-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2020; 10(1): 1-11
doi:10.5923/j.nursing.20201001.01

Effect of Supportive Nursing Instructions for Maternity Nurses Regarding Electronic Fetal Monitoring
Amira Refaat Said, Hanan Amin Ali
Obstetrics & Woman’s Health Nursing, Faculty of Nursing, Benha University, Egypt
Correspondence to: Amira Refaat Said, Obstetrics & Woman’s Health Nursing, Faculty of Nursing, Benha University, Egypt.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Electronic Fetal Monitoring is one of the most commonly used obstetrical practices in the evaluation of fetal well-being. Nurses have important responsibilities on application and interpretation of electronic fetal monitoring. The aim of the study was to evaluate supportive nursing instructions for maternity nurses regarding electronic fetal monitoring. Quasi experimental study design was used. The study was conducted in the Obstetrics Department at Benha University Hospital. A convenient sample of all nurses working in Obstetrics emergencies department at Benha University Hospital (70 nurse). Two tools were used for data collection; I) A self-administered questionnaire: include three parts; Part 1: Socio demographic characteristics of the studied nurses. Part 2: Obstacles that affect achieving of nursing care for the use of electronic fetal monitoring. Part 3: Assessment of nurses’ knowledge regarding electronic fetal monitoring. II) Observational checklist for performanceofnursing practices regarding electronic fetal monitoring in the obstetrics unit. The study results showed that 85.7% of nurses had poor knowledge before application of the supportive nursing instructions. However, 60% of them had good knowledge after application of the supportive nursing instructions respectively. As well as, 75.7% of them had unsatisfactory practices toward nursing care during electronic fetal monitoring before application of the supportive nursing instructions. Meanwhile, after application 82.9% had highly satisfactory practices respectively. The study concluded that supportive nursing instructions have appositive effect on nurse’s knowledge and practices regarding electronic fetal monitoring. There was a highly statistically significant difference before / after supportive nursing instructions of the studied nurses’ knowledge and practice regarding electronic fetal monitoring (P ≤ 0.001). The study recommended that continuous refreshment courses and follows up programs for nurses regarding electronic fetal monitoring.
Keywords: Electronic fetal monitoring, Nursing instructions, Maternity nurses
Cite this paper: Amira Refaat Said, Hanan Amin Ali, Effect of Supportive Nursing Instructions for Maternity Nurses Regarding Electronic Fetal Monitoring, International Journal of Nursing Science, Vol. 10 No. 1, 2020, pp. 1-11. doi: 10.5923/j.nursing.20201001.01.
Article Outline
1. Introduction
- Electronic fetal monitoring is a method of assessing fetal status both before and during labor. The fetal heart rate base line are obtained and evaluated to identify any abnormalities that can impact fetal wellbeing. [1]. This kind of fetal monitoring is an electronic method of continuously assessing the fetal heart rate and obtaining information about the laboring woman’s uterine activity, this information is recorded on graph paper, allows on ongoing minute to minute assessment of fetal well-being during labor and provides a permanent record for the medical chart [2].The primary objective of electronic fetal monitoring is to provide information about fetal oxygenation and prevent fatal injury that could result from impaired fetal oxygenation. Electronic fetal monitoring provides a continuous record the instantaneous fetal heart rate and uterine contractions; patterns are of clinical significance, use in low and high-risk patients [3]. It is used periodically throughout the labor process based on the maternal and fetal status. Observing fetal heart rate on monitor is easier than listening with stethoscope or fetoscope [4].There are two methods of electronic fetal monitoring; external fetal monitoring is also called indirect fetal monitoring or noninvasive fetal monitoring. Aultrasonic transducer to monitor the FHR. While the contraction pattern is monitored with atocdynamometer both are applied to the laboring woman’s abdomen, internal fetal monitoring is direct FM, Invasive fetal monitoring. Fetal heart rate is monitored by the use of a hook electrode which is applied directly to the presenting part of the fetus. Contraction Pattern is monitored by the use fluid field C which is inserted below the presenting part directly into the uterine cavity through the cervix. Internal monitoring provides a more accurate and consistent transmission of the fetal heart rate than external monitoring because factors such as movement do not affect it. Internal monitoring may be used when external monitoring of the fetal heart rate is inadequate, or closer surveillance is needed [5]. It is responsibility of the nurse to assess FHR patterns, perform independent nursing interventions, and report non-reassuring patterns to the physician or nurse, the emotional, informational, and comfort needs of the woman and her family must be addressed when the mother and her fetus are being monitored [6]. The nurse explain the procedure to mother and labor support partner how the electronic monitor (internal or external) works in assessing, detecting fetal heart rate and assessing quality of uterine contractions to remove fear of unknown and ensure that mother can work with the monitor, when applying the monitor, explain to the mother what is being done, discuss with mother fetal conditions and increased the sound of fetal heart to allow the mother to hear the FHR beats to gain her confidence and trust and notes F H R baseline, variability and presence of accelerations or decelerations in F H R pattern [7]. More over the nurse must carefully follow guidelines and checklist for application and initiation of monitoring to provide dislodgement of the trunsedoser instruct mother not to move, document monitor strip and observation such as maternal vital signs, maternal position/repositioning, vaginal examinations & findings, medications; anesthesia/analgesia, voiding; emesis, fetal movement, baseline FHR, pushing and bearing down [8]. The nurse must adjust during fetal heart rate monitoring in relocation of transducers, flushing or adjustment of catheter, replacement of catheter and time lapsed while changing monitor strip paper [9].The nurse plays an important role in emergency measures during fetal heart rate monitoring which include reposition patient in lateral position to increase uteroplacental perfusion or relieve cord compression. Administer oxygen at 10 to 12 L/min or per hospital protocol via face mask. Discontinue oxytocin if infusing. Correct maternal hypovolemia by increasing IV as ordered. Assess FHR pattern change, such as maternal hypotension. Notify physician of the finding observed [10].
1.1. Significance of the Study
- Lack of knowledge can increase the anxiety levels of both the woman and her support nurse. Birthing room nurses have responsibilities for recognizing and interrupting fetal monitoring patterns, notifying the physician and certified nurse of problems and initiating corrective and supportive measures when needed [11].Trusting relationship also makes it easier for the client to follow Instructions and better participate in the labor process. When the client and her support persons feel the nurse is aware and respectful of their level of knowledge and any cultural or religious consideration, they are more likely to cooperate and actively participate in the plan of care [12], supportive nursing instructions was applied for maternity nurses to update and upgrade their knowledge, practices and to be reference guide whenever needed, also, it should be utilized and integrated through instructional modalities, therefore this study was conducted.
1.2. Aim of the Study
- This study was aimed to evaluate effect of supportive nursing instructions for maternity nurses regarding electronic fetal monitoring, this aim was achieved through- Assessing nurses' knowledge, and practices about electronic fetal monitoring.- Designing and developing supportive nursing instructions about electronic fetal monitoring. - Implementing supportive nursing instructions for nurses regarding electronic fetal monitoring. - Evaluate the effect of supportive nursing instructions on nurses' knowledge and practices about electronic fetal monitoring.
1.3. Research hypotheses
- In order to fulfill the purposes of the research, the following Hypotheses were formulated1- The majority of nurses have a lack of knowledge and practices about electronic fetal monitoring, before application of supportive nursing instructions.2- Supportive nursing instructions have appositive effect on nurse’s knowledge and practices regarding electronic fetal monitoring.
2. Subjects and Methods
2.1. Research Design
- Quasi experimental design was used for conducting the study.
2.2. Research Setting
- The study was conducted in Obstetrics Department at Benha University Hospital.
2.3. Subjects
2.3.1. Subject Type
- A convenient sample of a total nurse’s works in Obstetrics department at Benha University Hospital was recruited for the study (70 nurses).
2.3.2. Subject Size
- All nurses who worked at previous mentioned setting. Size of the sample was completed during 6 months /three days per week.
2.4. Tools of Data Collection
- Two tools were utilized for data collection, prepared by the researchers after reviewing related literature and tested by a panel of experts for validity.
2.4.1. First Tool
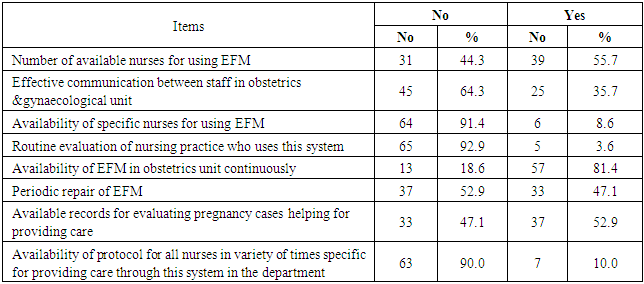
- Self-administered questionnaire sheet: include three parts; Part 1: Socio demographic characteristics of the study nurses: included (Age, educational level, years of experience, previous training courses, and duration of courses). Part 2: obstacles that affect of using electronic fetal monitoring such as (number of available nurses for using EFM, effective communication between staff in obstetrics &gynecological unit, availability of specific nurses for using EFM, routine evaluation of nursing practice who uses this system, availability of EFM in obstetrics unit continuously, Periodic repair of EFM, available records for evaluating pregnancy cases helping for providing care and availability of protocol for all nurses for providing care through system of EFM in the Obstetrics department. Part 3: Assessment of nurses’ knowledge regarding electronic fetal monitoring such as (meaning of EFM, indications of performance EFM, methods of using EFM, connections to monitor the rate of fetal pulse and following the contractions and contractions of the uterus, nursing care should be performed for the pregnant woman who uses the electronic fetal monitor, the expected explanations as to their priority to observe the fetus, nursing procedures of their priority when there are disturbances and abnormalities in the fetal pulse rate and the risks of using the device).Scoring system: The questions were scored as the following; score (1) was given for the correct answer and (0) for the incorrect answer before and after application of the guideline. The scores of total knowledge was considered as more than 60% was adequate and less than 60% was in adequate.
2.4.2. Second Tool
- Observational checklist: it was adapted from the (Royal College of obstetricians and Gynaecologists guidelines, 2018) guidelines present recognized methods and techniques for clinical practice, based on published evidence for nursing practices management regarding electronic fetal monitoring which included Prepare the equipment, explain procedure for women, and offer the opportunity to ask any questions, recording complete mother identification at beginning of the monitor strip, Performing Leopold’s maneuvers to determine fetal position &locate fetal back, undress to put a wide elastic belt around her back to secure the transducer in place, putting mother in comfortable position, washing hands and drying it well to prevent cross infection, assessing fetal heart tone, Placing monitor belts under the mother back, Confirming the presence of fetal heart tone with feto-scope before applying fetal monitor, Connecting the ultrasound transducer and the toco-transducer to the fetal monitor, Placing the toco-transducer on the fundus of the uterus so that the pressure sensitive button is flush against the maternal abdomen, Placing the ultrasound transducer on the maternal abdomen over the fetal back, Evaluation the FHR strip, Removing electronic fetal monitor, Cleaning mother’s abdomen from gel and Washing hand). Scoring system: The checklist items were scored (2) for done each step correctly while (1) score was given for done incomplete correctly and (zero) score for not done. The scores of total practice were considered as ≥ 80% was highly satisfactory and ≤ 80% was unsatisfactory.
2.5. Methods
- The study was executed according to the following steps
2.5.1. Approvals
- This research was conducted under the approval of the Faculty of Nursing Ethical Committee, Benha University. An official permission was obtained from the directors of the pre-mentioned setting to conduct the research after explaining its purpose.
2.5.2. Tools Validity and Reliability
- The developed tool was reviewed for appropriateness of items and measuring the concepts through five an expert jury panel in the field of maternity nursing and obstetric medicine specialty to assure content validity. The questionnaires were modified according to the panel judgment on clarity of sentences and appropriateness of content (The reliability was done by Cronbach's Alpha coefficient test equal 0.87).
2.5.3. Ethical Considerations
- All ethical issues were assured, participants were given explanations about the purpose of the study, and they were also informed that they could withdraw from the study at any time before the completion of the study. Participants who agreed to complete in this study were asked to sign a consent form. Confidentiality of participants‟ information was assured and the data were accessed only by the researchers involved in this study.
2.5.4. The Pilot Study
- The pilot study was conducted on (7) nurses (10% of 70 nurses) to test the clarity and the applicability of the tool, find out the possible obstacles and problems that might face the researchers and interfere with data collection. The study sample included in the pilot study was included also into the study due to no modification done in the tool.
2.5.5. Field Work
- Incorporate the following phases as following- Assessment phase:Nurses were assessed for their needs prior implementation of the supportive nursing instructions regarding electronic fetal monitoring.- Planning phase:The content of the supportive nursing instructions related to electronic fetal monitoring was designed to meet the following objectives: § General objective: At the end of supportive nursing instructions sessions each nurse should be able to acquire essential knowledge and skills needed to provide competent care to women during electronic fetal monitoring.§ Specific objectives: At the end of guideline sessions each nurse should be able to: 1. Define the concept of electronic fetal monitoring.2. Enumerate indications of electronic fetal monitoring.3. Recognize how to use this device.4. Determine the connections number to follow the fetal heart rate and follow the contractions of the uterus.5. Discuss the nursing care performed for pregnant women who use an electronic fetal monitor.6. Explain the expected interpretations based on their priority for electronic fetal monitor.7. Enumerate nursing procedures according to their priority in the event of disturbances and abnormalities in the fetal heart rate.8. discuss the risks of using this device.- Implementation phase: The supportive nursing instructions for maternity nurses were carried out in Obstetrics Department at Benha University Hospital. Based on the results obtained from pre training assessment using the interviewing questionnaire and observation checklists, teaching and training were constructed to satisfy the studied nurses’ deficit knowledge and practices regarding electronic fetal monitoring. Implementation of teaching and training took (12) weeks period and were implemented for a group of (7) nurses according to working circumstances. The researcher visited the setting three days per week. The overall sessions were 8 sessions were devoted to (3 theory and 5 practical), nurses were divided into 10 groups and the content was implemented for each group separately. The duration of each theory session was ranged from 20-30 minutes while practical session was ranged from 30-60 minutes including periods of discussion according to their achievement, progress and feedback. The researchers went to the unit two days per week from 9.00 A.M to 1.00 P.M for six months starting from the beginning of June 2019 till end of November 2019. At the beginning of first session an orientation to the instructions, general and specific objectives were explained. Arabic languish was used to suit all level of education. Different methods of teaching and training strategies were used such as lecture, group discussion, demonstration and re-demonstration for clinical procedures Instructional media included, handout prepared by the researcher and distributed to all nurses in the first day of the training. After each session feedback was done. Most nurses were cooperating and interested by this topic. - Evaluation phase: After completion of the supportive nursing instructions sessions the questionnaire format and observation sheet were filled again to evaluate effectiveness of the supportive nursing instructions with the same pretest questionnaire.
2.5.6. Statistical Analysis
- Data was collected, presented in tabular form. Percentages were calculated for qualitative data and x2 for test of significance, mean and standard deviations were calculated for quantitative data using the Statistical Package for Social Sciences (SPSS version 24) for statistical analysis.
3. Results
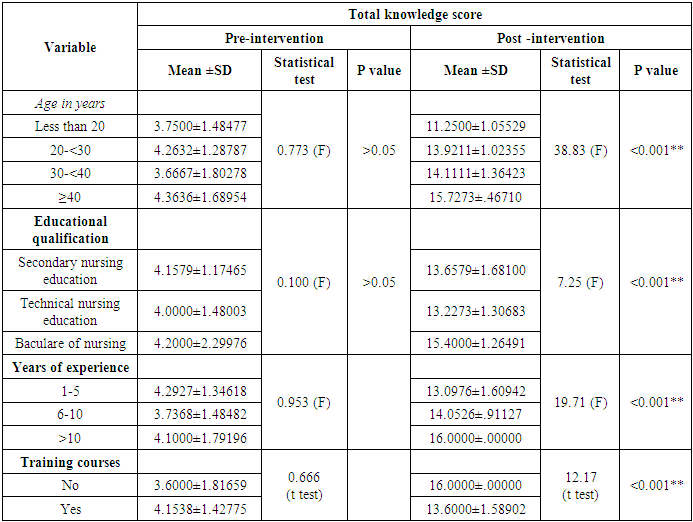
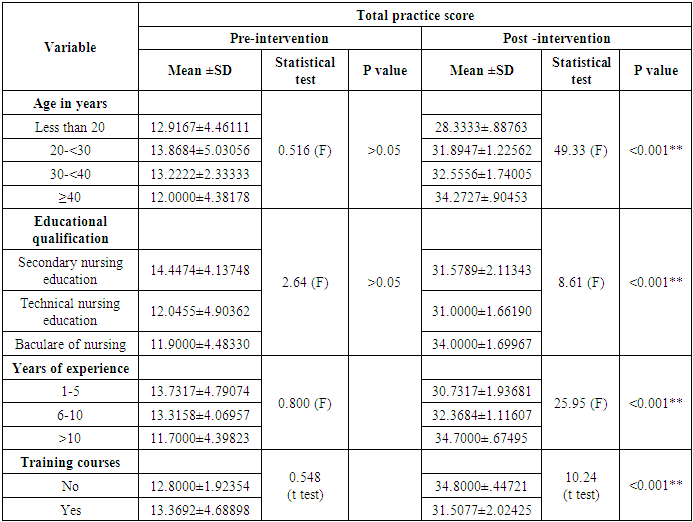
- Table (1) shows that, 54.3% of studied sample were from 20 to 30 years, the mean age was 27.75 ± 8.05. Regarding educational qualification, more than half of them 54.3% had secondary school diploma and 14.3% had bachelor degree. As regards years of experience, more than half of them 58.6% had from one to five years of experience, while 14.3% had more than 10 years of experience, the mean years of experience 5.77±3.624. The majority of the studied nurses 92.9% did not receive any training program regarding electronic fetal monitoring in the department.
|
|
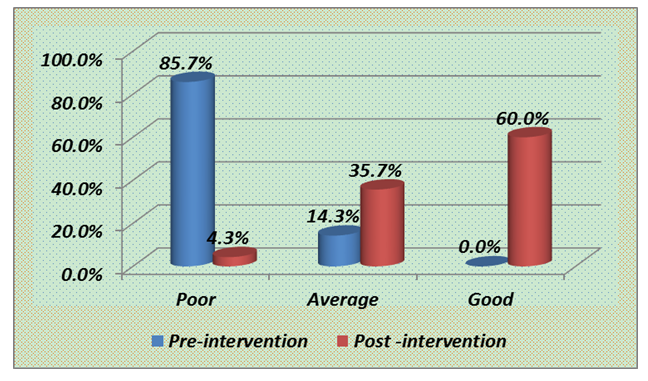 | Figure (1). Distribution of studied nurses’ total knowledge score regarding fetal monitoring pre and post intervention |
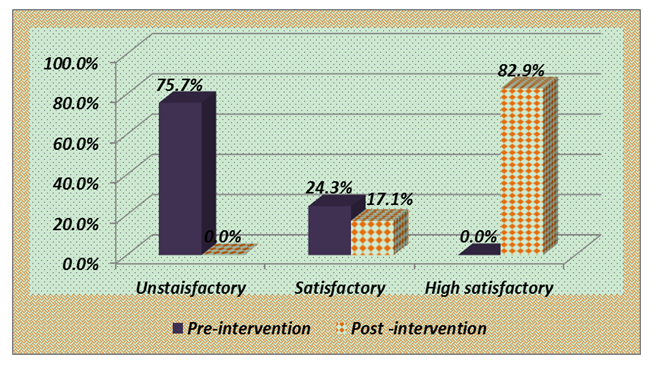 | Figure (2). Distribution of studied nurses’ total practice score regarding fetal monitoring pre and post intervention |
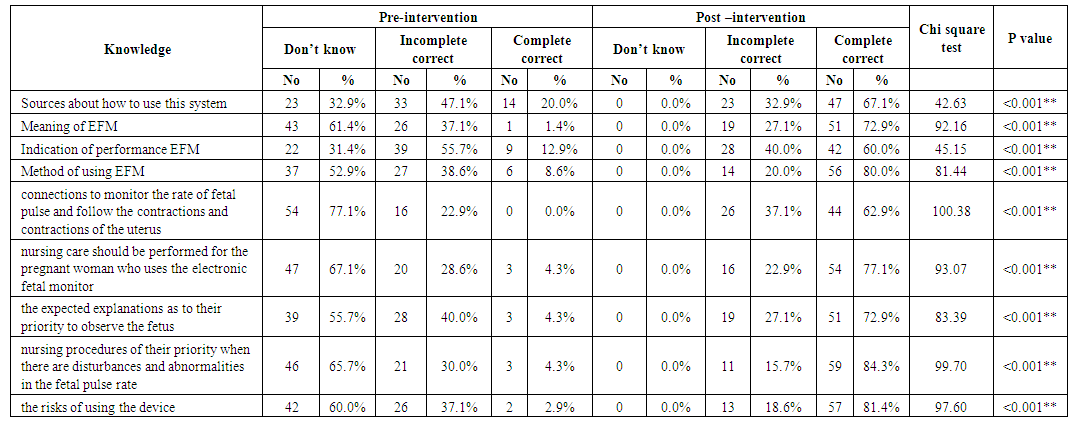 | Table (3). Distribution of studied nurses’ knowledge regarding fetal monitoring pre and post intervention (n=70) |
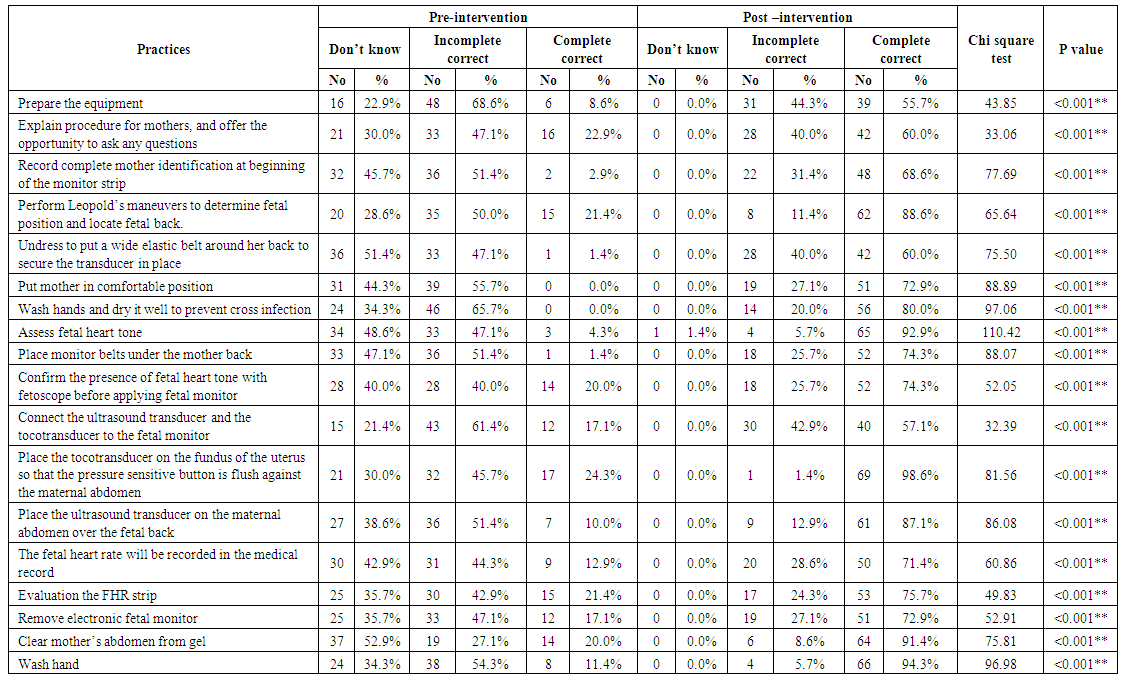 | Table (4). Distribution of studied nurses’ practice regarding fetal monitoring at different phases of intervention (n=70) |
|
|
|
4. Discussion
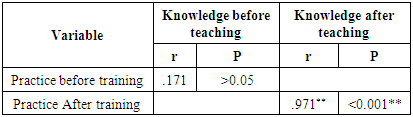
- The nurse plays an important role in providing information about fetal monitoring methods, its effectiveness in low risk women and about its advantages and limitations. It is the responsibility of each nurse to assess FHR patterns, implement independent nursing interventions, and report non reassuring patterns to the physician regularly assess and record results of electronic EFM (FHR and variability, decelerations, accelerations, uterine activity contractions, uterine resting tone) to provide consistent and timely evaluation of fetal well-being and progress of labor. Auscultate FHR and palpate contractions on a regular basis to provide a cross-check on the EFM output and ensure fetal well-being. Pregnant women should be informed about the equipment and procedures used and the risks, benefits, and limitations of intermittent auscultation [13].This research was aimed to study effect of the nursing supportive instructions on nurses regarding electronic fetal monitoring, this aim was achieved through assessing nurses' knowledge, and practices about electronic fetal monitoring, Designing and developing guideline instructions about electronic fetal monitoring, implementing guideline instructions for nurses regarding electronic fetal monitoring and evaluate the effect of guideline instructions on nurses' knowledge and practices about electronic fetal monitoring. Regarding personnel characteristics’ of the studied nurses, the study showed that, half of studied sample were from 20 to 30 years, Regarding educational qualification, more than half of them had secondary school diploma. As regards years of experience, more than half of them had from one to five years of experience. The majority of the studied nurses did not receive any training program regarding electronic fetal monitoring in the department. This result may be due to absence of educational program regarding EFM in the unit. Also, this lack of knowledge may be related to the level of education and could be interpreted that nearly most of the studied nurses were diploma nursing graduate that were graduated since long period of time that might led them to lose too much of their basic graduation knowledge and skills, as well as absence of training programs related to EFM. Regarding obstacles affecting the provision of providing care for fetal monitoring as reported by the studied nurses the majority of nurses reported that there are no effective communication between staff in labor unit, no specific nurses for using EFM, no routine evaluation of nursing practices who uses this system, there are no available protocol for all nurses in variety of times specific for providing care through this system in the department and no periodic repair of EFM.Regarding nurses' knowledge about EFM in obstetrics department, results of the present study revealed that there was most of the nurses included in the study had incorrect knowledge before intervention of nursing instructions. This result may be due to absence of educational program regarding EFM in the unit. Also, this lack of knowledge may be related to the level of education and could be interpreted that nearly most of the studied nurses were diploma nursing graduate that were graduated since long period of time that might led them to lose too much of their basic graduation knowledge and skills, as well as absence of training programs related to EFM. The results of the present study revealed that there was significant improvement of nurses’ knowledge after instructional guideline application compared to before it. These finding was agreement with ramadan., etal 2018 [14], who studied maternity nurses’ performance regarding Non-invasive Fetal Wellbeing Measures and showed that, significant difference in the level of knowledge and interpretation of maternity nurses about cardio-tocography <0.001. Also Pehrson etal. (2011) [15] who studied evaluation and impact of cardio tocography training interventions: a systematic review and found that training can improve knowledge of cardiotocography (CTG) leading to better quality care team training courses.This result is contradicted with Bayley et al, [2013] [16]. Who studied Knowledge and perceptions of quality of obstetric and newborn care of local health providers, concluded that training had little impact on levels of knowledge and the gap of knowledge couldn't be overcome by simply providing more training, so most of staff reported perception of poor quality of care. The present study revealed that that more than three quarter of studied nurses have unsatisfactory practice before supportive nursing instructions, this unsatisfactory level of practice showed the importance of continuous education, protocols and regular updating clinical courses for nurses to promote knowledge and practice. Therefore, it is important and essential that nurses are well trained and educated on EFM nursing care have the vital role to play to inform the maternity nurse and begin the initial assessment and management of such cases. The present study revealed that highly statistically significant difference before and after training instructions during fetal monitoring procedures. This may be due to the educational program was effective in raising staff nurse awareness, increasing motivation to further expand their skills and also has a great effect because continuing education plays a significant role in preparing nurses to deal with the major changes currently making an impact on health care.These results are supported by Islam et al., [2015] [17]. Who studied Perceptions of health care providers and patients on quality of care in maternal and neonatal health in fourteen Bangladesh government healthcare facilities, found that the majority of nursing personnel mentioned that training could be a good initiative for an improved quality of care and indicated that in-service training needs to be organized regularly to enhance the quality of health care. Also, this result agreed with Bradley et al., [2015] [18]. Who studied the impact on obstetric care providers and on quality of care in Malawi and found that inadequate obstetric skills and undermining performance and professionalism were from factors that effect on the practices of maternity nurses.Results of the present study revealed that there was highly statistically significant difference between studied nurses total knowledge score, and their personnel characteristics before and after intervention, these results is disagree with Sangeetha C. (2012) [19] who studied assessment of knowledge, attitude and practice regarding Cardiotocography among staff. Who found that there is a significant relationship between knowledge on interpretation of CTG and respondents age, educational level and work experienc.Also, results of the present study revealed that there was a highly statistically significant difference between studied nurses total practices score, and their personnel characteristics pre and post training, these results agrees with Devane, etal 2017 [20] who studied Cardiotocography versus intermittent auscultation of fetal heart on admission to labour ward for assessment of fetal wellbeing and found that there was highly statistically significant relation between nurses’ performance & their age.Regarding correlation between the total scores of maternity nurses’ knowledge & practices before & after nursing supportive instructions. There was statistically significant correlation between knowledge after teaching and practice after training. These finding is agreed with Sowmya etal., 2013 [21] who studied effectiveness Of Cardiotocography Training intervention on knowledge and skill among nurses working in maternity units and concluded that Cardiotocography Training Intervention (CTP) improved the level of knowledge and skills among nurses after program. Therefore, it is important and essential that nurses are well trained and educated how to cope with EFM system in the obstetrics department as they have the vital role to play to inform the doctor and begin the initial assessment and management of such cases. This could be attributed to the fact that any training course increase nurses knowledge in turn changes their practice.Generally, this research pointed out that, after instructional guidelines, there was improvement in the most aspects of knowledge and practices, this partially supported the research hypothesis, and it revealed the areas of weakness of nursing practices. Moreover, it is hoped to establish in-services training programs, standards of care and follow up for continuing improving knowledge and practices regarding EFM.
5. Conclusions
- The present study shade lights on electronic fetal monitoring. Before applying the program, majority of studied sample had poor knowledge and practices about electronic fetal monitoring while after implementation of program applied guideline instructions succeeded to a great extent in improving nurses 'knowledge and practices regarding electronic fetal monitoring. Supportive nursing instructions have appositive effect on nurse’s knowledge and practices regarding EFM.There was a significant improvement in the nurses ‘knowledge and practices regarding EFM after supportive nursing instructions compared with that before it. There was positive correlation between nurses’ knowledge and their practices before and after instructions in relation to their age and years of experience and positive significant correlation between nurses’ knowledge and practices after instructions. Aforementioned findings are mainly supported the study hypothesis.
6. Recommendations
- In the light of the findings of current study the following recommendations were be suggested:a. Supportive nursing instructions regarding EFM nursing care must be available at the Obstetrics Department.b. Developing periodical training and teaching programs regarding EFM nursing care.c. Continuous refreshment courses and follows up programs.d. Replication of the study on large sample size and in different hospitals to evaluate knowledge and practices of nurses in relation to EFM nursing care for generalizing the findings.
ACKNOWLEDGEMENTS
- The authors would like to thank all Nurses who willingly participated in this study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML