-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2019; 9(3): 65-69
doi:10.5923/j.nursing.20190903.02

Perinatal Factors Associated with Birth Asphyxia among Neonates at a County Referral Hospital in Kenya
Beatrice Kadenyeka Amadi1, Sherry Oluchina2, Drusilla Makworo2, Bernard Mbithi2
1School of Nursing, Jomo Kenyatta University of Agriculture and Technology and Nursing Officer at Kenyatta National Hospital, Nairobi, Kenya
2School of Nursing, Jomo Kenyatta University of Agriculture and Technology, Kiambu, Kenya
Correspondence to: Beatrice Kadenyeka Amadi, School of Nursing, Jomo Kenyatta University of Agriculture and Technology and Nursing Officer at Kenyatta National Hospital, Nairobi, Kenya.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

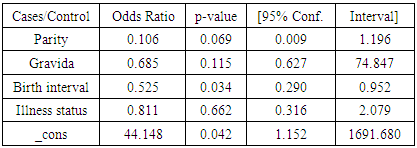
Perinatal asphyxia is a common and serious neonatal problem globally and significantly contributes to both neonatal morbidity and mortality given that it is a major cause of death and of acquired brain damage in newborns. Therefore, the objective of this study was to determine the antepartum risk factors associated with perinatal asphyxia among neonates. This was an unmatched mixed case control study, conducted at a County Referral Hospital (MCRH) in Nairobi (Kenya). Participants were assigned into case or control groups purposively whilst excluding patients with congenital anomalies. The sample size comprised 124 participants, 31 cases and 93 controls, with controls being systematically picked at intervals of 4. A questionnaire, a data collection form designed with pre-coded responses, and a key informant guide were used to collect both quantitative and qualitative data respectively. Odds ratios for Mantel Haenszel method and unconditional logistic regression were obtained using STATA 14 software, with statistical inference done at an alpha level of significance of 0.05. The study findings revealed that age, marital status, employment status, and education level were not significantly associated with perinatal asphyxia. Birth interval was the only significant antepartum factor associated with perinatal asphyxia. For every unit increase in the birth interval, the log-likelihood of having a baby with perinatal asphyxia reduces by 0.5 times (OR = 0.525; p=0.03). This observation on birth interval could be due to the fact that the longer the break between deliveries, the lesser the likelihood for complications as the reproductive systems would then have fully been restored.
Keywords: Asphyxia, Neonates, Perinatal, Risk Factors
Cite this paper: Beatrice Kadenyeka Amadi, Sherry Oluchina, Drusilla Makworo, Bernard Mbithi, Perinatal Factors Associated with Birth Asphyxia among Neonates at a County Referral Hospital in Kenya, International Journal of Nursing Science, Vol. 9 No. 3, 2019, pp. 65-69. doi: 10.5923/j.nursing.20190903.02.
Article Outline
1. Introduction
1.1. Background of the Study
- Globally, deaths caused by perinatal asphyxia account for about 23% of the deaths among four million neonatal deaths, with an estimated one million survivors developing such complications like cerebral palsy and mental retardation. When new-borns are deprived of oxygen, for a period long enough to cause physical harm especially to the brain, the condition is referred to as perinatal asphyxia (PA) [1]. World Health Organization (WHO) defines perinatal asphyxia as the failure to sustain, or in extreme circumstances to initiate breathing at birth. Causes of perinatal asphyxia include birth trauma, congenital sepsis or maternal opiates, intrauterine pneumonia, severe meconium aspiration, cord compression, congenital pulmonary or cardiac anomalies, narcotic administration or a transplacental anaesthetic, obstructed airway, or placental abruption [2]. Perinatal asphyxia clinically presents with cardio-respiratory and neurological depression with Apgar score persistently <7 within the first 5 minutes of birth coupled with evident hypoxic compromise resulting in acidemia [1].The prevalence and mortality rates for PA are also high. In resource-poor countries like Africa, the incidence is even higher, with Kenya having a prevalence rate of about 5.1% [3]. However, these incidences are sometimes an underrepresentation of the actual prevalence of PA in the community given the exclusion of any occurrences outside health facility settings. Nairobi County has some of the best facilities nationwide for delivering care to patients of acute neonatal complications. Data from District Health Information System (DHIS 2) shows that close to 50% of New Born Unit (NBU) admissions are due to birth asphyxia. However, there is no documented data on the determination of perinatal risk factors in the County Referral Hospital where the study was conducted [4].
1.2. Research Objective
- To determine the antepartum risk factors associated with perinatal asphyxia among neonates at a County referral hospital in Kenya.
2. Methodology
2.1. Study Design
- This was an unmatched mixed case control study. According to Yin, case control studies are designs used to retrospectively establish the relationship between risk factors and a given outcome by comparing the frequency of the exposure among two groups (those with and those without the disease or outcome of interest) [5]. The study design was also suitable for rare disease outcomes such as perinatal asphyxia. According to Global Genes (2018) and the National Organization for Rare Diseases (NORD)’s Database, Perinatal Asphyxia was listed as a rare disease [6].
2.2. Sampling and Recruitment Procedure
- The study participants were classified into case or control groups, at a ratio of 1:3 respectively. Multiple studies suggest a ration of anything between 1:1 and 1:4 for cases to controls [7,8]. It has also been noted that a matching ratio up to 1:4 case to control ratio elicits the lowest bias [7]. However, the financial feasibility of the chosen approach was cited as a contributory factor to the ratio. The assignment of participants into case or control groups was purposive and solely based on them having or not having perinatal asphyxia respectively. During this assignment into participant groups, the patients were also screened for other congenital anomalies so that those who had any such kind of anomalies were excluded from the study entirely. Upon isolation of the cases, systematic sampling was used to pick controls through at an interval of 4 given that the estimated number of non-asphyxia deliveries per month was 426, representing 70.9% of the estimated 600 deliveries and the sample for controls was estimated to be 93. As for the Key informant guide, a census approach was used where all the 57 workers in the maternity unit were allowed to participate. However, the point of saturation technique was used to determine the point at which the diversity of the responses ceased leading to no new information gathered. This point was reached after 30 interviews.
2.3. Data Management
- The questionnaires were pre-coded for ease of data entry. All the raw data was reviewed by the researcher and cross-checked to ensure completeness. The filled questionnaires were kept in a safe and confidential place that was accessible only to the researcher awaiting data entry. After cross-checking the information in the questionnaires, a data entry template was designed in Epidata to allow for the setting of controls and validation of the variables, thereby preventing data entry errors. On completion of the data entry exercise, the data was exported to STATA version 14 for analysis. Data analysis involved univariate analysis for descriptive statistics (frequencies and percentages for categorical variables, and means, median and standard deviations for continuous variables). Bivariate and multivariate analysis, specifically the Mantel Haenszel method and unconditional logistic regression were afterward used to obtain odds ratios, regression coefficients, p-values, and confidence intervals. The unconditional logistic regression was used since the study was of unmatched case control design and given that the dependent variable was binary, with two mutually exclusive outcomes (presence or absence of Perinatal Asphyxia). Hypothesis testing was done at an alpha level of significance of .05 such that any p-values below the alpha were deemed significant. Qualitative data were analysed thematically. The codes were then revised routinely as new information was gathered from the qualitative data collection tools. The qualitative data were then used to support the outcome of the quantitative data as well as develop grounded theories for basing study conclusions. Data were presented using tables and narratives.
2.4. Ethical Considerations
- Approvals and research permits were sought from all relevant institutions in the study. The researcher and research assistants collected data that was not too sensitive, and when the situations got sensitive, the participants were assured and reassured. Illiterate participants were allowed to take part through translated Swahili version of the consent and data collection forms. Written and signed consents were obtained from each participant after a detailed explanation of the study being undertaken. Additionally, authors do not have conflicting or competing interests towards the publication of this study.
3. Results
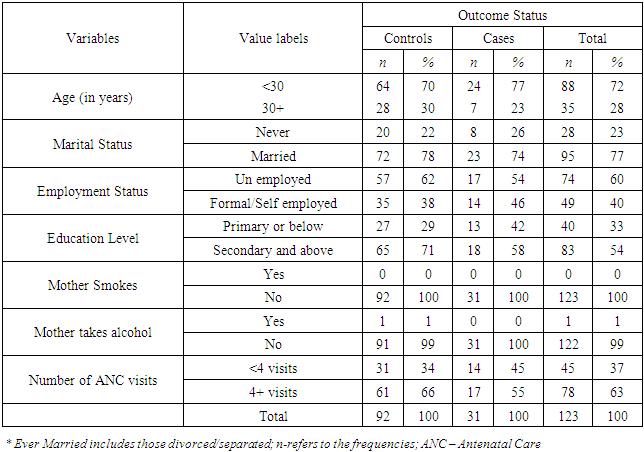
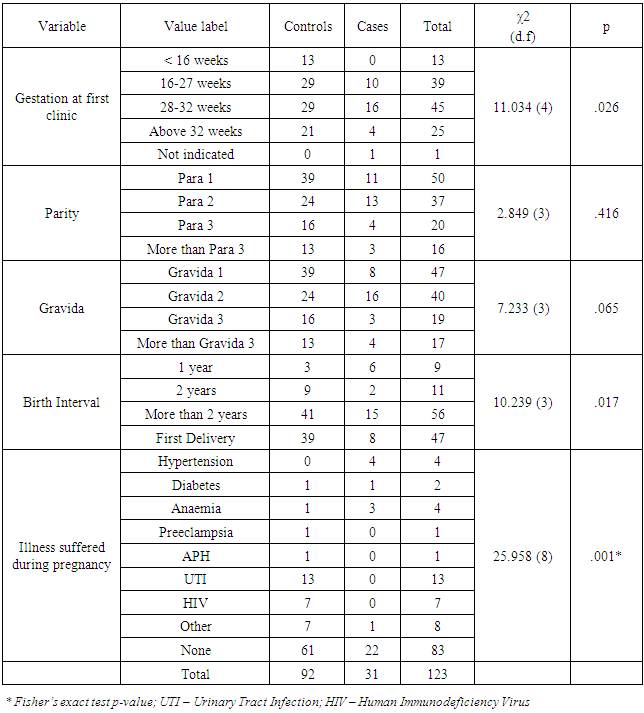
- This section presents the findings of the study. The frequencies are presented along with the Pearson chi-square test for antepartum factors, and Cochran-Mantel Hansel chi-square test results for the inferential statistics. The key informant responses conducted on 20 professionals within the hospital are also triangulated with the quantitative findings. Of the 124 study participants, 123 provided complete information that was then used to provide the analysis.Table 1 shows a descriptive analysis of the socio-demographic data.
|
|
|
4. Discussions
- Age, marital status, employment status, and education level did not have statistically significant differences across its categories. These findings were inconsistent with what Aslam et al.’s report that decreasing or increasing maternal age affected the likelihood of developing perinatal asphyxia [9]. These findings were also not consistent with reports from Tabassum et al. and Seikku et al. [10,11]. While Tabassum et al indicated that perinatal asphyxia was significantly associated with maternal literacy and the knowledge of mothers on health-related issues including attendance to antenatal care, Seikku et al. reported that the risk for low birth weight, and consequently of asphyxia is higher among those with single marital status (either unmarried or separated) [10,11]. They also found out that mother’s unemployment, mother's age below 20 years, and low literacy levels for mothers were other risk factors for perinatal asphyxia. In addition, these findings were not in line with Lawn et al. who suggested that a low level of education was also associated with perinatal asphyxia [12]. However, these findings could act as support for Rani et al.’s argument that using maternal literacy levels to determine their predisposing conditions could be misleading since literacy is a cross-cutting indicator for socio-economic levels [13]. While maternal age was not statistically significant, the gestational age at first ANC visit yielded statistically significant correlations with perinatal asphyxia. These findings support the indication by Onyearugha & Ugboma that perinatal asphyxia was significantly influenced by antenatal attendance in primary healthcare facilities [14]. The findings also agree with Seikku et al. report which showed that gestational age affected other mother-related characteristics that led to neurologic morbidity including perinatal asphyxia. However, Chiabi et al., following a study in a Cameroonian urban health facility on birth asphyxia risk factors, suggested that what matters is the quality of the care accorded as opposed to the number of consultations [15].Additionally, birth interval yielded statistically significant associations with perinatal asphyxia, such that as parity increased, the likelihood of developing perinatal asphyxia decreased. These findings were consistent with those of another study which reported that child spacing of at least 36 months apart minimized the risk of infant morbidity and mortality [16]. These findings also contradicted the findings of another study by Seikku et al. which established that birth intervals longer than 5 years were associated with adverse perinatal outcomes forcing such patients to deliver through caesarean section [11]. The conditions suffered such as oligohydromnious, meconium aspirate syndrome, and chronic illnesses were found to be associated with perinatal asphyxia. These findings were consistent with Seikku et al.’s report that neurologic morbidity increased the likelihood of developing further conditions such as perinatal asphyxia [11]. Finally, the study found no correlation between birth asphyxia and the number of ANC visits. This finding was inconsistent with reports by Onyearugha & Ugboma that lack of antenatal care, is an independent risk factor for neonatal encephalopathy, a complication of perinatal asphyxia [14].
5. Conclusions
- The study results demonstrated that greater birth interval reduced the likelihood of developing perinatal asphyxia by 0.5 times (OR = 0.525; p=.03). Reducing the confidence interval to 90% would show more factors to be significant such as gestational age and illnesses suffered during pregnancy.
ACKNOWLEDGEMENTS
- The study would like to acknowledge Beatrice Kadenyeka Amadi, Sherry Oluchina, BScN, MScN, PhD, Drusilla Makworo, BScN, MScN, PhD, and Bernard Mbithi, BScN, MSc (PH), PhD. Beatrice was the principal investigator for the study and was also involved in developing the manuscript write-up for publication. Sherry, Drusilla, and Bernard were involved in supervising the study activities from its inception to completion.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML