-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2018; 8(5): 77-82
doi:10.5923/j.nursing.20180805.01

Observed Utilization of the Nursing Process among Nurses in Selected Public Health Care Facilities in Kenya
Bernard W. Mbithi, Catherine S. Mwenda, Jane Karonjo
School of Nursing, Mount Kenya University, Thika, Kenya
Correspondence to: Bernard W. Mbithi, School of Nursing, Mount Kenya University, Thika, Kenya.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Nursing process is a systematic rational method which the nurse utilizes to plan and provide individualized care to clients. However despite efforts by various health care facilities to promote the nurses’ practice on nursing process, its utilization is still poor. Therefore, this study was undertaken to determine the utilization of nursing process among nurses in selected health care facilities in Kenya. This study was conducted among 249 nurses from five selected health care facilities in Kenya. The nurses were observed as they provided nursing care to patients, with observation checklists being used to enter the collected data. The study results showed that only about 29% (71) of the respondents were able to carry out their procedures and document according to the steps of nursing process. In conclusion utilization of nursing process among the respondents was poor. This is a situation which called for further measures to be instituted to promote utilization of the nursing process in the provision of nursing care.
Keywords: Nursing process, Utilization, Nursing care, Health care facilities, Kenya
Cite this paper: Bernard W. Mbithi, Catherine S. Mwenda, Jane Karonjo, Observed Utilization of the Nursing Process among Nurses in Selected Public Health Care Facilities in Kenya, International Journal of Nursing Science, Vol. 8 No. 5, 2018, pp. 77-82. doi: 10.5923/j.nursing.20180805.01.
Article Outline
1. Introduction
- Nursing process is a systematic rational method which the nurse utilizes to plan and provide individualized care to clients [1]. Nursing process and standardized nursing terminologies are essential elements to the structuring of nursing documentation in daily nursing information management [2]. The process is divided into five distinct steps which emphasize on the essential activities that must be taken to address client’s nursing diagnoses and manage any collaborative problems or complications [3]. The five steps include assessment, nursing diagnosis, planning, implementation and evaluation [4]. These steps are aimed at achieving the ultimate goal of nursing where the nurse strives to promote, maintain, rehabilitate or assist clients to achieve a peaceful death and to enable the family or the community to manage their own health care to the best of their ability [5]. Assessment is the initial step of the process in which case the nurse elicits as much information as possible from the client through verbal communication, physical examination, performing diagnostic tests and also from significant others [6]. The acquired data is validated, documented and used to derive the appropriate nursing diagnoses, forming the second step of the nursing process. Nursing diagnosis is a clinical judgment about an individual, family or community‘s responses to actual and potential health problems/life processes, that nurses can legally identify and for which they can prescribe the primary interventions for treatment and prevention [7]. Planning of the nursing care interventions forms the third step of nursing process, whereby the nurse organizes the nursing diagnoses according to priorities and makes a nursing care plan. In the care plan, the nurse develops expected care outcomes and nursing interventions [8]. Implementation of the nursing care plan forms the fourth step of nursing process, whereby the nursing care interventions are implemented to alleviate the client’s [8]. Once the nursing care interventions have been implemented, the nurse evaluates their effectives (the fifth step of nursing process) to ensure that the expected outcomes have been achieved. However, if the goals of the interventions are not realized, the nurse carries out further assessment on the client, hence repeating the process again [1]. Utilization of the various steps of nursing process results in the formation of a strong nurse – patient relationship. This will promote the patient’s compliance to the treatment regime, hence good care outcome [9]. However, despite these universal benefits of the nursing process, its utilization has remained minimal in most of the health care facilities in Kenya.Poor utilization of the nursing process may lead to poor quality of patient care and vice-versa. However, nurses’ ability to utilize nursing process may be affected by many factors as demonstrated by various studies identified in the literature. For example, a cross-sectional retrospective study carried out to review 302 records for adult patients admitted to surgical, clinical and intensive care unit in a hospital in Porto Alegres showed that deficiency in data collection for nursing records and absence of the nursing diagnosis step were the major findings in this study. Data collection and formulation of nursing diagnoses form part of the steps of the nursing process. Therefore, their absence showed that there was poor utilization of the nursing process among the study participants [10]. Similarly, a systematic review to assess 36 articles on the outcomes of nursing diagnoses showed that there were deficits in reporting of signs/symptoms and aetiology, demonstrating that utilization of the nursing process was poor [11]. Similarly, a study involving 200 nurses showed that all respondents never followed the scientific ways of applying nursing process while providing care to patients. These findings correspond to those realized in a study to evaluate utilization of nursing process among nurses in a Psychiatric hospital in Port Harcourt (Nigeria) whereby the nurses’ practice on nursing process was found to be poor [9]. Likewise, a review of 68 medical records at Brazilian teaching hospital showed that all the steps of nursing process were not documented [12]. These findings were in concurrence with those of a study on professional nurses’ perception of the nursing process at the University of Calabar Teaching Hospital, Nigeria which showed that 62.7% of the respondents were constantly using the NANDA diagnostic system, with 25.4% using it occasionally while 11.9% never used it at all [13]. Another study on evaluation of the implementation of nursing process among nurse clinicians established that a total of 57.1% of the respondents said that they used the nursing process in patients care in their hospitals while 25.8% of them said that they never used the strategy [14]. Contrary to these findings, results of a cross-sectional study on the analysis of the nursing records used at public and private centers in the health area Gipuzkoa (Basque Country) showed that nursing process was being utilized to provide nursing care to patients in 98% of all the centers included in the study. This showed that there was good utilization of the nursing process among nurses in the health care facilities [15]. Participants in a study on the barriers and facilitators for execution of nursing process from nurses' perspective in two hospitals at Najran region, Saudi Arabia identified some phases of nursing process where they faced difficulties while implementing the nursing process. Majority of the respondents (63.5%) identified data collection as the most difficult phase followed by formulation of nursing diagnoses (56.8%), evaluation (48.6%) and lastly planning phase (42.3%) [16]. Contrary to these findings, a descriptive retrospective study carried out to review 338 patient documents in three randomly selected governmental hospitals in Amhara regional state (Ethiopia) established that over 78% of the patient profiles had documentations in regard to nursing process. This showed that the respondents had good knowledge on the nursing process [17]. Similarly, the finding of a study on nurses’ perception of nursing diagnosis showed that all the respondents interacted with nursing diagnoses in their daily practice through the use of standardized nursing care plans. They said they formulated some of the nursing diagnoses while others were pre-formed. This meant that not all the nurses formulated nursing diagnoses by themselves [18]. In adequacy in the utilization of nursing process was also established in a study conducted on the factors influencing implementation of the nursing process in Naivasha District Hospital, whereby the respondents who utilized some of the components of nursing process ranged from 15.7% to 30.1% [19].
1.1. Study Question
- What is the observed utilization of nursing process among the nurses in the selected health care facilities?
1.2. Study Objective
- To establish the observed utilization of nursing process among the nurses in the selected public health care facilities.
2. Materials and Methods
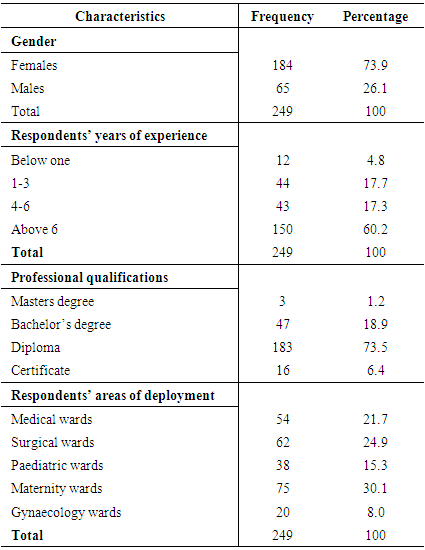
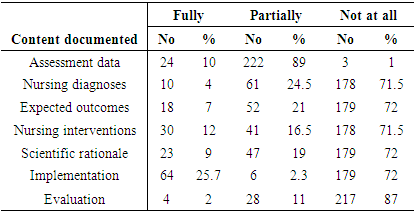
- Cross-sectional study design was utilized to collect data from five selected public health care facilities. Cross-sectional studies are conducted at one time point at a time or over a short period [20]. Cross-sectional studies enable generation of many findings which may be used to create new theories. The study design may also be utilized to prove or disapprove various study assumptions. The data generated in these study designs may be useful in different types of research. However, the design may be used to analyze respondents’ behavior for a long time [21].To collect information regarding the respondents’ socio-demographic characteristics a structured questionnaire was used. Observation checklists were used to record the information gathered from 249 nurses who were observed as they provided nursing care to patients. The checklists were formulated using the standard contents of the nursing care plan. The content included patient assessment data, formulation of nursing diagnosis and formulation of the expected patient care outcomes. Also included in the content were developed nursing care interventions, their scientific rationales, implementation and evaluation. The nurses were observed as they provided nursing care to patients. The information they documented in the patients’ files was then recorded against each of the contents of the checklist as either fully performed, partially performed or not at all. To draw inferences on the respondents’ observed utilization of nursing process, fully and partially performed were collapsed to read “fully-partially” while the other observed performance remained as “not at all”. The collected information was validated and analyzed using STATA software version 14.4.Descriptive statistics on the respondents’ socio-demographic characteristics such as frequencies and percentages were computed. Descriptive statistics were also computed to determine the frequency of each of the observed practice in line with the contents of the checklist.
2.1. Inclusion Criteria
- All the nurses who had worked for more than three months after qualifying from the training school were included in the study.
2.2. Exclusion Criteria
- Nurses on internship or those on orientation were excluded from the study.
3. Ethical Considerations
- Authority to collect data was obtained from the relevant authorities while the respondents signed an informed consent before participating in the study.
4. Study Results
|
|
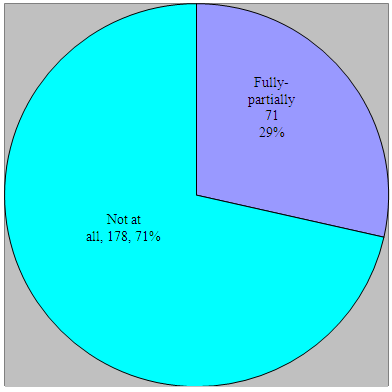 | Figure 1. Respondents’ overall utilization of Nursing Process |
5. Discussion
- Out of the 249 respondents observed, only 10% of them were able to perform and fully document the patient assessment data, an indication that utilization of nursing process among the respondents was poor since documentation is the only evidence that the planned care was provided. Failure to document the care provided to the patient may also lead to medication error like repetition of administration of the same drug among others. On the contrary, a cross-sectional study conducted to analyze the nursing records used at public and private centers in the health area Gipuzkoa (Basque Country) showed that nursing process was being utilized to provide nursing care to patients in 98% of all the centers included in the study, translating to good provision of nursing care to the patients [15]. Findings of the study showed that only four of the respondents fully documented the nursing diagnoses in the nursing care plans according to the assessment data. Since formulation of nursing diagnoses form the basis of developing nursing care interventions, it also means that the nurses did not develop the right interventions, which may also lead to poor patient care. The percentage of the respondents who fully formulated the nursing diagnoses is less than the ones who had documented the patient assessment data. This could still be explained by the fact that more than half of the respondents said that they had difficulties in formulating nursing diagnoses. These findings are in contrast to the results of a case study conducted in three government hospitals in Ethiopia to assess the implementation of nursing process whereby more than 68% of the nursing diagnoses were documented, indicate good provision of nursing care to the patients [17]. If the diagnostic statements are not well formulated, there is likelihood that the nursing interventions and patient care expected outcomes may also be poorly formulated. Consequently, the study findings showed that only seven percent of the respondents managed to document the expected nursing care outcomes in line with the developed nursing diagnoses. With only seven percent of the respondents document the expected care outcomes properly, this also demonstrates that the care provision to the patients was poor. Corresponding findings were established in a study conducted among 150 nurses in three selected hospitals in Ibadan, Nigeria to determine the extent of utilization of the nursing process for documentation of nursing care whereby documentation of nursing care using nursing process was realized to be poor [22]. The study findings also showed that most (71.5%) of the respondents did not document the nursing care interventions, which could also be the explanation why only nine percent of the respondents fully documented the scientific rationales. All these were indications of poor utilization of nursing process among the respondents. Similarly, a study to evaluate utilization of nursing process among nurses in a Psychiatric hospital in Port Harcourt (Nigeria) showed that utilization of nursing process was poor [9]. Regarding the implementation of the nursing care interventions, only 25.7% of the respondents fully documented them, which may be interpreted to mean that the interventions that were not documented were never implementation, which is an indication of poor nursing care to the patients. This could also be translated to indicate that the respondents had difficulties in relation to utilization of the various steps of nursing process. This makes it difficulty for them to provide the required nursing care to the patients. Similarly, a study on the barriers and facilitators for execution of nursing process from nurses' perspective in two hospitals at Najran region, Saudi Arabia showed that most of the respondents faced difficulties in implementing the phases of nursing process [16]. The study results showed that only two percent of the respondents fully documented the nursing care evaluations. Through evaluation of the implemented nursing care interventions, the nurse is able to establish whether the desired outcomes were achieved. If this is not done as in the case of this study, this means that the nurses never assessed the achievement to the set patient care goals. This could possibly lead to poor patient outcomes. Likewise, findings in a study carried out to establish the challenges faced by nurses working in Jaffna Teaching Hospital special units in relation to implementation of nursing process showed that only three percent of them knew how to evaluate the implemented care [23]. Overall, only 28.5% of the respondents were able to carry out their procedures and document according to the steps of nursing process. Corresponding findings were also realized in a descriptive retrospective study which was conducted to evaluate nursing process utilization at a Brazilian teaching hospital by reviewing 68 medical records in which case all the steps of nursing process were not documented [12].
6. Conclusions
- The study results demonstrated that utilization of each of the steps of nursing process was poor. This is because only less than 30% of them were able to utilize each of the steps according to the set protocols. Overall, only 28.5% of the respondents demonstrated proper utilization of nursing process, which translated to poor utilization of nursing process among the respondents. Since this is one of the main strategies which nurses utilize in provision of nursing care, it may also indicate provision of nursing care to the patient sin these facilities was poor. This calls for further investigations to be instituted to establish the possible factors which led to this poor practice of nursing care provision to the patients.
ACKNOWLEDGEMENTS
- The respondents’ acceptance to participate in the study is highly appreciated. The authors also wish to thank the administration of the selected health care facilities for granting authority to collect data.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML