Catherine Mwangi1, Lucy W. Meng’anyi2, Ruth G. Mbugua3
1School of Nursing, Mount Kenya University, Nairobi, Kenya
2Department of Medical Surgical Nursing, School of Nursing, Mount Kenya University, Nairobi, Kenya
3Department of Community Health Nursing, School of Nursing, Mount Kenya University, Nairobi, Kenya
Correspondence to: Lucy W. Meng’anyi, Department of Medical Surgical Nursing, School of Nursing, Mount Kenya University, Nairobi, Kenya.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Background: The nursing process is a valuable tool that has revolutionized nursing practice for better patient outcome. Utilization of nursing process (NP) is however usually compromised by various internal and external factors. Objective: The aim of this study was to assess Knowledge, Attitude, Practices and Hospital factors affecting the utilization of nursing process among nurses in Thika Level 5 Hospital. Methods: A descriptive cross sectional study was conducted in the month of September 2017 where 69 respondents were randomly sampled from nurses in medical, surgical and paediatric units. Data on knowledge and attitude was collected using a self-administered questionnaire and Key Informant Interview guide of the ward in-charges. Data on practice of NP was collected using a checklist where in patient files were sampled. Results: Majority (78.3%) of the respondents reported they have a knowledge gap in NP, 81.2% felt NP is time consuming, 29% felt that NP contributes to patients’ wellness at times and 3% felt it does not contribute to patients’ wellness. Half (50%) of the unit in-charges reported that half of the nurses had a positive attitude towards utilizing NP. Most (72.5%) of the respondents reported the facility inadequately supports the implementation of the NP. From the in-patient files; incomplete or missing information, in regards to patient episodic assessment, and nursing care plans was revealed. Discussion: A knowledge gap in relation to utilization of NP and a negative attitude were noted. The practice on NP was wanting as most of the files did not have complete care plans and this therefore indicates that there might be a compromise in patient care. Respondents echoed that practice of NP was a challenge as a result of shortage of staff, lack of supplies as they are overworked and the NP paper work meant there was no time for patient care. Conclusions and Recommendation: The facility management needs to employ more nurses, provide material resources and ensure continuous education, workshops, seminars or updates on NP to support and enhance the implementation of NP.
Keywords:
Knowledge, Attitude, Practice, Nursing Process, Utilization
Cite this paper: Catherine Mwangi, Lucy W. Meng’anyi, Ruth G. Mbugua, Utilization of the Nursing Process among Nurses Working at a Level 5 Hospital, Kenya, International Journal of Nursing Science, Vol. 9 No. 1, 2019, pp. 1-11. doi: 10.5923/j.nursing.20190901.01.
1. Introduction
Nursing care has continued to evolve from the era of disease model to today’s scientific based care and holistic approach. Patients in the past were treated based on illness suffered without considering the psychological and social factors that always accompany physical illness. Nursing process application combines the art and science of nursing which has proved to be a valuable tool that has continued to revolutionize nursing practice as well as patient outcome globally. Nurse practitioners therefore must keep abreast with good scientific understanding of all the tasks done [1].The use of the nursing process in the clinical areas enhances high quality nursing care, improves health of patients and promotes nursing profession scientific discipline [2].Learning and using the nursing process are two different things with most of the nurses only practicing nursing process when they have one individual patient or a few patients but as the number increases the practice is compromised. A study conducted by Akbari and Shamsi (2011) shows that 50.6% subjects mentioned that they had cared for patients using the nursing process but many said they never learned it in the clinical areas correctly [3].Absence of an established knowledge base on nursing process by nurses has made nursing process acceptance low and its transition from theory to practice difficult at the clinical level [4]. A study conducted in the United States of America (USA) that assessed nurses’ attitude on the nursing process by using Dayton attitude scale revealed that participants were knowledgeable on nursing process and held positive attitude but it was associated with nurses with a high level of education that is nursing degree as opposed to those with low nursing qualifications [5].In a study conducted in a Brazilian teaching hospital on evaluation of nursing process practice 68 medical records were reviewed and the findings showed data collection of history and physical examination was most frequent on the day of admission. Other records had nursing interventions with no nursing diagnosis. The study showed failure in following of the nursing process steps and when they were applied there was no consistency [6].At Tabriz teaching hospital in Iran, a survey was done on knowledge and practice of nurses regarding nursing documentation. It showed that nursing records had insufficient information of the assessment data, planning, nursing intervention and evaluation [7].In Africa, many countries have adopted the nursing process approach in patient care but the problem lies in its utilization in the clinical settings. The extent of its implementations in the clinical settings has not been extensively studied and documented in many countries in Africa including Kenya. A study conducted in 4 African countries including Kenya in 2005 showed nurses in generally agree on benefits of nursing process although they don’t commonly use it in practice [8] .A study at Debre Markos Referral Hospital and Finote Selam District Hospital, northwest Ethiopia in 2013, on attitude and practices of nurses towards nursing process showed that out of the 124 respondents, 37.1% practice it well, 50% somewhat and 13% do not practice NP at all [9].Despite the training curricula for nurses and midwives incorporating the NP as a framework for nursing care in Kenya, nurses still find it difficult to practice NP hence this could be contributing to poor-quality of patient care [10].Hospitals also have problems that hinder full implementation of nursing process which includes excess work load on nurses, understaffing and lack of equipment. Yura and Walsh (1978) concluded that nursing process can only be effectively implemented when there is collaboration between hospital authority and nurses as it regards finances, equipment and personnel [11].The findings of a study in Ghana titled “Factors that influence the clinical utilization of the nursing process” at a hospital in Accra, Ghana concluded that although nurses had good theoretical knowledge, obstacles in implementing nursing process were due to inadequate staff especially and nurses having excess workload due to under staffing [12]. Nyatichi M., et al (2012) also revealed that, training, practical experience, adequate time, reference materials, administrative support, supplies and adequate staffing were found to be major factors influencing implementation of the NP in a hospital in Kenya [10]. Implementation of the NP has economic benefits to a country as it leads to increase in patients’ working time and decrease in the cost of health care as a result of patients’ reduced hospital stay which is a result of quality health care from nurses [11].
2. Main Body
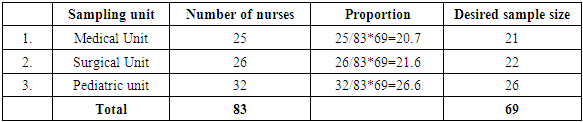
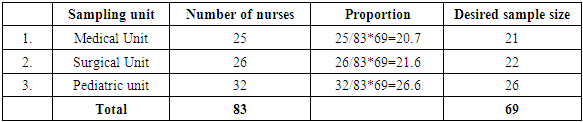
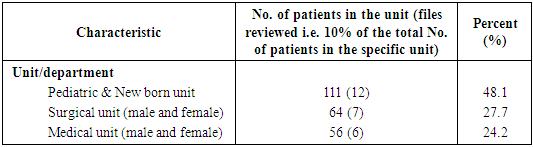
A descriptive cross sectional quantitative, qualitative study was conducted in the month of September 2017 where 69 nurses from the Medical, Surgical, Paediatric and New born units of Thika Level 5 Hospital in Kenya were recruited. Consent was sought from the respondents before recruitment. Approval to conduct the study was sort from Mount Kenya University Ethics and Research Committee, National Commission for Science, Technology & Innovation (NACOSTI) and Thika Level 5 Hospital Ethics Committee. A self-administered questionnaire and a checklist were used to collect quantitative data on knowledge, attitude, practice and hospital factors influence on utilization of nursing process. A key informant interview (KII) guide was used to collect qualitative data from the department nurse in-charges. To avoid missing questionnaires, the researchers requested the respondents to fill the questionnaires as they filled the checklist and conducted the interview with the in-charges. The checklist was used to record observations made from patient files to assess the implementation of nursing process. The researchers reviewed 10.8% of the files of total in-patients found in the three units at the time of the study.The tools were pre-tested for validity and reliability in the medical, surgical, and paediatric units in Gatundu Level 5 hospital. This was an ideal hospital for pretesting as the setup is almost similar to Thika Level 5 as the two hospitals are the same level. The sampling frame was all qualified nurses in medical, surgical paediatric and new born units whose total number at the time of the study was 83. The Cochran (1963:75) statistical formula for population studies was used to determine the sample size but since no proportions on KAP in nursing process had been documented in the county, the researchers used 50% (0.5) as the proportion in the study.The Fisher et.al. 1998 formula for social studies was further used to calculate the sample size as the study population was less than 10,000 which elicited a figure of 69 nurses from the respective departments. To avoid biasness a proportionate sample size was calculated from three units as shown in Table 1.Table 1. Proportionate sample per unit/ward
 |
| |
|
Thika Level 5 Hospital was purposefully sampled due to the hospital having a large number of nurses and patient population in the county. Medical, surgical, paediatric and new-born units were further purposefully sampled due to the critical role the nursing process plays in determining the patients’ outcome in these units. The researchers used the duty roster to know the number of nurses in each unit. The researchers then randomly sampled the respondents by writing Yes and No on pieces of paper which were equivalent to the number of nurses in the required sample size in each unit while the rest of the pieces were blank. The pieces were then shuffled and each nurse was requested to pick one. All the nurses who picked a piece with Yes on it were sampled to participate in the study. Any respondent who declined to participate in the study was replaced by any other qualified nurse on duty in the unit who agreed to participate in the study.The inclusion criteria was all the qualified nurses working in TL5H who were at their work stations in the medical, surgical, paediatric and new born units at the time of the study. The exclusion criteria was all nursing students on practical attachment, any nurse who was not working in the medical, surgical, paediatric and new born units and any nurse who declined to participate in the study. Nurses not on duty at the time of the study were also excluded from the study.The independent variables were; nurses knowledge on the NP, attitude of nurses towards NP, and hospital factors that affect utilization of the nursing process while the dependent variable was the utilization of nursing process. Quantitative and qualitative data was analysed using SPSS version 20.0. Qualitative data was further thematically analysed and triangulated with the study variables. Descriptive analysis was done and analysed data was presented in frequencies, proportions, percentages and measures of central tendency.
3. Results
3.1. Response Rate
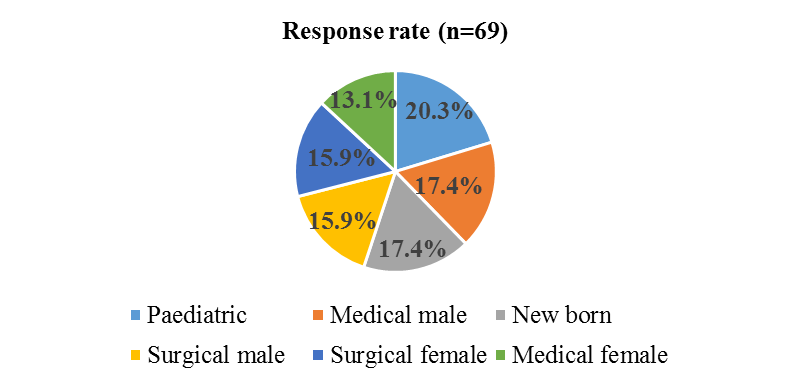
The response rate for the study was 100% (69), six (6) Key Informant Interviews with unit in-charges conducted and 25 (10.8%) of the in-patient files reviewed. The paediatric unit had the highest (20.3%) number of respondents, while the female medical unit had the least (13.1%) (Figure 1). The response rate was per the proportion of staff calculated in the sample size of the units (Table 1).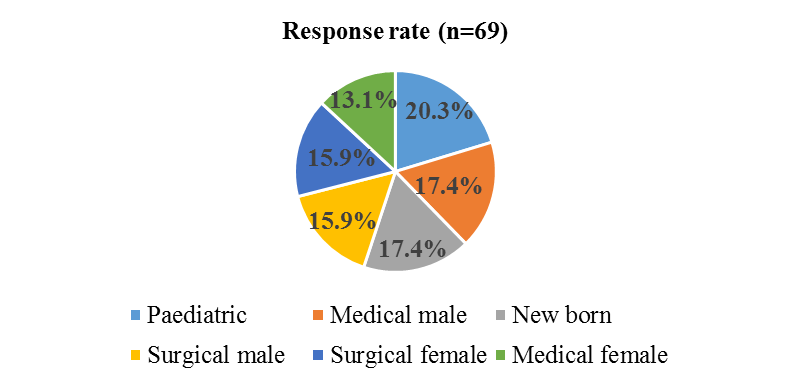 | Figure 1. Response rate |
3.2. Demographic Characteristics of the Respondents
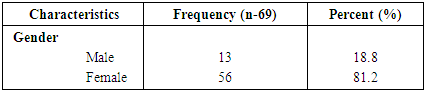
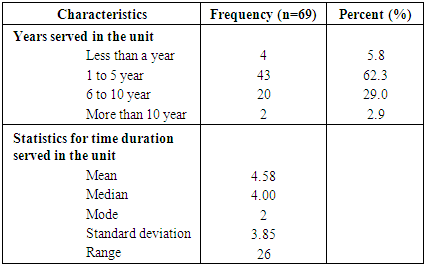
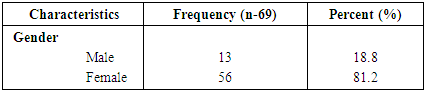
Majority (81.2%) of the respondents were female which is a representation of the large number of female staff in the nursing profession. This is proportionate with the facility staff population since majority of nursing staff are female (Table 2).Table 2. Gender of the respondents
 |
| |
|
3.3. Respondents’ Level of Education
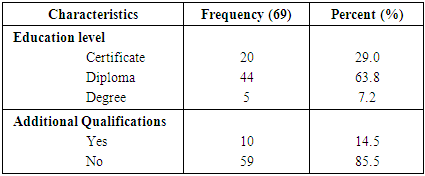
Most (64%) of the respondents had attained a diploma in nursing while 29% of the respondents had a certificate level of education in nursing and 7% degree education level. Only 14.5% of the respondents had attained additional qualification which ranged from counselling, Maternal Child Health / Family Planning (MCH/FP), Midwifery, Neonatal Nursing, Reproductive Health (RH) and Paediatric Nursing (Table 3).Table 3. Education Level of Respondents
 |
| |
|
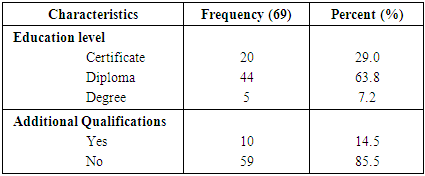
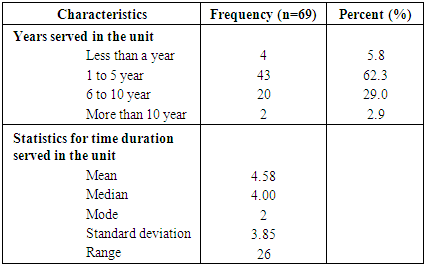
3.4. Years Served in the Unit by the Respondents
Most (62.3%) of the respondents had worked in the current station for 1 to 5 years while 2.9% had stayed in the department for more than 10 years. The mean duration of service in a unit was 4.58 years with a standard deviation ± 3.85 years. The longest serving nurse in a unit had served for 26 years, while those who had served for the shortest period was less than a year (Table 4).Table 4. Number of Years Served in the Unit
 |
| |
|
3.5. Respondents’ Description of the Nursing Process
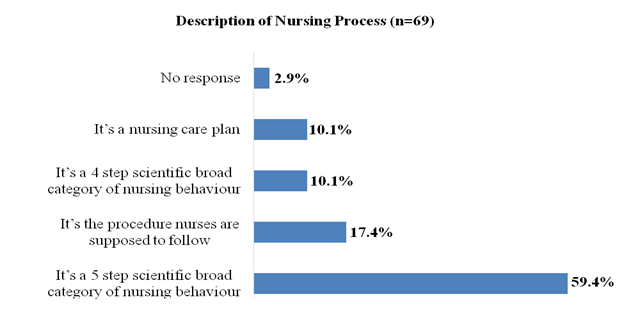
Over half (59.4%) of the respondents described Nursing Process (NP) as a 5 step scientific broad category of nursing behaviour. Ten percent (10.1%) described it as a nursing care plan, and a four step scientific broad category of nursing behaviour. A small (2.9%) proportion of the respondents indicated no response to the question (Figure 2).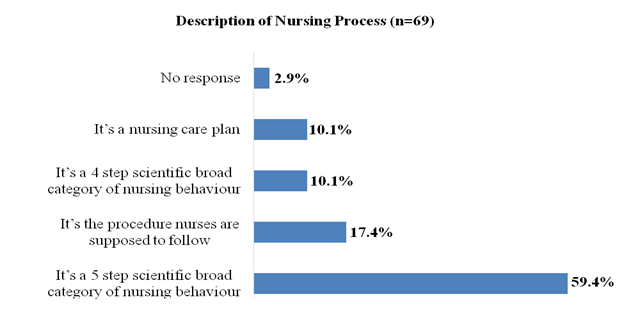 | Figure 2. Respondents’ Description of the Nursing Process |
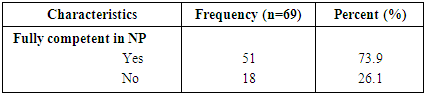
3.6. Competence in Implementing the Nursing Process
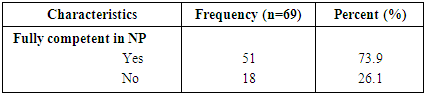
Majority (73.9%) indicated that they are fully competent in implementing the NP while the rest reported they were not fully competent in the process (Table 5).Table 5. Respondents’ Competence in Implementing the Nursing Process
 |
| |
|
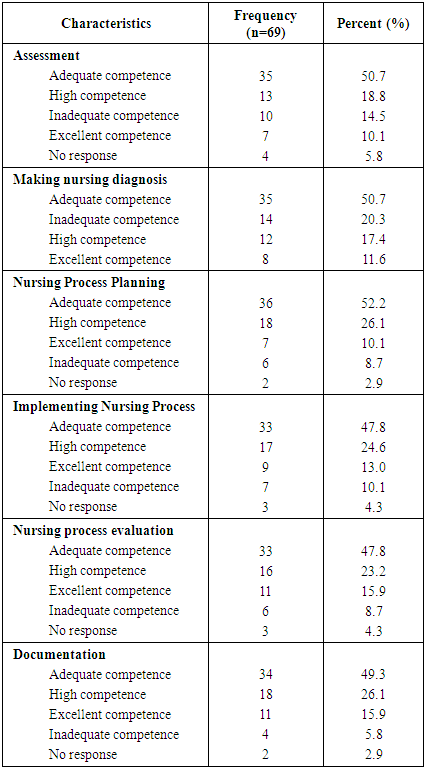
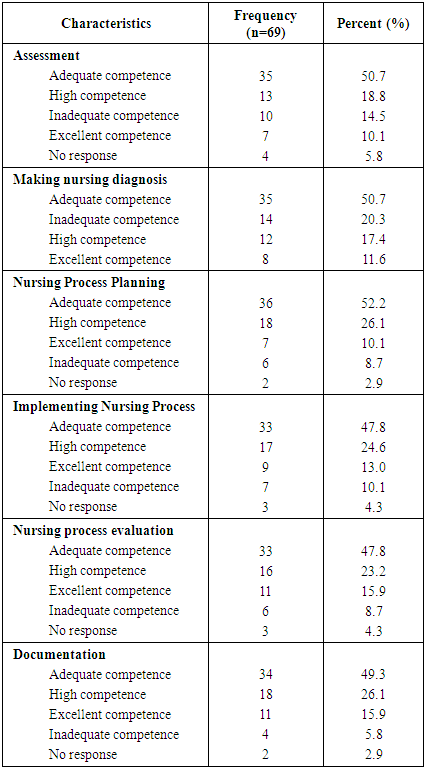
3.7. Respondents’ Self-rating of the Nursing Process
Half (50.7%) of the respondents felt they had adequate competence to undertake patient assessment, while 14.5% reported inadequate competency. Only 10.1% of the respondents reported excellent competence in patient assessment. On nursing diagnosis, half (50.7%) of the respondents reported adequate competence, while 20.3% reported inadequate competence. Self-rating on planning revealed that, slightly over half (52.2%) of the respondents had adequate competence with 8.7% of the respondents reporting inadequate competency. Less than half (47.8%), of the respondents reported adequate competence in implementing the Nursing Process, with 13.0% reporting excellent competence. However, 10.1% of the respondents reported inadequate competence in implementing the nursing process. The study further revealed that, less than half (47.8%) of the respondents reported adequate competence in nursing process evaluation. Less than a quarter (23.2%) reported high competence while 8.7% reported inadequate competence. Self-rating on documentation revealed 49.3% of the respondents had adequate competence, 26.1% had high competence and 15.9% had excellent competence. However, 5.8% of the respondents had inadequate competence for documentation of the nursing process.In all the areas assessed, the self-rating revealed a proportion of inadequate competence among the respondents. Even though these proportions were not huge, this could bring significant impact to the Nursing Process contributing to poor patient management and outcomes (Table 6).Table 6. Respondents’ nursing process Self-rating for competency level
 |
| |
|
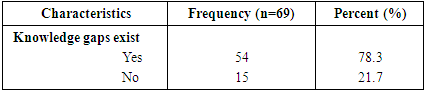
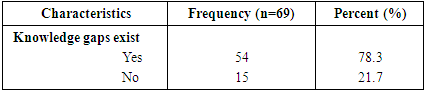
3.8. Knowledge Gap in Nursing Process
Majority (78.3%) of the respondents reported they have a knowledge gap in Nursing Process, while the rest reported that they did not have a knowledge gap. The existence of NP knowledge gap was identified as a hindrance to effective and adequate implementing the NP among the nurses in the course of their daily duties in the hospital (Table 7).Table 7. Existence of Nursing Process knowledge gaps
 |
| |
|
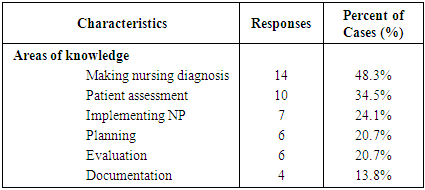
3.9. Identified Knowledge Gaps in the Nursing Process
Almost half (48.3%) reported a gap in making nursing diagnosis while over a third (34.5%) had a knowledge gap in patient assessment. Slightly less than a quarter (24.1%) reported a gap in implementing the Nursing Process, while 20.7% of the respondents reported a knowledge gap in planning and evaluation. Knowledge gap in documentation was reported by 13.8% of the respondents (Table 8).Table 8. Identified knowledge gaps (multiple responses – percent more than 100%)
 |
| |
|
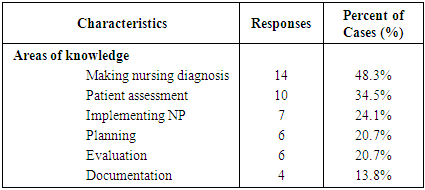
3.10. Recommendation to Bridge the Knowledge Gap in the Nursing Process
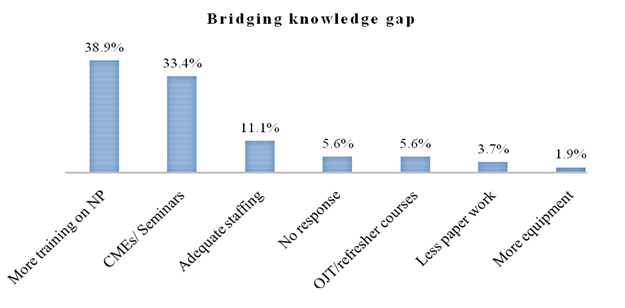
More than a third (38.9%) of the respondents with knowledge gap recommended more training while a third (33.4%) recommended frequent Continuous Medical Education (CME). Five (5.6%) recommended On Job Training (OJT) and refresher courses (Figure 3).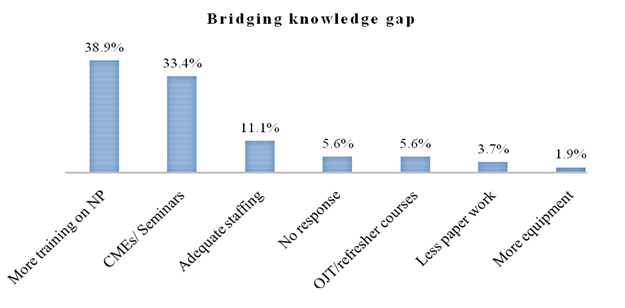 | Figure 3. Recommendation to Bridge the Knowledge Gap |
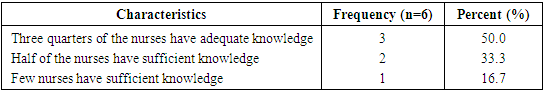
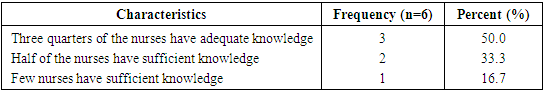
3.11. Unit In-Charges Assessment of Knowledge Gap
Key interviews with the unit in-charges revealed that half (50.0%) of the in-charges indicated that three quarters of the nurses have adequate knowledge, while a third (33.3%) of the in-charges reported that, a half of the nurses in the units have sufficient knowledge on Nursing Process (Table 9).Table 9. Nursing Process knowledge assessment by unit in-charges
 |
| |
|
3.12. Attitude on Nursing Process
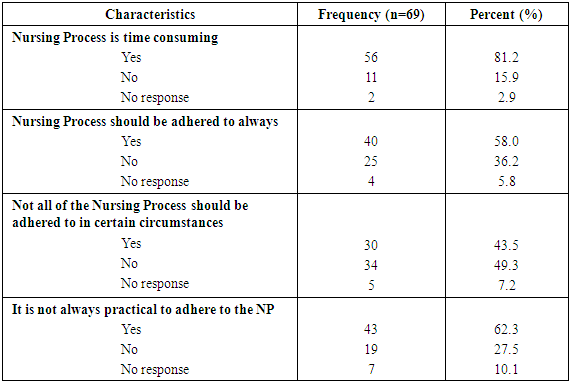
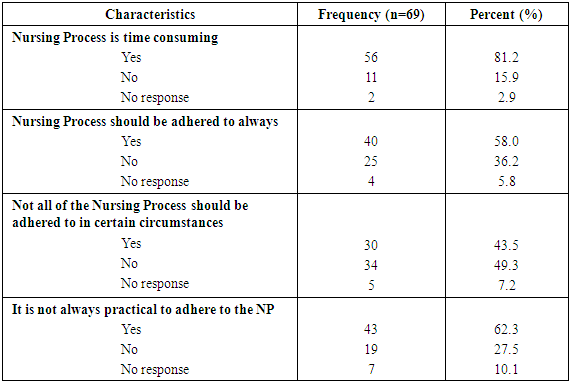
3.12.1. Nursing Process is Time Consuming
Majority (81.2%) of the respondents felt that Nursing Process is time consuming while 15.9% were of a contrary opinion. Over a half (58.0%) felt that Nursing Process should always be adhered to though, 36.2% felt it should not be always adhered to. Nearly half (49.3%) of the respondents held the opinion that NP should be adhered to irrespective of the circumstances, while 43.5% of the respondent held a contrary opinion. However, 62.3% of the respondents felt that it is not always practical to adhere to the NP. A small proportion of the respondents gave no responses on the attitude areas assessed by the researchers as indicated in the table (Table 10).Table 10. Nursing Process is time consuming
 |
| |
|
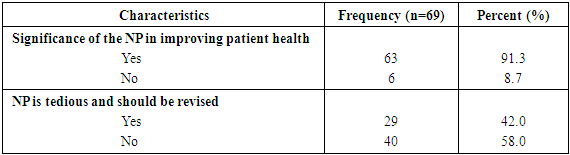
3.13. Respondents’ Opinion of Significance of Nursing Process in Patient Outcomes
Majority (91.3%) of the respondents reported that Nursing Process is significant in improving the health of the patient. Over half (58.0%) of the respondents felt that NP is not tedious and should not be revised, while the rest (Majority (81.2%) of the respondents felt that Nursing Process is time consuming while 15.9% were of a contrary opinion (Table 11).Table 11. Significance of the Nursing Process in improving patient health
 |
| |
|
3.14. Respondents’ Opinion of the Nursing Process Contribution to Patient Wellness
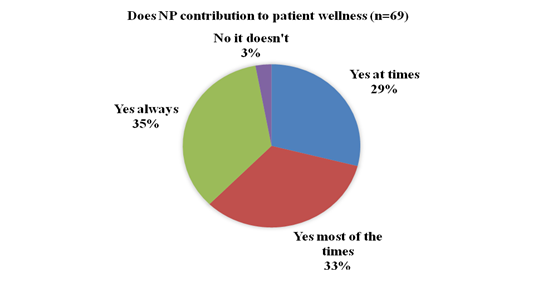
Over a third (35.0%) of the respondents reported that NP always contributes to the wellness of the patient, while 29.0% held the opinion that, NP contributed to patient wellness at times. A small proportion (3%) reported NP does not contribute to patients’ wellness (Figure 4).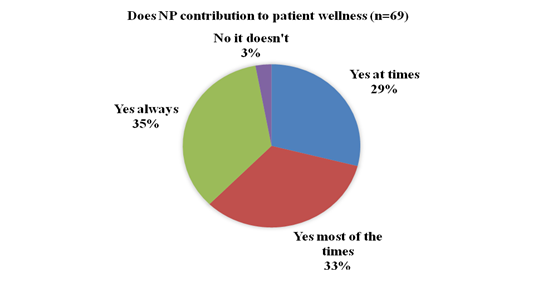 | Figure 4. Nurses opinion on NP contribution to patient wellness |
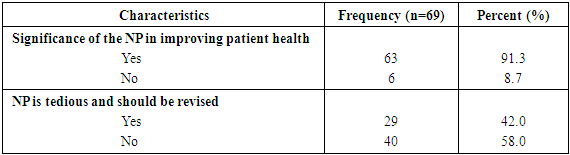
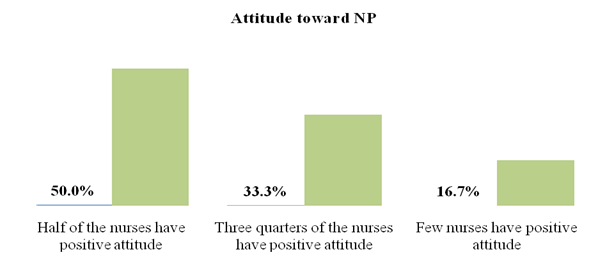
3.15. Opinion of Unit In-Charges on Nurses’ Attitude towards Nursing Process
Key informant interviews revealed that, half (50.0%) of the unit in-charges were of the opinion that half of the nurses have a positive attitude toward implementing the NP. However, a third (33.3%) of the in-charges indicated that, three quarters of the nurses have a positive attitude and 16.7% were of the opinion that few nurses have positive attitude towards implementing the NP (Figure 5).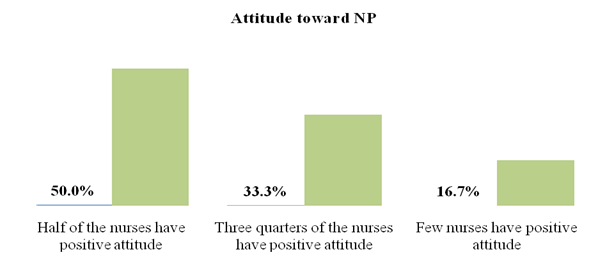 | Figure 5. Opinion of Unit In-Charges on Nurses’ Attitude towards NP |
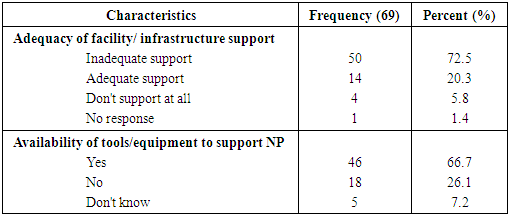
3.16. Hospital Factors
3.16.1. Facility, Tools and Equipment influence on Utilization of the Nursing Process
Most (72.5%) of the respondents reported the facility inadequately supports the implementation of the NP. Only 20.3% of the respondent felt that the facility support was adequate, while 5.8% reported the facilities or infrastructure do not support NP at all. Two third (66.7%) of the respondents reported missing facilities/ tools to support NP implementation, with a small (7.2%) proportion of the respondents were not aware whether there were missing tools or equipment to support NP implementation (Table 12).Table 12. Facility/ infrastructure support to NP utilization
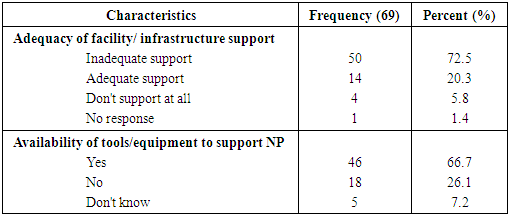 |
| |
|
3.16.2. Facility Management and In-Charges Support on NP
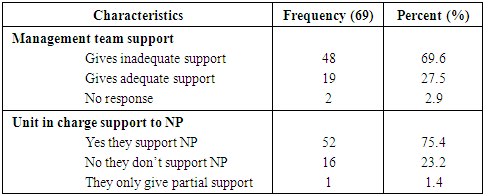
Over two thirds (69.6%) of the respondents reported that the management gives inadequate support for the implementation of NP, while 27.5% reported adequate support is given by the management. Most (75.4%) respondents indicated that, the unit/ department in-charges support NP. One respondent reported that the in-charges only give partial support, while the rest of the respondents reported in-charges do not support the implementation of the NP (Table 13).Table 13. Management and in-charges support to NP utilization
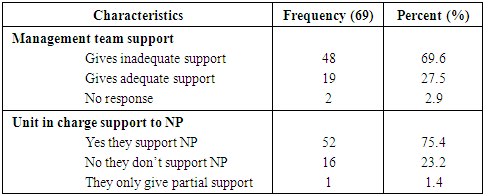 |
| |
|
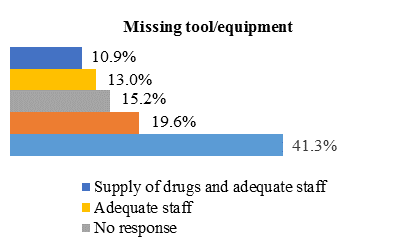
3.16.3. Missing Tools/ Equipment for Supporting NP
Less than half (41.3%) of the respondents reported adequate tools and equipment to support NP were missing, while 19.6% mentioned stationeries and equipment as missing, and 10.9% mentioned drugs supplies and adequate staff as missing (Figure 6).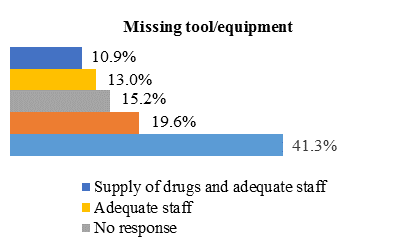 | Figure 6. Missing Tools/ Equipment for Supporting NP |
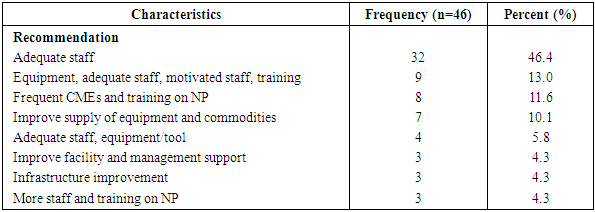
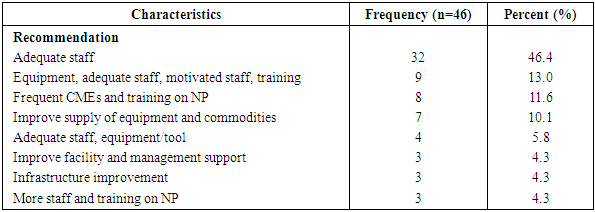
3.17. Recommendation on Improvement of Utilization of the Nursing Process
On improvement of utilization of NP, 46.4% of the respondents recommended deployment of adequate staff to the units/departments. Eleven percent (11.6%) of the respondents recommended frequent Continuous Medical Education (CME) and training on NP, while 4.3% recommended the improvement of facility and management support (Table 14).Table 14. Recommendation on improvement of Utilization of the Nursing Process
 |
| |
|
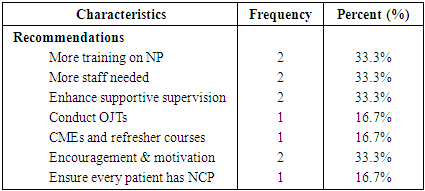
3.18. Unit In-Charges Recommendations on Improvement of Utilization of the Nursing Process
A third (33.3%) of the unit in-charges recommended more training on NP, more staff, enhancement of supportive supervision and staff motivation among the nurses in order to improve utilization of NP in the facility (Table 15).Table 15. Unit in- charges Recommendations on Improvement of Utilization of the Nursing Process (multiple responses - percent more than 100%)
 |
| |
|
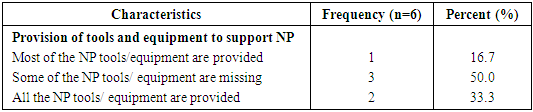
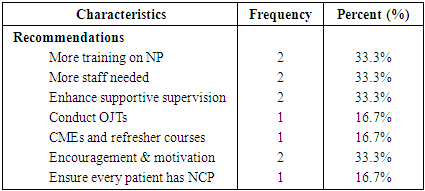
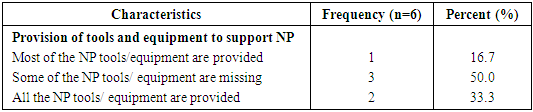
3.19. Unit In-Charges Responses on Tools and Equipment Provision in the Facility for Support of NP
Half (50.0%) of the unit in-charges reported that some NP tools and equipment were missing, while 16.7% reported most of the tools and equipment are provided. Only a third (33.3%) reported that, all the NP tools and equipment are provided to support implementation of NP in the facility (Table 16).Table 16. Unit in-charges responses on tools and equipment provision in the facility for support of NP
 |
| |
|
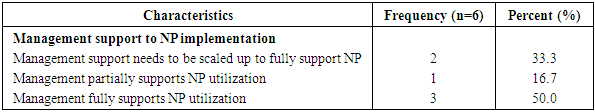
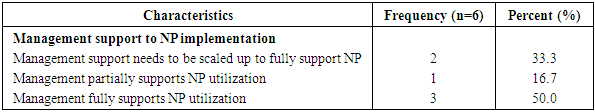
3.20. Description of Management Support in the Implementation of the Nursing Process by Unit In-Charges
Key interviews with the in-charges revealed that, half (50.0%) of them indicated management fully support the implementation of NP. However a third (33.3%) reported that management support needs to be scaled up to fully support implementation of NP in the facility (Table 17).Table 17. Description of management support in the implementation of the Nursing Process by unit in-charges
 |
| |
|
3.21. Practice of the Nursing Process by the Respondents’
Practice on NP was assessed using a checklist where 25 in patient files were randomly picked and reviewed for NP completeness and adequacy of data and information provided. The findings were triangulated with the respondents’ responses on how identified factors hindered their utilization of the NP.
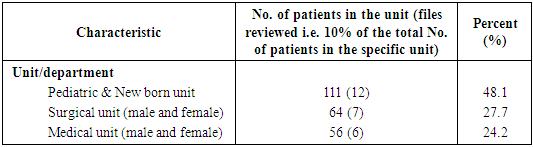
3.21.1. Proportion of Reviewed Files per Unit/ Department
A total of 25(10.8%) of 231 in-patient files in all the units were reviewed. The researchers reviewed 12 from the paediatric and newborn units, 7 files from the surgical (male and female) and 6 files from, the medical (male and female) units (Table 18).Table 18. Proportion of reviewed file per unit
 |
| |
|
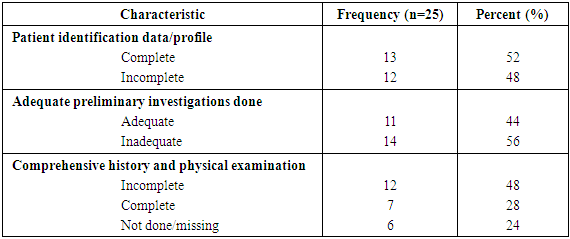
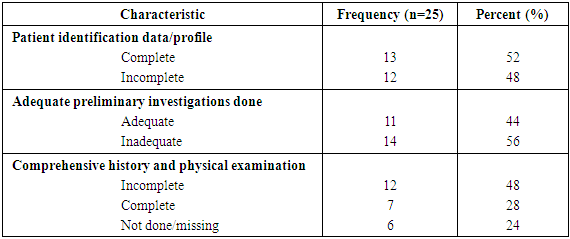
3.21.2. Completeness and Adequacy of Data and Information on NP
Assessment of Patients’ files on adequate patient identification data or patient profile, preliminary investigation, comprehensive history and physical examination revealed that, 52% of the files had complete patient identification data. Over half (56%) of the files had inadequate preliminary investigations while 48% had incomplete comprehensive history and physical examination (Table 19).Table 19. Completeness and adequacy of data and information on NP
 |
| |
|
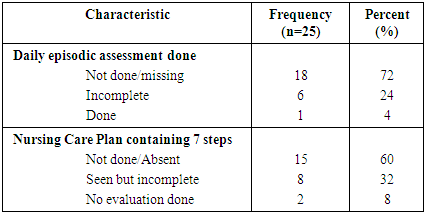
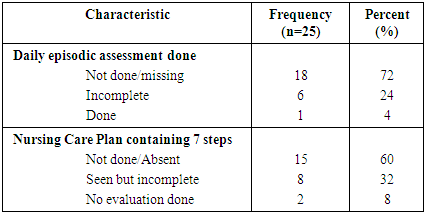
3.21.3. Daily Episodic Assessment and Nursing Care Plan (NCP) Revision
Review of the patients’ files led to the conclusion that majority (72%) of the files lacked or missed daily episodic patient assessment and only 1 file had complete daily episodic assessment done. Out of the 25 files reviewed 60% did not have a Nursing Care Plan (NCP) and 32% contained incomplete NCPs (Table 20).Table 20. Daily episodic assessment and Nursing Care Plan revision
 |
| |
|
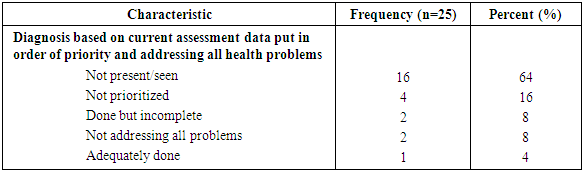
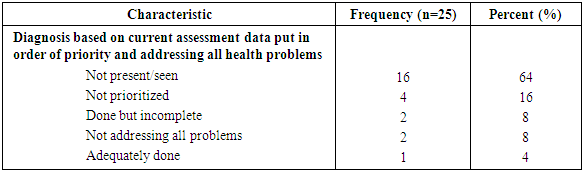
3.21.4. Nursing Diagnosis based on Current Assessment Data which is prioritized and Addresses All Health Problems
Reviewed files indicated that, 64% of the files had no diagnosis based on the assessment data to prioritize and address all noted health problems. In 16% of the files nursing diagnoses were not prioritized and 8% were incomplete. Only 4% (1) of the files had adequate diagnosis based on data, prioritized and had a plan to address all identified health problems (Table 21).Table 21. Nursing Diagnosis based on current assessment data which is prioritized and addresses all health problems
 |
| |
|
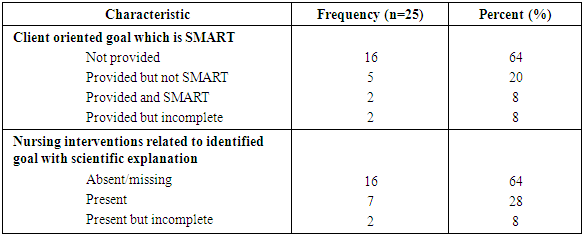
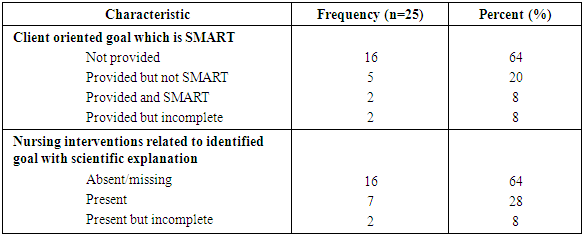
3.21.5. Client Oriented Goal Relevant to Nursing Diagnosis that is Specific, Measurable, Achievable, Realistic & Time Bound (SMART) and Nursing Interventions Provided
Review of the files indicated that 64% of the files did not have goals while 20% of the files had goals but not SMART and 8% had incomplete goals. Only 8% (2) of the files had complete and SMART client oriented goals. Further review indicated 64% of the files missed nursing interventions related to the goal and scientific explanation. Slightly over a quarter had the interventions though incomplete (Table 22).Table 22. Client oriented goal relevant to nursing diagnosis that is Specific, Measurable, Achievable, Realistic & Time bound (SMART) and nursing interventions provided
 |
| |
|
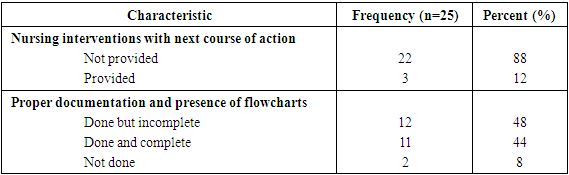
3.21.6. Evaluation of Nursing Interventions Indicating Whether the Goal has been Met or not and Proper Documentation
The study revealed that, only 12% of the files had a complete evaluation of nursing interventions indicating whether the goal has been met or not and the next course of action. Forty four percent (44%) of the reviewed files were found to have proper documentation and presence of relevant flowcharts. Most, (48%) of the files had incomplete documentation and flowcharts as required in the NP (Table 23).Table 23. Evaluation of nursing interventions indicating whether the goal has been met or not and proper documentation
 |
| |
|
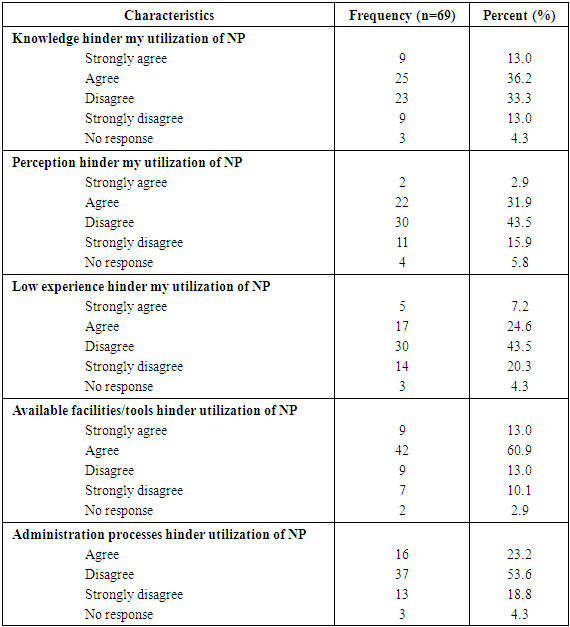
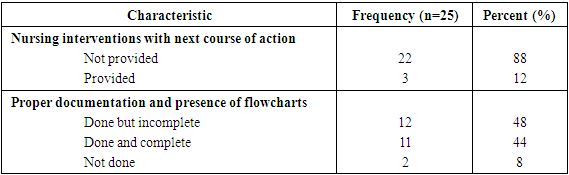
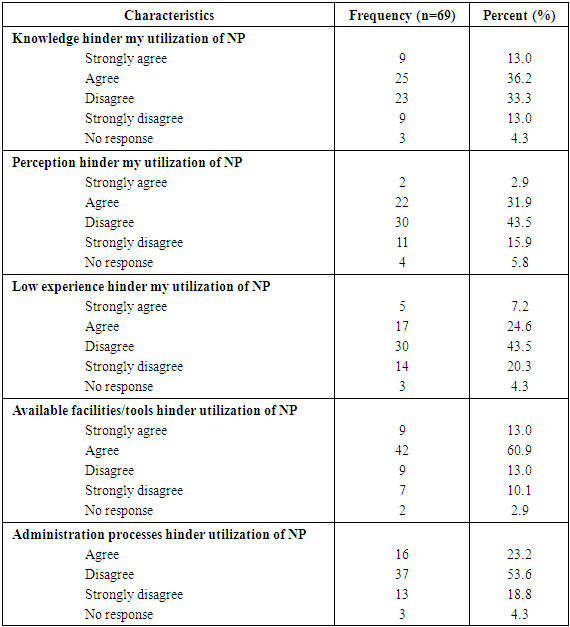
3.22. Level of Respondent Agreement with Factors that May Hinder Utilization of NP
The respondents’ level of agreement on various factors that could hinder their utilization of NP was sought, where over a third (36.2%) agreed that, knowledge hindered their implementation of NP. Less than a third (31.9%) agreed perception hindered them from implementing NP, while 24.6% agreed low experience was a hindrance. Most (60.9%) agreed available facilities/ tools hindered their implementation of NP. Only 23.2% agreed administration processes hindered their NP implementation (Table 24).Table 24. Level of respondent agreement with factors that may hinder utilization of NP
 |
| |
|
4. Discussion
The findings of the study revealed an average level of knowledge on NP among the nurses in Thika Level 5 Hospital. It was also revealed that over half of the nurses reported being fully competent in the NP. The findings contradict those of a study conducted in Mekelle Zone Hospitals, Northern Ethiopia which revealed that 90% of the respondents had poor knowledge of the NP [13].A self-assessment on key NP areas namely assessment, diagnosis, planning, implementation, evaluation and documentation revealed various levels of competencies. Generally the study revealed an average level of adequacy of these assessed areas, since the respondents reported adequate competency in three of the areas (assessment, diagnosis and planning). A small proportion of the respondents reported excellent competency in all these areas. However, adequate competency on NP implementation and documentation was reported by less than half of the respondents. These findings concur with Beaupre (1988) report that noted that nurses have deficiencies in knowledge regarding nursing process owing to rapid expansion of nursing knowledge and accountability [14]. This finding was further supported by the unit in-charges, half of whom reported that only three quarters of the nurses had adequate knowledge on NP. Some of the nurses also strongly agreed that knowledge hindered their implementation of the NP.Most of the nurses were of the opinion that NP is time consuming, and not all steps of NP should be adhered to under certain circumstances. Consequently, most of the respondents felt that it is always not practical to adhere to the NP. These findings are consistent with a study by Hagos et al., 2014 where the researchers found that in Mekelle Zone Hospitals, Northern Ethiopia not all the steps of the nursing process were adhered to by the nurses [13]. Half of the unit in-charges indicated only half (50%) of the nurses had positive attitude towards the NP. Even though majority of the respondents were of the opinion that, NP is significant in improving patient health, only slightly over a third reported NP always contributed to patients’ wellness. The rest reported NP contributed to patient wellness either most of the times or at times, while there were those who felt it does not contribute to patient wellness at all. These findings are in support of the Bowman (1983) report which indicated that the problems experienced in implementing the NP are caused by the nurses’ attitude towards it [15]. Carlson (1972) observed that, qualified nurses may fail to implement NP because they viewed it more as a student learning tool meant for examination purposes; hence acceptance of NP needs an in-depth attitude change than mere practice. The study further showed a comparatively large number of respondents who agreed with the fact that, their perception was hindering the utilization of NP [16].American Nursing Association (2009) postulates that NP is an important framework that needs to be practiced by nurses in providing high quality standard of care in all hospital setting [1]. The researchers used a checklist to assess the practice of the NP within the facility by evaluating the files of in-patients hospitalized at the time of the study. The assessment concentrated on completeness of patient identification or profile data, adequacy of preliminary investigations, undertaking of daily episodic assessment, presence of nursing care plans containing the 7 steps, diagnosis based on current assessment data to prioritize and address all health problems, client oriented goal relevant to SMART nursing diagnosis, interventions with next course of action and proper documentation. The findings of the reviewed in-patient files revealed incomplete, inadequate and or missing information, in regards to patient episodic assessment, and nursing care plans. The nursing care plans had incomplete or missing client oriented goals which were not SMART, incomplete or missing nursing diagnoses and interventions which also lacked scientific explanations. Most of the files lacked the nursing interventions with next course of action and proper documentation and presence of flowcharts. The study therefore revealed a low level of implementation of NP despite the basic nursing training which incorporates the nursing process. The failure of the nurses in the institution to effectively implement the nursing process concurs with a report by Mangare et al., (2012) which indicated that, though the training curricula for nurses in Kenya has incorporated the NP as a framework for nursing care, nurses find it difficult to practice it contributing to poor-quality of healthcare to patients [10]. Mahmoud and Bayoumy (2014) also argued that NP is used in clinical practice to provide patients with quality individualized plan of care, hence the lack of its application can reduce the quality of healthcare [17]. Though majority of the respondents reported experience did not hinder their utilization of NP, a good number of the respondent held contrary views about it.The researchers found out that most respondents reported that the facility management team inadequately supported implementation of NP in the hospital. However, the unit in-charges were found to support nurses in implementation of the NP. Half of the unit in-charges indicated that some tools or equipment for NP implementation were missing from their units. A large proportion of the respondents also reported that adequate tools and equipment to support NP were missing from the hospital. Majority of the respondents concurred with the unit in-charges that inadequate facility support, lack of sufficient infrastructure in regards to missing tools or equipment hindered implementation of NP in the hospital. The respondents suggested that employment of more staff, provision of necessary tools or equipment, staff training and motivation could improve NP utilization in the hospital. This is in line with findings by Yura and Walsh (1988) who identified hospital factors as a hindrance to full implementation of NP among nurses, which included excess workload and lack of equipment [18]. This view was further reinforced by Abebe et.al, (2014) who stated that disjointed care arises as a result of shortage of equipment and instruments in the hospital [9].A proportion of the respondents agreed that available tools and facilities hindered their utilization of NP. However they disagreed with the statement that the administration process was a hindrance to implementation of NP. The finding concurs with Laryea (1994) study on problems that prevent utilization of NP which indicated that, nurses complained of lack of power and equipment and lack of motivation by hospital management affect implementation of NP [19].In general, the study findings on knowledge, attitude, practice and hospital factors at Thika Level 5 Hospital concur with a study conducted in Naivasha hospital by Mangare. et.al (2012) which revealed that, experience, adequate staffing, administrative support and supplies were found to be major factors influencing the implementation of NP in the hospital [10].
5. Conclusions
Effective and efficient implementation of the nursing process directly contributes to the quality of healthcare and the patients’ health outcomes. From the findings in this study it can be concluded that there is a challenge in utilization of the nursing process as a result of inadequate knowledge, attitude and practice issues. Resources in terms of human and supplies needed in implementation of the nursing process were reported to be inadequate. The facility management therefore needs to provide all the necessary human and material resources to support and enhance the implementation of nursing process in the facility.
ACKNOWLEDGEMENTS
The authors give special thanks to the management of Thika Level 5 Hospital, the nurses in the Medical, Surgical, Pediatric departments and Newborn unit who participated in this study. The authors also appreciate Mt. Kenya University Research Department for the support they provided.
References
| [1] | American Nurses Association (2009). The Nursing Process: A Common Thread among all Nurses. From http://www.nursingworld.org. Accessed online on 27/06/2017. |
| [2] | Habermann, M. and L.R. Uys, The nursing process: a global concept. 2006: Elsevier Health Sciences. |
| [3] | Akbari. M, S., A. , A survey on nursing process barriers from the nurses’ view of intensive care units. Iran J Crit Care Nurs, 2011. 4: p. 181-6. |
| [4] | Jansson, I., Bahtsevani, C., Pilhammar-Andersson, E., & Forsberg, A. (2010). Factors and Conditions that Influence the Implementation of Standardized Nursing Care Plans. The open nursing journal, 4, 25-34. |
| [5] | Martin, P.A., et al., Nurses' attitudes toward nursing process as measured by the Dayton Attitude Scale. The Journal of Continuing Education in Nursing, 1994. 25(1): p. 35-40. |
| [6] | de Moraes Lopes, M.H.B., et al., Evaluation of the nursing process used at a Brazilian teaching hospital. International Journal of Nursing Terminologies and Classifications, 2010. 21(3): p. 116-123. |
| [7] | Jasemi, M., Zamanzadeh, V., Rahmani, A., Mohajjel, A. & Alsadathoseini, F., Knowledge and practice of Tabriz teaching hospitals’ nurses regarding nursing documentation. Thrita Journal of Medical Sciences, 2012. 1(4): p. 133-8. |
| [8] | Sabona, E., E., Irinoye, O., Kamazi, D., Uys, L., Ofi, B. & Cassimjee, R.., The perception on, and use of, the nursing process in four African Countries. Afr J Nurs Midwifery, 2005. 6(1): p. 67-77. |
| [9] | Abebe, N., H. Abera, and M. Ayana, The implementation of nursing process and associated factors among nurses working in Debremarkos and Finoteselam Hospitals, Northwest Ethiopia, 2013. J Nurs Care, 2014. 2014: p. 4-7. |
| [10] | Mangare, L.N., L. N., Omondi, L., Ayieko, A., Wakasiaka, S., Omoni, G. & Wamalwa, D.., Factors influencing implementation of the nursing process in Naivasha District Hospital, Kenya. African Journal of Midwifery and Women's Health, 2016. 10(2): p. 67-71. |
| [11] | Miskir, Y. and S. Emishaw, Determinants of Nursing Process Implementation in North East Ethiopia: Cross-Sectional Study. Nursing research and practice, 2018. 2018. |
| [12] | Agyeman-Yeboah, J., K.A. Korsah, and J. Okrah, Factors that influence the clinical utilization of the nursing process at a hospital in Accra, Ghana. BMC Nursing, 2017. 16(1): p. 30. |
| [13] | Hagos, F., Alemseged, F., Balcha, F., Berhe, S. & Aregay, A., Application of nursing process and its affecting factors among nurses working in mekelle zone hospitals, Northern Ethiopia. Nursing research and practice, 2014. 2014. |
| [14] | Beaupre, B.A., An administrative marketing strategy: a different perspective on the nursing process. The Journal of nursing administration, 1988. 18(11): p. 37-41. |
| [15] | Bowman, G.S., D.R. Thompson, and T.W. Sutton, Nurses' attitudes towards the nursing process. Journal of Advanced Nursing, 1983. 8(2): p. 125-129. |
| [16] | Carlson, S., A practical approach to the nursing process. The American journal of nursing, 1972: p. 1589-1591. |
| [17] | Mahmoud, M.H. and H.M. Bayoumy, Barriers And Facilitators For Execution Of Nursing Process From Nurses'perspective. International Journal of Advanced Research, 2014. 2(2): p. 300-315. |
| [18] | Yura, H. and M.B. Walsh, The Nursing Process: Assessing. Planning, Implementing, Evaluating. (5th ed) Appleton & Lange, New York, 1988. |
| [19] | Laryea, J., Barriers to the implementation of the nursing process. West Afr J Nurs, 1994. 5(1): p. 10-7. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML