Methu C. W. 1, Mwenda C. M. 2, Mbugua R. G. 3
1School of Nursing, Mount Kenya University, Thika, Kenya
2Department of Medical Surgical Nursing, School of Nursing, Mount Kenya University, Thika, Kenya
3Department of Community Health Nursing, School of Nursing, Mount Kenya University, Thika, Kenya
Correspondence to: Methu C. W. , School of Nursing, Mount Kenya University, Thika, Kenya.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Urinary tract infections are the most frequently occurring health-care associated infections. 75% of these infections are linked with utilization of an indwelling urinary catheter. However, 40% of urinary tract infections are preventable. The researcher sought to assess nurse related factors influencing compliance with Centre for Disease Control (CDC) guidelines for CAUTI prevention among nurses working at Embu level 5 hospital. The study was carried out in 2017. Methods: A descriptive cross-sectional study was conducted among nurses working at Embu level 5 hospital between 107 participants were selected using systematic random sampling. Data collection tools included a self-administered structured questionnaire, and an interview schedule for key informants and an observation checklist. Data analysis was done using SPSS version 21 and thematic analysis. Findings: Compliance among the nurses was found to be low (46.7%). However, most respondents had adequate knowledge of the guidelines on CAUTI prevention (overall knowledge score of 71%). A majority (60.2%) of the respondents also had a positive attitude towards CAUTI prevention. There was no significant association between nurse related factors (knowledge & attitude) and nurse’ compliance (all p >0.05). However, some of the key informants felt that inadequate knowledge on CAUTI prevention guidelines was a factor hindering nurse’ compliance. Conclusion & Recommendation: The nurses’ level of compliance with CAUTI guidelines was poor. The null hypothesis (H0) was accepted (p > 0.05) which implies that nurses’ knowledge and attitude do not influence their compliance with CAUTI guidelines. Further studies should be carried out on other factors, for example institutional factors that might influence nurse’ compliance with guidelines for CAUTI prevention.
Keywords:
Compliance, Urinary tract infection, Nurses, CDC, Indwelling urinary catheter
Cite this paper: Methu C. W. , Mwenda C. M. , Mbugua R. G. , Nurse Factors Influencing Compliance with CDC Guidelines for Catheter Associated Urinary Tract Infection Prevention in a Referral Hospital in Kenya, International Journal of Nursing Science, Vol. 9 No. 3, 2019, pp. 70-76. doi: 10.5923/j.nursing.20190903.03.
1. Introduction
Urinary tract infections (UTIs) account for approximately 34% of all nosocomial infections worldwide. These infections are the most common hospital associated infections in developed countries. 75% of UTIs are attributed to the use of indwelling urinary catheters [1]. According to the United States Centre for Disease Control (CDC) a catheter associated urinary tract infection (CAUTI) is defined as an infection occurring in an individual who has had an indwelling catheter for 2 days or more and is experiencing one or more signs and symptoms (urinary frequency or urgency, fever, suprapubic tenderness, dysuria or costovertebral angle tenderness) or has a urine culture of >10CFU/mL bacterial species [2]. In a report released by the CDC in 2013 the pooled means for CAUTI for intensive care units (ICUs) varied from 1.2 per 1000 urinary catheter days in medical-surgical ICUs to 4.1 in burn ICUs. Non-ICU rates ranged from 1.3 to 1.5 per 1000 catheter days. The incidence of CAUTI in ICUs in selected low and middle-income countries was found to be 4.8 per 1000 device days [3]. In Kenya, the burden of CAUTI has been reported only at a facility level, that is at Kenyatta Hospital where CAUTI incidence was found to be 32% [4].Catheter associated urinary tract infections have been linked to a number of complications namely secondary blood stream infections, extended hospital stays, increased treatment costs, local and systemic morbidity and mortality. As it is estimated that 69% of CAUTI are avoidable [5], the CDC in collaboration with the Association for Professionals in Infection Control and Epidemiology (APIC) developed guidelines for the prevention of CAUTI in 1981 which were then updated in 2009. These guidelines offer the best practices for preventing CAUTI. They focus on appropriate indications for catheter placement, catheter insertion techniques, catheter care and maintenance, specimen collection, documentation and surveillance [2].Several studies have been carried out to demonstrate the effect of implementing the CDC guidelines via the use of catheter care bundles. These bundles draw from the recommendations outlined in the guidelines. After implementing a catheter bundle one study observed a significant reduction in monthly CAUTI rates. Additionally, a reduction in CAUTI rate from 2.3 per 1000 device days in 2008 to 0.3 per 1000 devise days in 2011 and 0.1 and 0.2 in 2015 and 2016 was seen [6]. Another study observed an 80% reduction in CAUTI rate after implementing a 5-S CAUTI bundle [7].Most of the recommendations in the guidelines are considered nurse-led interventions as nurses are primary care givers and play an important role in diagnosing CAUTI [1]. Nurses are also considered pivotal in quality improvement efforts. However, whereas the implementation of these guidelines in reducing CAUTI rates has been demonstrated CAUTI cases persist in hospitalized patients. In addition, several studies have shown inconsistent application of these guidelines with widespread inappropriate use of urinary catheters. It has also been observed that catheters remain in place for long durations as health personnel are often unaware of catheter insertion and on-going care due to poor documentation [8-10].Studies have also demonstrated knowledge deficit among nurses regarding the prevention of CAUTI [11-13]. Nurses’ attitude toward CAUTI prevention has also been shown to be mostly negative [14]. Locally, only a few studies have been carried out in regards to CAUTI but none focusing on nurse factors that might influence compliance with established CAUTI prevention guidelines. This formed the basis for the researcher’s motivation to conduct a study on nurse factors influencing compliance with CDC guidelines for CAUTI prevention at Embu Level 5 Hospital. The objectives of the study were to assess the level of compliance with the CDC guidelines for CAUTI prevention, to determine nurse related factors influencing compliance and to examine the association between nurse factors and compliance with CDC guidelines among nurses at Embu level 5 hospital.
2. Methods
A descriptive cross-sectional study design was used for this study. The study site was Embu level hospital which is located in Embu County and is about one kilometer from Embu town on the Embu – Meru highway. The hospital has a bed capacity of 618 beds and 12 departments; Outpatient services, radiology, laboratory, dental, ophthalmology, surgical, medical, obstetrics/gynecology (Obs/Gyn), CCC, psychiatric, public health and MCH. It has 217 nursing personnel. A sample size of 107 nurses was calculated using the Yamane formula (1967). Purposive sampling was used to select the departments (medical, surgical, obstetrics/gynecology) to be involved in the study. A proportionate sample for each department was calculated and then the duty rosters from each department were used as a sampling frame and the target population divided by 107 to get a sampling interval (K) of 2. Thus, every 2nd nurse who agreed to take part in the study was included (stratified random sampling).A self-administered structured questionnaire based on the CDC guidelines was developed by the researcher. An interview guide was also used to collect qualitative data from selected key informants. The independent variables in the study were knowledge and attitude while the dependent variable was level of compliance to the guidelines. Validity of the data collection tools was tested by pre-testing of the questionnaires and interview guides and necessary adjustments carried out. In order to ensure reliability, the researcher designed questions that were not ambiguous and that were easy to score and gave clear instructions for the respondents.Qualitative data was transcribed from verbatim into a word document then converted to PDF format. This was then uploaded to NVIVO version 12 software and a word frequency run. The most prominent themes that emerged were then sorted and categorized. Quantitative data was coded and entered into SPSS version 21 software for analysis. Descriptive statistics, that is, percentages and frequencies were used while the chi-square test was utilized for inferential statistics where the p value was set at <0.05. Data was presented in the form of frequency tables, charts and narrations. Ethical approval for the research study was secured from the ethical review committee at Mount Kenya University and the National Commission for Science Technology and Innovation (NACOSTI). Permission to collect data was acquired from the County Health Services, the hospital’s Medical Superintendent, the Chief Nurse and the Ward-in Charges. Lastly, informed consent was obtained from the study respondents.
3. Findings
3.1. Demographic Characteristics
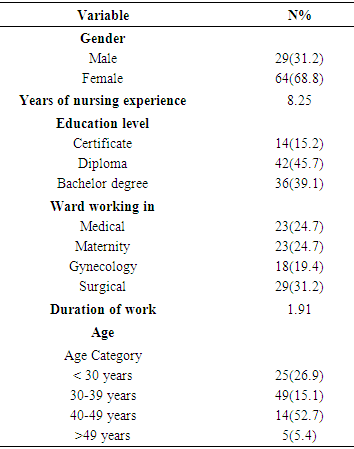
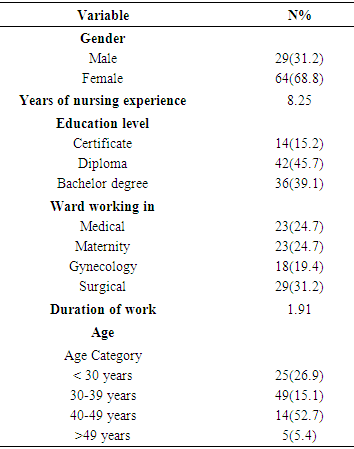
Out of a sample size of 107 nurses 86% (93) returned the questionnaires duly filled. Of these, 68.8% (64) were female whereas 31.2% (29) were male. The average period of nursing experience among the respondents was 8 years and most of the nurses [45.7% (42)] were diploma holders whereas 15.2% (14) and 39.1% (36) were certificate holders and graduate nurses respectively. A majority [44.1% (41)] of the nurses worked in the Obs/Gyn department followed by those working in the surgical department [31.2% (29)] and 24.7% (23) worked in the medical department. Most of the respondents [52.7% (49)] were between the age of 30 to 39 years followed by those less than 30 years [26.9% (25)] whereas those above 40 years were 20.5% (19), (See Table 1).Table 1. Respondent’s demographic characteristics
 |
| |
|
3.2. Nurse Factors Influencing Compliance with CDC Guidelines for CAUTI Prevention
3.2.1. Knowledge of CDC Guidelines for CAUTI Prevention
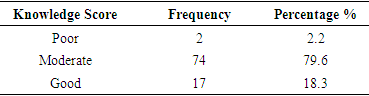
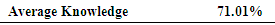
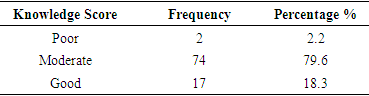
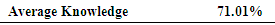
The study evaluated the nurses’ knowledge on the CDC guidelines for CAUTI prevention. It was observed that 66.7% (62) of the respondents were aware of the CDC guidelines for CAUTI prevention but only 16.1% (15) had received specific training on the same. The overall knowledge score of the participants was 71% indicating that the participants’ knowledge regarding CAUTI prevention was moderate. To come up with this score all the appropriate response percentages (total percentage sum = 922.9) were added up and then divided by the total number of items (13). The MacDonald’s standards of learning outcome measuring criteria was then used to rate the respondent’s level of knowledge (Table 2). Table 2. Knowledge rating of respondents
 |
| |
|
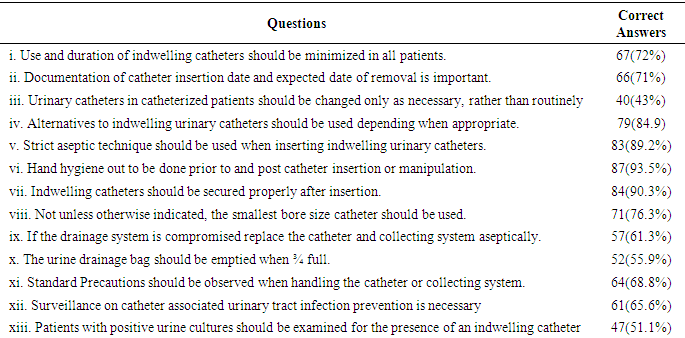
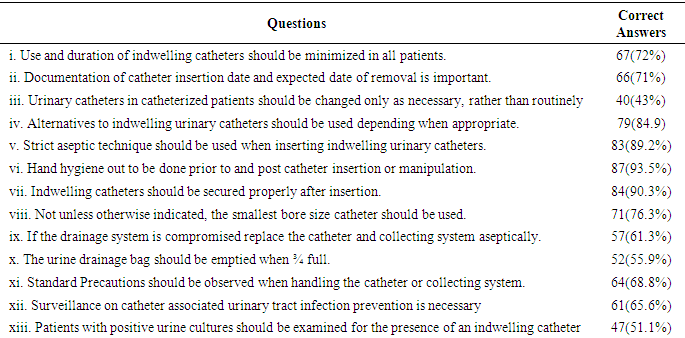
The key informants also opined that the nurses at the facility had the knowledge and skills regarding CAUTI prevention as reported by R1 “Most of the nurses are knowledgeable regarding catheter care and infection prevention though they need regular CMEs”. 72% (67) of the nurses responded correctly use of indwelling catheters and duration of placement should be minimized in all patients. 71% (66) of the participants also correctly identified documentation of catheter insertion date and expected date of removal as being key in preventing development of CAUTI. Employment of aseptic method for catheter placement to prevent CAUTI occurrence was also correctly identified by 89.2% (83) of the nurses while 93.5% (87) indicated that hand hygiene should be performed prior to and post catheter insertion or handling. However, only 43% (40) of the participants correctly responded that urinary catheters ought to be changed only as necessary rather than routinely. This data coincides with that from the key informants who reported that urinary catheters should be changed routinely that is after every 2 weeks. R3 reported “In our facility we change urinary catheters after every 2 weeks…” Also, 48.9% (46) of the nurses were not aware that patients whose urine cultures tested positive need to be examined for the existence of an indwelling catheter and a CAUTI. Table 3. Nurses’ knowledge on CDC guidelines for CAUTI prevention (percentage of correct answers) (N=93)
 |
| |
|
Table 4. Overall knowledge scores (N=93)
 |
| |
|
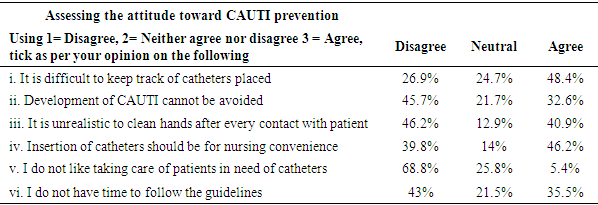
3.2.2. Attitude towards CAUTI Prevention
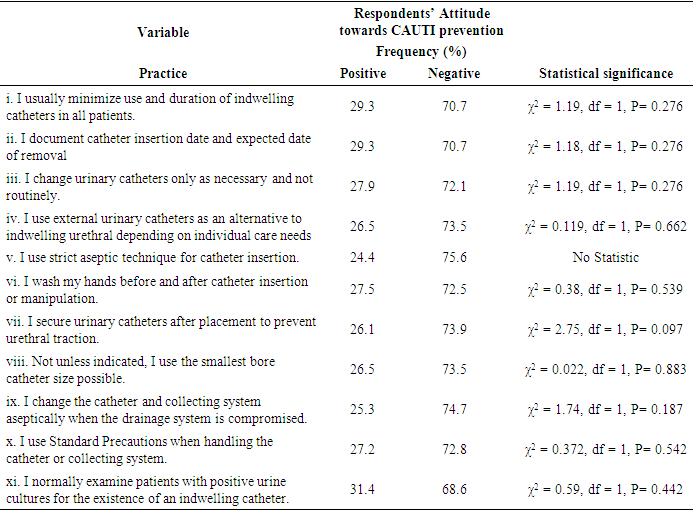
According to the study results, 48.4% (45) of the respondents felt that it was difficult to keep track of catheters placed. This was supported from information collected from the key informants. The ratio of nurses to patients is a hindrance to keeping track of catheters placed in patients as reported by one of the informants, “To be sincere one can forget that you inserted a catheter even though the date is in the file. Due to the workload one tends to forget”. Only 45.7% (43) of the respondents were of the opinion that development of CAUTI cannot be avoided while opinions were divided on whether it is unrealistic to wash hands post every contact with the patients. Insertion of catheters as a nursing convenience was agreed upon by 46.2% (43) while 35.5% (33) of the nurses felt that they did not have time to follow the guidelines, see Table 5. According to data from the key informants urinary catheterization is done mainly for nursing convenience as reported by R4, “So what we do basically in the wards for all bed ridden patients is we catheterize them to avoid them getting bed sores and also this helps to conserve linens which might not be enough for other patients if we keep changing linens. Table 5. Nurses’ attitude towards CAUTI prevention
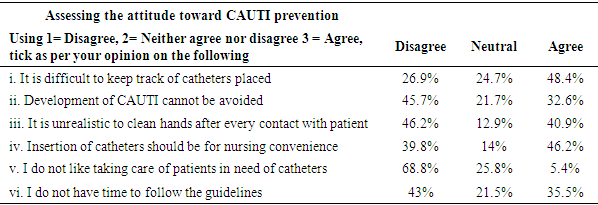 |
| |
|
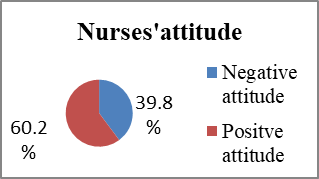
As seen in the figure below, the study results indicate that 60.2% nurses working at the facility had a positive attitude towards prevention of CAUTI. First all negatively formed questions (4) were reversed. Then the aggregate score was worked out and then used to obtain the mean. Categorization of the respondents’ attitude as either positive or negative was based on the mean score (39.1%) selected as the cut-off point. Therefore, the resulting categories were as follows; 39.8% were rated as having negative attitude because their score fell below the mean and 60.2.% of the nurses who were rated as having a positive attitude had a score above the mean.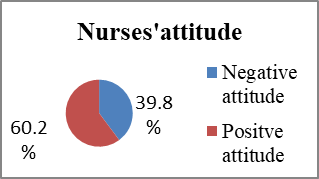 | Figure 1. Nurses’ attitude towards CAUTI prevention |
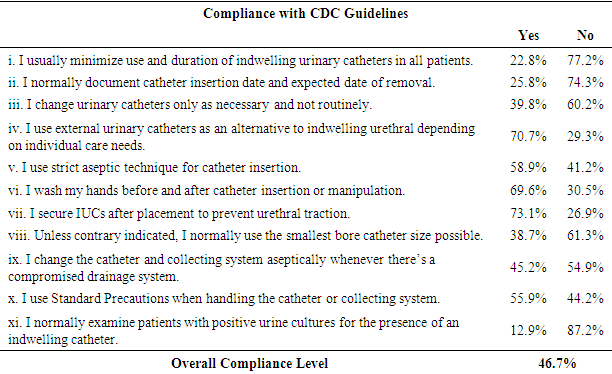
3.3. Nurses’ Level of Compliance with CDC Guidelines for CAUTI Prevention
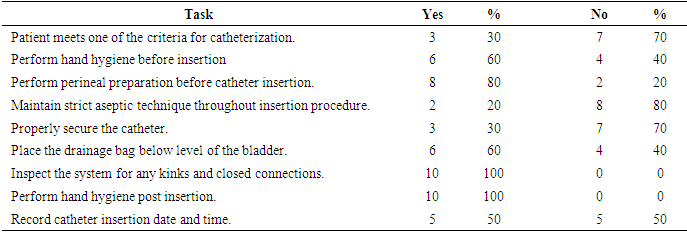
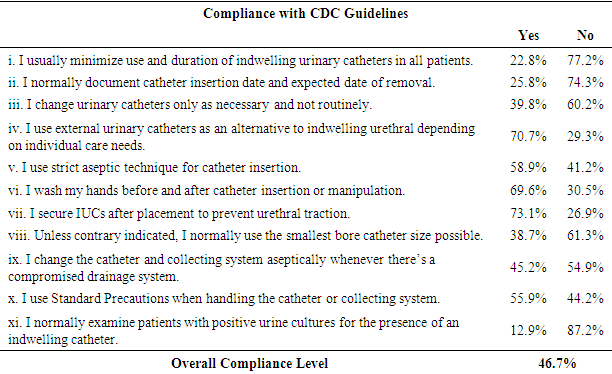
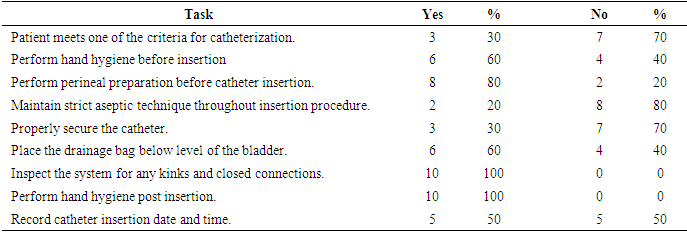
The overall level of compliance was low (46.7%). The overall score was attained by adding up all individual score percentages (total percentage sum = 889) then dividing by the number of items (no. of items = 11). As can be seen from Table 6, implementation of the CDC guidelines varied with only 22.8% minimizing urinary catheter use in patients while 25.8% reported documenting catheter insertion date and expected date of removal. This is consistent with data obtained from observation where only 30% (3) respondents observed inserted IUCs in patients with appropriate indications and half of the participants 50% (5) remembered to document the catheter insertion date and time. Nearly 40% of the respondents reported changing urinary catheters only as necessary and not routinely while 70.7% used external catheters as an alternative to IUCs depending on individual care needs. Most of the respondents, 58.9% reported using aseptic technique for catheter insertion, 69.6% performed hand hygiene while 73.1% prevented urethral traction by properly securing indwelling catheters after placement. Qualitative data showed that 60% (6) washed their hands before IUC insertion and 100% (10) washed hands after insertion. However, only 20% (2) were seen to observe strict aseptic technique as most could not obtain sterile equipment and some sterile gloves while only 30% (3) secured the IUC to prevent movement and irritation. Only 38.7% of the nurses reported using the smallest bore catheter size possible. 45.2% replaced the catheter and collecting system aseptically while, 55.9% used Standard Precautions with only 12.9% of the respondents reported examining patients with positive urine cultures for the presence of an indwelling catheter. Table 6. Nurses’ compliance with CDC guidelines for CAUTI prevention (N=93)
 |
| |
|
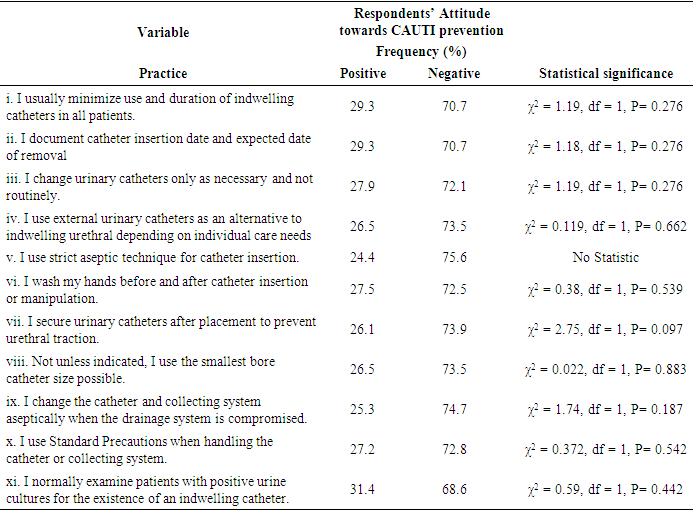
3.4. Relationship between Knowledge and Compliance with CAUTI Prevention Guidelines
As can be observed from table 8 no statistically significant relationships were observed between the nurses’ knowledge and implementation of the CDC guidelines on CAUTI prevention (p>0.05). Thus, the null hypothesis was accepted.Table 7. Distribution of respondents according to observation of performed tasks (N=10)
 |
| |
|
Table 8. Relationship between nurses’ attitude and compliance with CDC guidelines for CAUTI prevention
 |
| |
|
4. Discussion
Results from the current study indicated that the majority of nurses are knowledgeable (overall knowledge score - 71.1%) regarding most of the CDC guidelines statements for CAUTI prevention among them use of aseptic technique, minimizing use and duration of indwelling catheterization and use of alternatives to indwelling catheters. These results are consistent with findings from a study carried out in Minnesota by [15]. The survey evaluated foley catheter use and knowledge among nurses in Minnesota. It was surmised that the Minnesota RNs exhibited high level of appreciation of the function of expeditious catheter removal in averting CAUTI. However, some gaps in knowledge were identified in the current study. Most nurses were not aware that incontinence is not an indication for indwelling catheterization, IUCs should be changed only as necessary and not routinely and that surveillance of CAUTI is crucial. These findings concur with those from a study conducted by Mukakamanzi which evaluated the knowledge, attitude and practices of nurses toward prevention of CAUTI in selected referral hospitals in Rwanda. Nurses were not aware of the inappropriate indications for urethral catheterization and that urinary catheters should not be changed routinely or at fixed intervals [13]. The study also revealed that a majority (66.7%) of the participants had heard of the CDC guidelines for CAUTI prevention however only a few (16.1%) had received specific training on the guidelines. A statistically significant difference in knowledge between those that were aware of the CDC guidelines for CAUTI prevention and those that were not was noted (p = 0.018). However, there was no statistically significant association observed between the nurses’ knowledge of the CDC guidelines for CAUTI prevention and having specific training on the guidelines. This is contrary to findings from a study carried out by [4] which sought to determine the factors affecting nurses’ adherence to standard safety measures for infection prevention at Mbagathi District Hospital, Kenya. The study revealed a statistically significant difference in knowledge between those nurses trained formally on infection prevention and those that hadn’t received training (p = 0.027).In this study a majority (60.2%) of the respondents were found to have a positive attitude towards CAUTI prevention. Only a few of the respondents felt that it was difficult to keep track of catheters placed and also most of the respondents felt that development of CAUTI could be avoided. In regards to adhering to the guidelines, less than half of the participants felt that they had the time to follow the guidelines. These results are not unique to this study as another study by [13] showed that most nurses had a positive attitude in regards to catheter indications and CAUTI prevention. The current study results indicate that nurses’ level of implementation of the CDC guidelines for CAUTI prevention is low (40.6%) despite most participants being knowledgeable regarding the guidelines. Only a small proportion of the respondents indicated that they minimized utility and period of catheterization in all patients (22.8%). Documentation of catheter insertion date and expected date of removal was carried out only by a few of the respondents (25.8%). It was also reported by the key informants that indwelling catheters were routinely changed after every 2 weeks which tallied with quantitative data from the participants where only 39.8% reported changing urinary catheters as necessary and not routinely. Strict aseptic technique during catheter placement was reported by most of the participants however only 20% of those observed performing catheter insertion were seen to observe strict aseptic technique. The results from this study are consistent with findings from a study by [16] that sought to evaluate observance of practice guidelines of the UK’s CAUTI bundle. The study results showed a general lack of consistent catheter care over a 5-day duration and also revealed that compliance with each specific CAUTI bundle criteria decreased with each passing day. These findings contrast with those from a study carried out in Rwanda by [13] which sought to evaluate nurses’ practices, attitude and knowledge regarding CAUTI prevention. The study demonstrated that despite the nurses having a low level of knowledge the level of implementation was moderate (79.9%). A majority of the study respondents (96.2%) washed their hands after catheter insertion. Most of the respondents used aseptic technique (52%) during catheter insertion and a few of the respondents secured the IUC after placement to avert urethral traction.It was hypothesized that nurse-related factors, that is, knowledge and attitude did not influence compliance with CDC guidelines for CAUTI prevention. Analysis of these variables showed no statistically significant relationships between nurse related factors (knowledge and attitude) and implementation of the CDC guidelines among the nurses (all p>0.05). Hence, the null hypothesis was accepted. The results from this study contradict findings from other studies. One such study is by [17] that sought to investigate nurses’ perceived barriers to implementing of evidence-based practices (EBP) found that a limited knowledge of EBP was one of the barriers to implementation identified. The results were comparable to those obtained from a study carried out by [18] that sought to determine nurses’ perceptions of nursing practice based on scientific evidence. Time and knowledge were largely cited as the most common barriers to implementing evidence-based practice.
5. Conclusions and Recommendations
There were no significant associations observed between nurse related factors and their compliance with CAUTI prevention guidelines. Thus, according to the study nurse related factors do not influence their compliance with specified guidelines. However, information from the key informants suggests that nurses require regular updates on CAUTI prevention in the form of continuous medical education (CMEs). The study findings also showed that the nurses’ level of compliance with CDC guidelines for CAUTI prevention was low. The researcher therefore recommends that the hospital organize regular CMEs on CAUTI prevention in order to keep the nurses updated on current evidence-based practices. A second recommendation is that monitoring of nurse’ compliance with CAUTI prevention guidelines be conducted on a regular basis in order to ensure provision of quality care.
ACKNOWLEDGEMENTS
The authors would like to appreciate Embu level 5 hospital management and the nurses in the Surgical, Medical and Obs/Gyn departments who took part in the study. The support accorded by Mount Kenya University’s research department is also appreciated.
References
| [1] | National Health Statistics Network (2018). Healthcare-acquired infections (HAIs). Patientcarelink.org GooleSearch(n.d.). Retrieved September 7, 2019, from https://0x9.me/q6sTH. |
| [2] | Catheter-associated Urinary Tract Infections (CAUTI) | HAI | CDC. (2019, April 16). Retrieved September 3, 2019, from https://www.cdc.gov/hai/ca_uti/uti.html. |
| [3] | Rosenthal, V. D., Al-Abdely, H. M., El-Kholy, A. A., AlKhawaja, S. A. A., Leblebicioglu, H., Mehta, Y., … Salama, M. F. (2016). International Nosocomial Infection Control Consortium report, data summary of 50 countries for 2010-2015: Device-associated module. American Journal of Infection Control, 44(12), 1495–1504. |
| [4] | Maturi P.M, (2010). "The prevalence of Nosocomial Urinary Tract Infections in patients with indweling urinary catheters at Kenyatta National Hospital." UON Digital Repository. 2010. Accessed from http://hdl.handle.net/11295/25007erepository.uonbi.ac.ke. |
| [5] | Rebmann, T., & Greene, L. R. (2010). Preventing catheter-associated urinary tract infections: An executive summary of the Association for Professionals in Infection Control and Epidemiology, Inc, Elimination Guide. American Journal of Infection Control, 38(8), 644–646. |
| [6] | Al-Hameed, F. M., Ahmed, G. R., AlSaedi, A. A., Bhutta, M. J., Al-Hameed, F. F., & AlShamrani, M. M. (2018). Applying preventive measures leading to significant reduction of catheter-associated urinary tract infections in adult intensive careunit. Saudi Medical Journal, 39(1), 97–102. https://doi.org/10.15537/smj.2018.1.20999. |
| [7] | Elkbuli, A., Miller, A., Boneva, D., Puyana, S., Bernal, E., Hai, S., & McKenney, M. (2018). Targeting Catheter-Associated Urinary Tract Infections in a Trauma Population: A 5-S Bundle Preventive Approach. Journal of Trauma Nursing, 25(6), 366. https://doi.org/10.1097/JTN.0000000000000403. |
| [8] | Dailly, S. (2012). Auditing urinary catheter care. Nursing Standard (through 2013), 26(20), 35. |
| [9] | Meddings J., R. M. (2017). Reducing unnecessary urinary catheter use and other startegies to prevent catheter-associated urinary tract infections: An integrative review. BMJ Quality and Safety Journal, 23(1), 277-289. doi:https://doi.org/10.1136/bmjqs-2012-001774. |
| [10] | Winter, M., Helms, B., Harrington, L., Luquire, R., McVay, T., & Rhodes, N. (2009). Eliminating Catheter-Associated Urinary Tract Infections: Part I. Avoid Catheter Use. Journal for Healthcare Quality, 31(6), 8–12. |
| [11] | Jain, M., Dogra, V., Mishra, B., Thakur, A., & Loomba, P. S. (2015). Knowledge and attitude of doctors and nurses regarding indication for catheterization and prevention of catheter-associated urinary tract infection in a tertiary care hospital. Indian Journal of Critical Care Medicine: Peer-Reviewed, Official Publication of Indian Society of Critical Care Medicine, 19(2), 76. |
| [12] | Mohammed, H. T., & Hamza, R. A. H. (2019). Effectiveness of Educational Program on Nurses’ Knowledge toward Preventing Female Catheter-Associated Urinary Tract Infections. Prof. RK Sharma, 13(1), 230. |
| [13] | Mukakamanzi, J. (2017). Knowledge, attitude and practices of nurses towards the prevention of catheter-associated urinary tract infection in selected Referral Hospitals in Rwanda. (PhD Thesis). University of Rwanda. |
| [14] | Shehzadi, A., Afsar Ali, M., & Bhatti, R. (2018). Saudi Journal of Nursing and Health Care ISSN: 2616-7921 (Print). |
| [15] | Drekonja D.M., Kuskwoski M.A., Johnson J.R. (2010). Internet survey of foley catheter practices and knowledge among Minnesota nurses. American Journal of Infection Control; 38(1): 317 Retrieved from http://www.ajicjournal.org/article/S0196-6553(09)00660-9/fulltext. |
| [16] | Johnston, J. (2015). An Evaluation of the Adherence to an Indwelling Urinary Catheter Maintenanc Budle. DNP Projects. Retrieved from https://uknowledge.uky.edu/dnp_etds/33. |
| [17] | Gerrish K., Clayton J. (2004). Evidence-based practice: An organizational approach. Journal of Nursing Management; 12; 114-123. |
| [18] | Koehn M.L., Lehman K. (2008). Nurses' perceptions of evidence-based nursing practice. Journal of Advanced Nuring, 62(2); 209-215. doi:10.1111/j.13652648.2007.04589. |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML