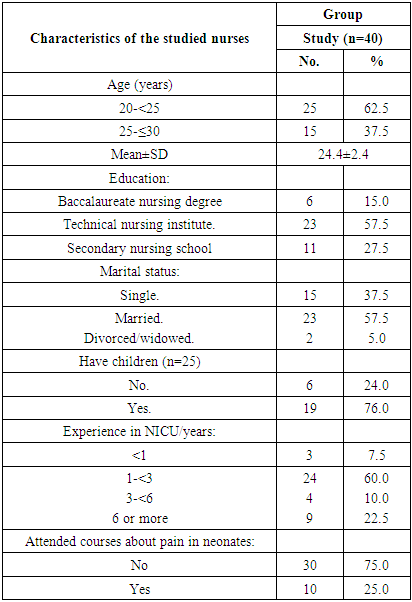
- Concerning the personal characteristics of the studied nurses, Table (1) demonstrates that more than two-thirds of the studied nurses were in age from 20-25 years old, more half of them had graduated from technical nursing institutes. The majority of the studied nurses don't attend training courses related to pain management in neonates, and more half of them had 1 to 3 years of work experience in NICU.
|
|
|
|
4. Discussion
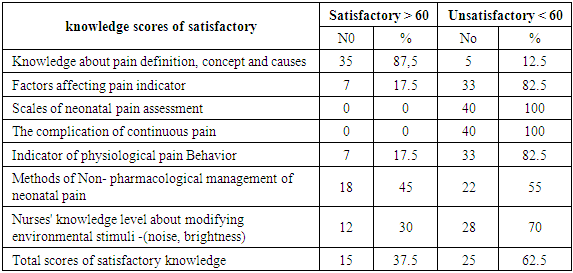
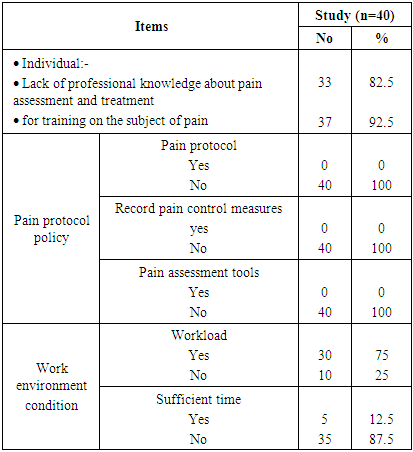
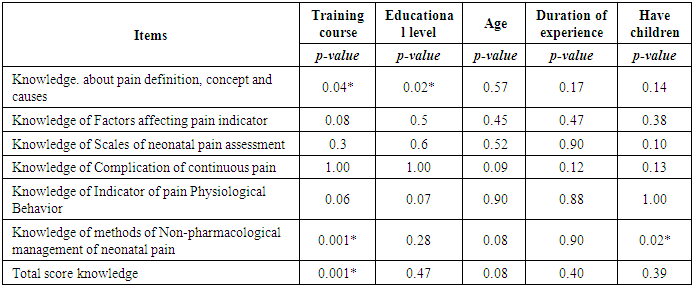
- Non –pharmacological approaches are often performed as the first step in neonatal pain management because it minimizes neonatal pain and stress while maximizing the newborn's own regulatory and copping abilities. Non -pharmacological strategies have no side-effects and can reduce acute pain from invasive or non-invasive procedures [12]. Concerning nurses' total knowledge regarding non- pharmacological management of pain for high- risk neonates, the present results indicated the majority of nurses had unsatisfactory scores regarding knowledge of non-pharmacological management of pain. This means lacks of necessary knowledge, which is basic for intervention skills in order to be able to provide and promote high- quality care for high- risk neonates. This lack of knowledge may be related to lack of training programs about non-pharmacological management of pain which did not happen among more than two- thirds of nurses in this study. These results are in agreement with Al Qadir & Al khalaileh [13] in Jordan and Mehrnoush. et al. [14] in Iran stated the participants in their studies haven't information about non-pharmacological ways to decrease pain in the neonates., On the other hand, these results did not agree with Aymar et al., [15] in Brazil also found that most health care professionals knew the management protocols for neonatal pain.Non- pharmacological methods provide improved growth outcomes, shorter durations of mechanical ventilation and oxygen supplementation. Also, it decreased length of stay and cost of hospitalization in addition to enhanced neurodevelopmental outcomes [16]. The findings of the present study indicated that slightly less than half of the studied nurses knew the benefits of non-pharmacological management of pain in high-risk neonates. In the same respect, Hall & Anand [12] stated that the non-pharmacological methods were the first steps to be undertaken in high-risk neonatal pain management because they minimized pain and stress while maximizing the newborn's own regulatory and coping abilities; also, it does not cause side-effect and reduced acute pain from invasive or non-invasive or non-invasive procedures. On the other hand, these findings were inconsistent with those of Wu., [17] in China, where they stated that the non-pharmacological intervention could not ease or relieve pain.A statistically significant association was detected in the present study between staff nurses' knowledge and their marital status and their attendance in training programs. Thus, married nurses and those who had attended training programs had adequate knowledge about non- pharmacological management of neonatal pain; this might be attributable to the fact that married nurses had additional knowledge from their experience as mothers. This finding is in the same way with the Iranian study of Mehrnoush et al., [14] that mentioned that appropriate pain management was significantly correlated with sufficient training.Recent studies showed high sound pressure levels in the NICUs and in the incubators and have shown the neonates harmful health effects [18]. So, the study centred on that issue related to the nurses’ knowledge regarding modification of environmental stimuli like controlling environmental noise and light at NICU the majority of the study nurses had unsatisfactory knowledge. These results are in the same line with the Egyptian study of El-Ziady et al., [19] that revealed the same finding. The investigator mentioned that the training program is vital to improve the nurses' knowledge level that effectively decreases NICU noise and light.Consistent with the previous findings, the effective pain management barriers were identified as high workload, personnel shortage, knowledge lack, pain management protocols absence, time lack, and lack of trust in the pain assessment instruments [20]. According to pain protocol policy, the present study indicated that there are no pain protocol, pain assessment tools and record pain control measures resulting. Also, none of the studied nurses in the present study has adequate knowledge regarding both the scales of pain assessment and the use of pain assessment. evidence-based pain management guidelines in the NICU absence has also been reported in the previous studies [1]., [21]. In a study in the United States and China, less than half of the study sample reported that pain management guidelines or protocols were evidence-based [22].There is no record pain control measures also appeared as a barrier in this present study. The record is part of the health information system, enables the ethical and legal support of the assistance, works as auditing and development instrument of the teaching and research in the nursing area [23]. Also, the findings revealed that organizational factors play a crucial role in the health care services development for the neonates, involving pain management. It is necessary to provide the needed training for all the personnel working with neonates.
5. Conclusions
- Based on the results of the present study, there was a statistically significant relationship between lack of nurses’ knowledge and training courses they took and the children they have. Among the barriers that the nurses faced; the lack of training on neonatal pain, absence of pain protocols, lack of time, and a high workload.
6. Recommendations
- Periodic educational program for nurses working at NICU is mandatory, to rise and update their knowledge. Moreover, care protocols for pain assessment and management should be incorporated, and manual of critical care procedures for the newborn should be offered to all nurses in NICU. In the same vein, written policies of neonatal pain should be content part of care the neonatal pain management in all NICU.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML