-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2018; 8(2): 27-43
doi:10.5923/j.nursing.20180802.03

Obstetrics Staff Nurses Expected Versus Actual Role at Maternity and Child Health University Hospital
Nadia Abdalla Ali1, Hosnia Abd-Elmoniem Amer2
1Assist.Prof. of Maternity and Child Health Nursing, Faculty of Nursing, South Valley University, Egypt
2Lecturer of Nursing Administration Department, Faculty of Nursing, Zagazig University, Egypt
Correspondence to: Hosnia Abd-Elmoniem Amer, Lecturer of Nursing Administration Department, Faculty of Nursing, Zagazig University, Egypt.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Nurses assume a key role in giving a high quality of maternal services all through the antenatal period, labor and postnatal those contribute to reducing maternal and prenatal death. They are responsible for caregiving, providing up-to-date health education and listening to clients’ suggestions about the services which women need. Each individual within the organization should have specified role, which is reflected in the job description. The Aim is to assess the expected roles of the obstetric staff nurses versus their actual role, on a sample of 40 nurses at the obstetric and gynecology departments' settings at the maternity and child health hospital. A descriptive comparative research design was utilized. Data was gathered from November 2017 to January 2018 Tool. The Staff nurses' role Assessment Questionnaire to assess the obstetric staff nurses expected and actual roles. Results demonstrated that there was a statistically significant difference between the staff nurses expectation of their role and their actual observed practice in their Post-natal nursing care role, and there was an adequate expectation of the staff nurses only at their Antenatal nursing care role, Administrative, and communicator role, and adequate actual performance only in their Antenatal nursing care role. Its concluded that the staff nurses expectation/actual performance for those in “morning” shift is better than “afternoon” shift by 0.151 and for those “night” shift by 0.194, and for those who are “30-39” years is less than those who are “<20” years old by 0.287, and for those who have “bachelor of nursing” as level of education is greater than those who have “others” as level of education by 0.363, Therefore, it is recommended that there was a need for job description and it should be drawn up in consultation with employees; to increase commitment, and to reduce role ambiguity.
Keywords: Staff nurses, Expected role, Actual role
Cite this paper: Nadia Abdalla Ali, Hosnia Abd-Elmoniem Amer, Obstetrics Staff Nurses Expected Versus Actual Role at Maternity and Child Health University Hospital, International Journal of Nursing Science, Vol. 8 No. 2, 2018, pp. 27-43. doi: 10.5923/j.nursing.20180802.03.
Article Outline
1. Introduction
- Obstetrical and Gynecological nursing is a healthcare profession that centers on the care of the women and newborn, hence Obstetrical and Gynecological nurses (OB/GYN nurses) ought to be highly knowledgeable and well-trained caregivers for the overall safety and prosperity of women from the moment of menarche to menopause. [1] Maternal health services incorporate all services given to a woman amid pregnancy, amid conveyance, immediately in the wake of conceiving an offspring and contraception methods. It incorporates medical and dental assessment, health and nutrition education, psychosocial screening and referral, mind coordination, assistance with plans for conveyance and postpartum home visiting [2, 3].Nurses assume an accepted part of giving a high caliber of maternal services all through the antenatal period and labor, will diminish maternal and prenatal death. An antenatal care provider such as a nurse greatly affects the nature of care also, add that Nurses ought to have ethical, moral and professional responsibility to provide care to pregnant women [4]. They are responsible for caregiving, providing breakthrough wellbeing instruction and listening to clients’ suggestions about the services which pregnant women require [5]. Nurses can take a total health history, perform physical examinations, arrange and decipher laboratory investigations, and give essential care to wellbeing support and advancement [6, 7]. Destitute quality of care may come from assortment of variables including insufficient and unfit staff; clinical botch of patients; coldhearted treatment of patients by health staff; chronic absence of basic equipment, supplies, pharmaceuticals, and blood for transfusion; inadequate management of health facilities; and in addition from inadequate functioning of referral systems substandard care adds to maternal wellbeing results [8].Every pregnant woman ought to get quality pre-birth care to assess and treat dangers to both the mother and fetus. Early recognition of high-risk pregnancies permits clinicians to give suitable care to diminish morbidity and mortality. "Women who get early and regular prenatal care will most likely have healthier infants" [10] All pre-birth care suppliers ought to be qualified to give suitable instruction, risk assessment, and treatment to this population.The latest worldwide estimation of maternal mortality is 380 deaths for every 100,000 live births [11]. Studies have found that no less than 88-98% of maternal deaths can be prevented if a good quality emergency, obstetric care is accessible [60]. This field guide is concerned with what should be done to guarantee that a good quality of care is given.Essential responsibilities of nurses in postpartum settings are to assess postpartum patients, give care and teaching and if necessary, report any noteworthy findings. Postpartum nurses are basically detectives looking for findings that might lead to negative results for patients in case of left unattended [12].The nurse should know about normal physiological and psychological changes that occur in clients bodies and psyches remembering the ultimate objective to supply far-reaching care amid this period. In an expansion of client and family teaching, a champion among the most noteworthy duties of the postpartum nurse is to perceive potential therapeutic complication after conveyance. [13] Roles are classifications of behavior, whereas positions are classifications of people. The staff nurse role is a position- related role. A position- related role has three basic elements: the job description (the job one is hired to do), the social expectations, and personal enactment. The new nurse will find that the staff nurse role entails more than the job description and is shaped by both the norms (expectations) of the work group and the personal attributes and values one brings to the role [14].Each role has its own characteristics and the expectations for one position could be in conflict with demands of the other roles. Therefore, when the expectations for one role create conflict with another, role conflict occurs [15]. On the other hand, role conflict is concerned with problems, which emerge as the result of role incompatibility [16].In order to avoid overlapping functions among many different roles, it's recommended that a relevant job description must be developed to delineate and clarify such responsibilities and to avoid expected conflicts. The clear written job description of nurse's role that explains the duties and responsibilities of different nurse's jobs must be available. Also, the specification of the functions and scope of responsibilities should be commensurate with the types of qualification and training of each category as recommended by [61]. A job description identifies important and not- important tasks that are assigned to a particular position. It also identifies reporting relationships and may also describe required qualifications, minimum requirements, working setting, and desirable education. Supervisors are responsible for developing and maintaining accurate and current job descriptions for their staff. The duties should be appropriate for the classification and consistent with the class specification. [17] healthcare settings especially high risk and labor units.
2. Subjects & Methods
2.1. The Aim of the Study
- The aim of this study is to assess the expected role of staff nurses versus their actual role at the obstetric and Gynecological department at South Valley University Hospitals.
2.2. Research Question
- • What is the expected role as perceived by the staff nurses?• What is the actual role of staff nurses?• Is there a difference between the expected role of the staff nurses and their actual role?
2.3. Research Design
- A descriptive comparative research design was used in the present study.
2.4. Setting
- The study was conducted at the obstetrics and gynecology department at the maternity and child health hospital which are affiliated with South Valley University.
2.5. Subjects
- A convenient sample of 40 nurses was incorporated into the present study, representing all the staff nurses in the selected obstetrics and gynecology department at the maternity and child health hospital.
2.6. Data Collection Tool
- Staff nurses' role assessment Questioner was used to collect data germane to the present study, it was developed by the investigator in view of the related literature and guided by the developed job description from the ministry of health. The sample tool was used to assess the staff nurses expected roles and also it was used in a form of the checklist by the investigator to observe the staff nurses actual role.The staff nurses' role assessment Questioner has two parts:-The first part: Concerned with the demographic and work-related data of the study sample, as age, gender, level of education, years of experience in current hospital …. etc.The second part: Staff nurses' role assessment Questioner, to assess the expected staff nurses' role such as Antenatal care role, Post-natal care role, and Administrative role …. etc. Those activities are categorized into 7 major sections of nursing care activities namely; Antenatal care role, Post-natal care role, Administrative role, communicator role, educator role, Advocator role and researcher role. The 1st section for the Antenatal care role (17 items). The 2nd section for the Postnatal care role (33 items). The 3rd section for the administrative role (33 items), The 4th section for the communicator role (5 items), The 5th section for the educator role (5 items), The 6th section for the advocator role (5 items), The 7th section for the researcher role (5 items). The responses of the observational checklist of the participants were checked on either done or not done: done will be scored (1), not done= (0). The responses of the participants related to their expected role were checked on agreed, or not agreed, scored on agreed = (1), not agreed = (0). All the scales of the questionnaire and the checklist were considered adequate if they were more than> 60%, and inadequate if they were less than<60%.
2.7. Validity and Reliability
- The tool utilized as a part of the study was checked for its content validity by a jury of 3 specialists in the field, recommended modifications and reconstruction of the tool were done. The tool has high reliability with Cronbach alpha coefficients 0.85 for the total scale.
2.8. Pilot Study
- A pilot study was done on 10% of the total study samples (4 nurses) to ascertain the lucidity, relevance, and applicability of the study tools as well as to estimate the time needed to answer them, and those subjects were included in the.
2.9. Procedure
- Upon securing necessary permission, the fieldwork was started in November 2017 and was completed by the end of January 2018. To counteract Hawthorne impact amid data collection, observations on practice were at first done before the staff nurses were met. Hawthorne impact alludes to psychological response in which members of research change their conduct since they realize that they are being watched. Each nurse was observed while providing the care for the pregnant women over the three shifts, two nurses were seen in each shift, and each nurse was seen on three distinct events to ensure that the procedures are performed or not using the staff nurses role assessment checklist.After that, the investigator visited the selected settings on daily basis; explaining to the study participant the aim and procedures of the study to obtain their written consent to participate. The researcher also distributed the questionnaires among the nurses after having a full instruction in how to fill them in, it took from 10-15 minutes to complete the form. The filled forms were collected and revised to check for any missing data.
2.10. Ethical Consideration
- An official authorization to lead the proposed study was acquired from the director of the maternal and child health Hospital to ask for consent to direct the study. Prior to recruitment of nurses, the investigator gave a verbal clarification of nature and the aim of the study to staff nurses to get their informed consent to participate. They were informed about their rights to refuse or to pull back from the study at any time without giving any reason. Anonymity and confidentiality of the participants have assured trough coding all data. They were additionally reassured that the information would be confidential and used for the research reason only.
2.11. Statistical Analysis
- Data were analyzed utilizing the Statistical Package for Social Sciences (SPSS) variant 20.0. Cronbach alpha test was utilized to assess the reliability of the scales. Descriptive statistics were computed for the structure and process factors and the outcomes are shown as frequencies, means, and rates. Mean scores for the result components of quality of care were the figure as rates. The percentages were contrasted with the cutoff point of no less than 60% for adequacy to be regarded to provide nursing care role. Significance was considered at p<0.05.
2.12. Limitations of the Study
- The study was directed in one area consequently the outcomes may not be summed up to the entire nation despite the fact that the pattern is comparative in most health facilities of the nation. And the Small sample size, so the findings of the present study are less amenable to generalization because the sample was selected from one geographical area in Egypt (South valley university hospital).
3. Results
- Table (1) Represents the distribution of the staff nurses in the study according to their socio-demographic characteristics. It was found that among the nurses in the study 47.5% of them were working at morning shift, 72.5% of them were 20-29 years old, while the lowest percentage (2.5%) was recorded for those who have (>40 yrs), 37.5% of them had bachelor degree in nursing, and 72.5% have less than <5 yrs. of experience, while the others have (5-10 yrs.) of experience.Table (2) Presented that there was a statistically significant difference between the staff nurses expected the role of the Ante-natal nursing care role and they are actual observed practice in sub items of " Evaluate the pregnant women condition and take a patient history ", " Help in preparing for and carrying out gynecological tests and pregnancy and delivery-related screenings ", " Administer the medication according to the physician instructions. i.e. tables, injections, infusions" and " Provide care of cannula", Where the highest percentage of agreement (100%, 97.5%) was for the sub-item of " Monitor vital signs like blood pressure and pulse rate in pregnant women ", Meanwhile the lowest percentage of agreement (20%, 25%) was regarding the sub-item " Perform bed making " for both expected and actual role respectively.Table (3) Presented that there was a statistically significant difference between the staff nurses expected role of post-natal nursing care role and their actual observed practice among most of responses of study participant's, at <0.05, where the highest percentage of agreement (87.5%) was in the sub item of " Assess general maternal well-being (blood pressure, temp, pulse), Meanwhile the lowest percentage of agreement for the expected role (27.5%) was regarding the sub item of " Check perineum for tears, discharge ", for their actual role the lowest percentage was recorded for most of the items of the Immediate postpartum nursing care for the newborn.Table (4) Presented that there was a statistically significant difference between the staff nurses expected administrative role and their actual observed practice among most of responses of study participant's, at <0.05, where the highest percentage of agreement (100%, 92.5%) was in the sub-items of " Daily checkup of supplies and equipment for each shift " and " Keep the supplies and equipment in correct and safe way " for both the expected and actual role respectively. Meanwhile the lowest percentage of agreement for the expected role (25%) was regarding the sub-items of " The sharps container is changed if it's 3⁄4 full "and " Sign and date the sharps container and indicate the origin", for their actual role the lowest percentage (10%) was in the sub-item of " Know the content of the crash cart " and " Check the crash cart every shift and after every use.Table (5) Presented that there was a statistically significant difference between staff nurses expected communication role and their actual observed practice on the sub-items of " communicating verbally and write any changes in patient health status to the physician", and " Asking easily for advice from nurses in this unit ", where the highest percentage (90%) of agreement for the expected role was on the sub-items of " Asking easily for advice from nurses in this unit ", and on " Communicate verbally and written any changes in pregnancy women health status to the physician" for the actual role, Meanwhile the lowest percentage of agreement (37.5%) for the expected role was regarding the sub item of " Answer to the pregnant women and family questions " and on the sub-item " When communicating with pregnancy women consider their religious and ethical values" for their actual role.Table (6) Presented that there was an insignificant difference between the staff nurses expected educational role and their actual observed practice, the highest percentage of agreement (40%) was on the sub item of " Assess learning needs of pregnancy women, considering religious and ethical values ", Meanwhile the lowest percentage of agreement (12%) was on the sub items of " Orient the newly admitted pregnancy omen to the environment and inform them about procedures and treatments which constitute part of their care" and "Participating in the students training and evaluation" for both the expected and actual role.Table (7) Presented that there was a statistically significant difference between the staff nurses expected advocacy role and their actual observed practice on the sub item of "ensuring that the pregnancy women choose treatment options without coercion", the highest percentage of agreement of the expected role (45%) was on the sub item of " Respect a pregnancy women decision, even if it differs from the decision the nurse would make ", and (50%) for the sub items of "Seeking appropriate consultation when advocacy results in intrapersonal or interpersonal conflict", for the actual role, Meanwhile the lowest percentage of agreement (15%, 20%) was on item " Inform the pregnant woman about the implications of any decisions regarding his health status " for both the expected and actual role respectively.Table (8) Presented that there was an insignificant difference between the staff nurses expected researcher role and their actual observed practice, the highest percentage of agreement (42.5%, 37.5%) was on the sub item of " Support study implementation within the context of clinical care in dedicated clinical research sittings ", for both the expected and actual role respectively, Meanwhile the lowest percentage of agreement (35%, 27.5 %) was on the sub item of " Fairly identify appropriate research participants, minimizing the research risks and maximizing potential benefits" for both the expected and actual role respectively.Table (9) Presented that there was a statistically significant difference between the staff nurses' total expectation of their post-natal nursing care role and their actual observed practice, Where the highest percentage of the staff nurses total expectation and actual performance of their role was (70%, 72.5%) for their Antenatal care role respectively, while the lowest percentage (27.5%) was for their Advocate role. For their actual role, the lowest percentage (32.5%) was for their educational and researcher role.Table (10) Presented that there was a statistically significant difference between the staff nurses expected / actual role and their level of education.Table (11) Practice score for base categories (“morning” shift, “<20 yrs” age and “others” level of education), Practice score for those in “morning’ shift is greater than “afternoon” shift by 0.151 in average, Practice score for those in “morning” shift is greater than “night” shift by 0.194 in average, Practice score for those who are “30-39” years is less than those who are “<20” years old by 0.287 in average, Practice score for those who have “bachelor of nursing” as level of education is greater than those who have “others” as level of education by 0.363 in average.
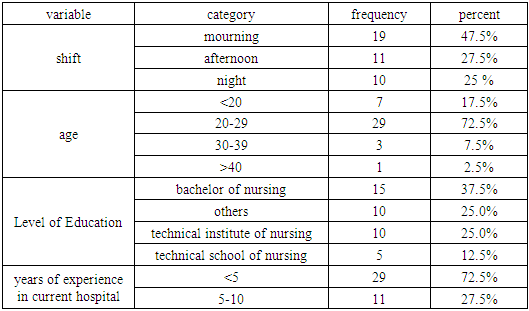 | Table 1. Socio-Demographic and Work Related Characteristics for the Staff Nurses (N = 40) |
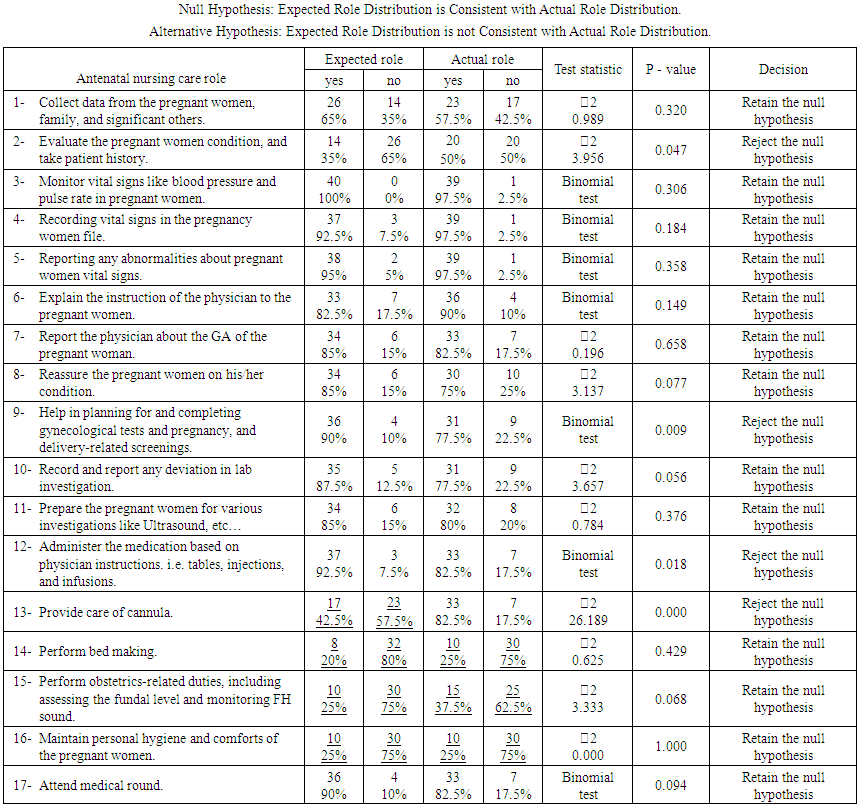 | Table 2. Comparison Between Expected Versus Actual Staff Nurses Ante Natal Nursing Care Role (N= 40):- |
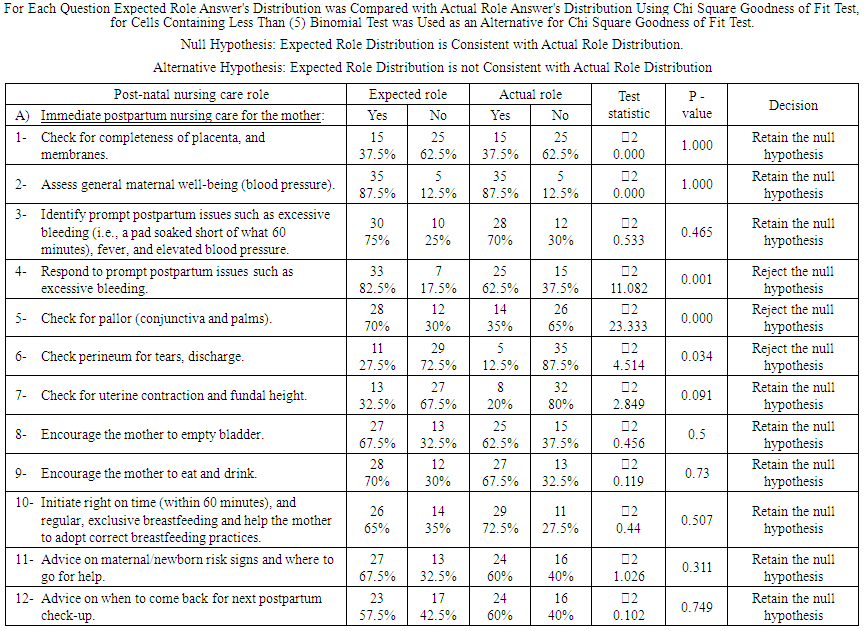 | Table 3. Comparison Between Expected Versus Actual Staff Nurses Post-Natal Nursing Care Role (N= 40):- |
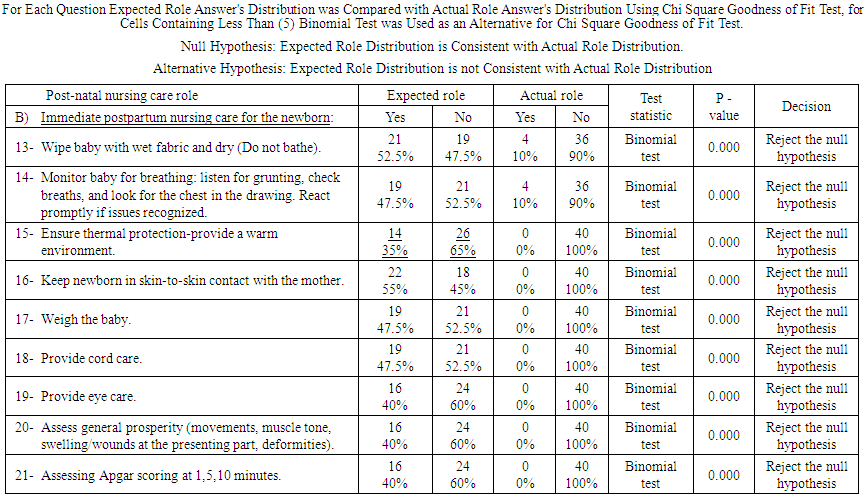 | Cont… Table 3. Comparison between Expected Versus Actual Staff Nurses Post-Natal Nursing Care Role (N= 40):- |
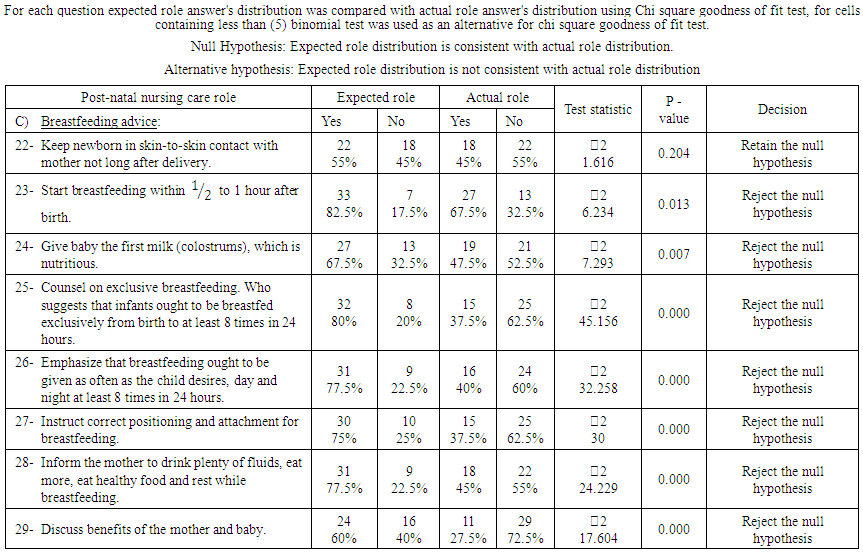 | Cont….Table 3. Comparison between expected versus actual staff nurses Post-natal nursing care role (N= 40):- |
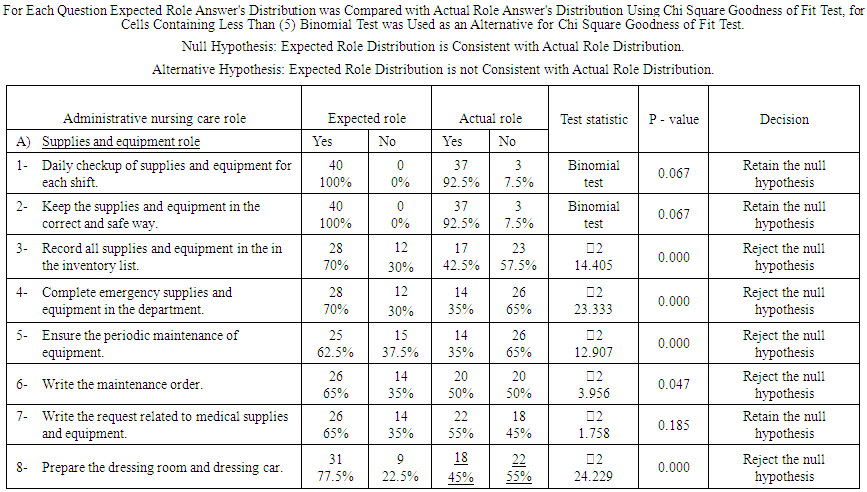 | Table 4. Comparison between Expected Versus Actual Staff Nurses' Administrative Role (N= 40): |
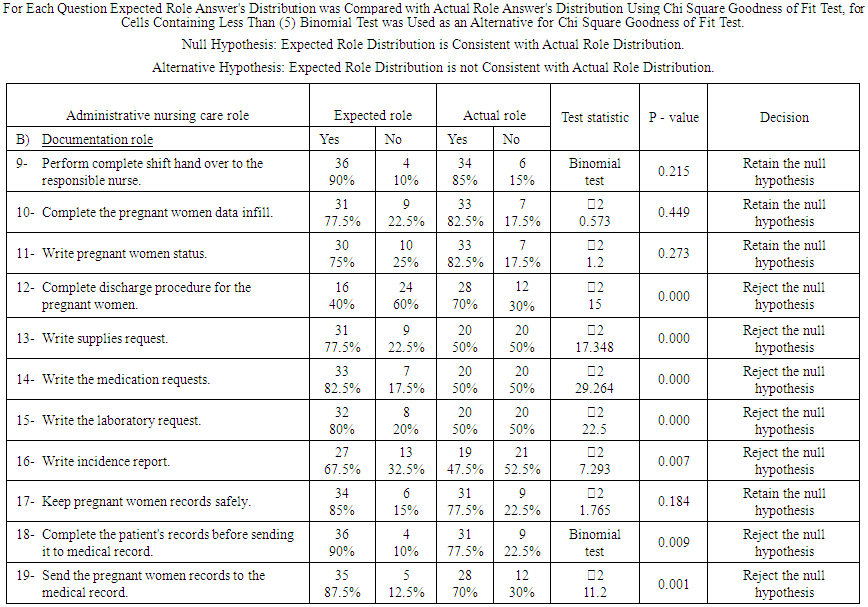 | Cont…. Table 4. Comparison between Expected Versus Actual Staff Nurses' Administrative Role (N= 40): |
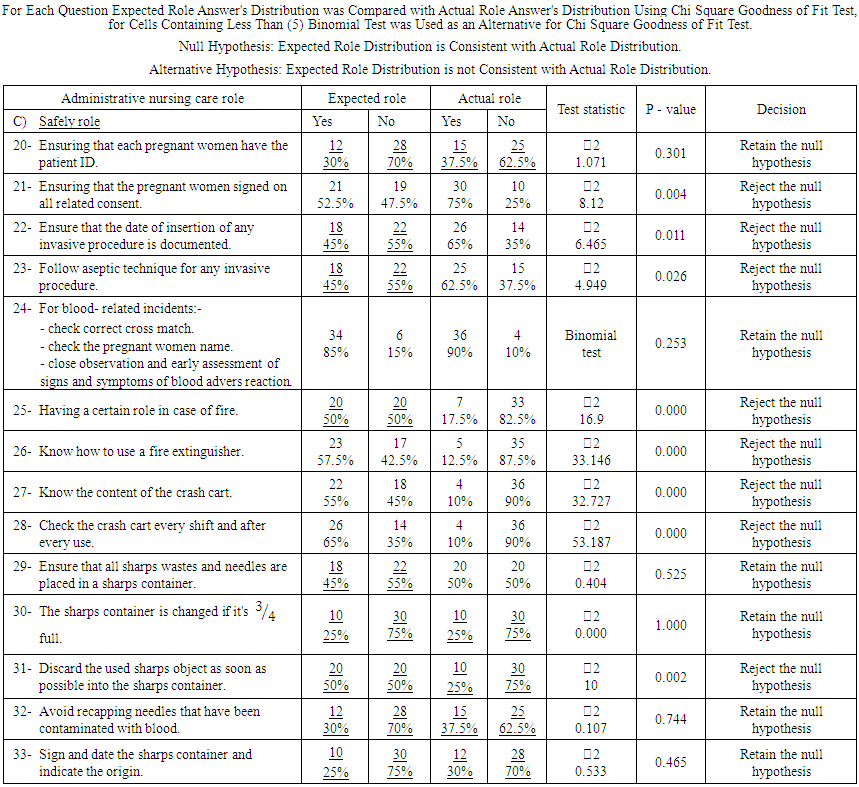 | Cont…. Table 4. Comparison between Expected Versus Actual Staff Nurses' Administrative Role (N= 40): |
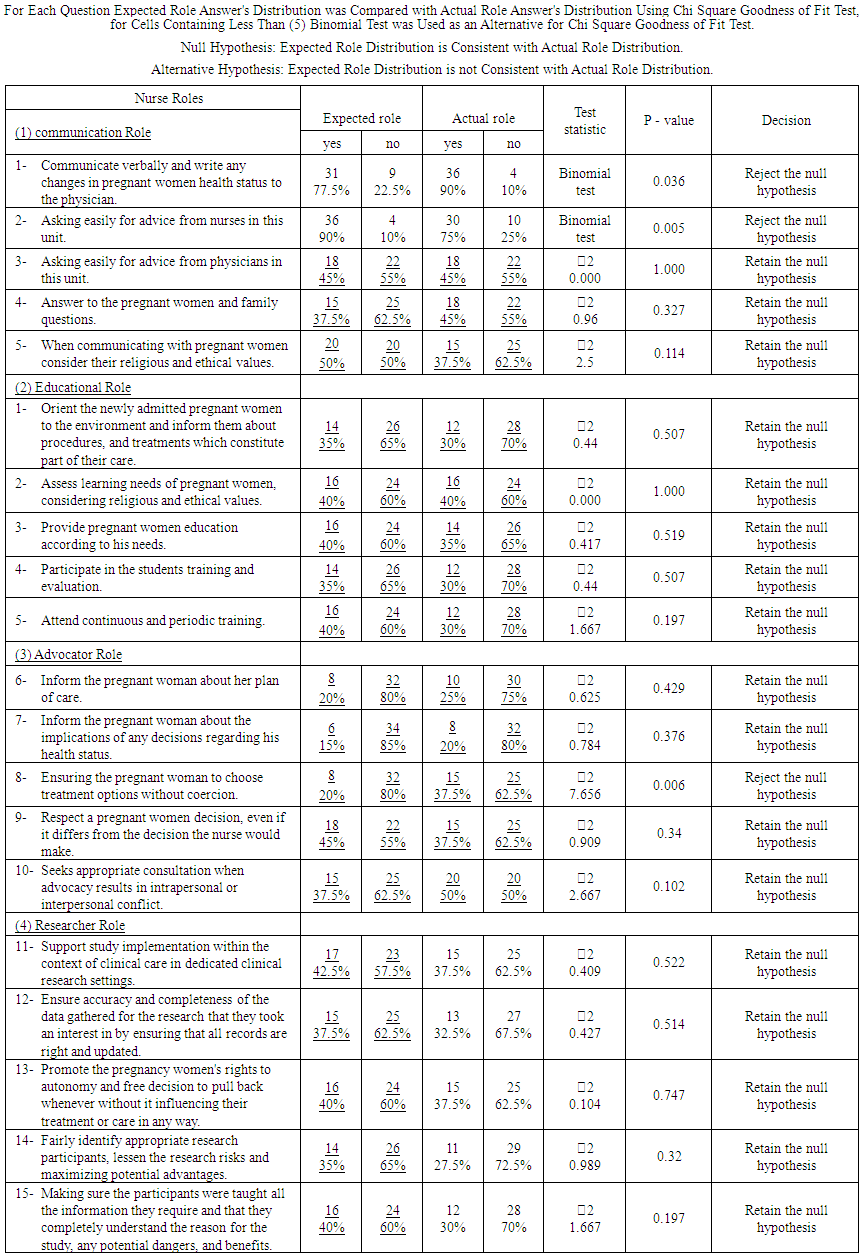 | Table 5. Comparison Between Expected Versus Actual Staff Nurses Communication, Educational, Advocator and Researcher Role (N= 40):- |
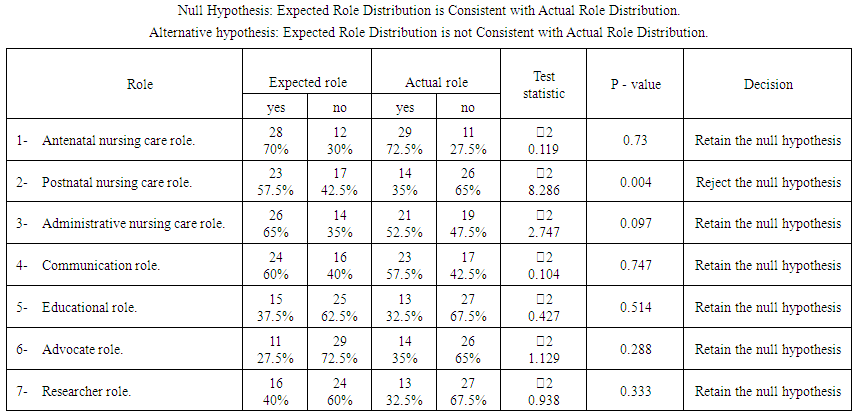 | Table 6. Comparison between Total Expectation Versus Actual Performance of The Staff Nurses for All Dimensions of Their Role (N= 40):- |
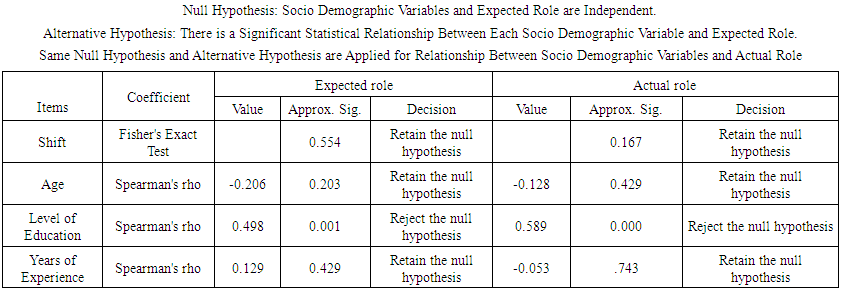 | Table 7. Relation between Staff Nurses' Expected / Actual Role and Their Work Related Characteristics (N=40):- |
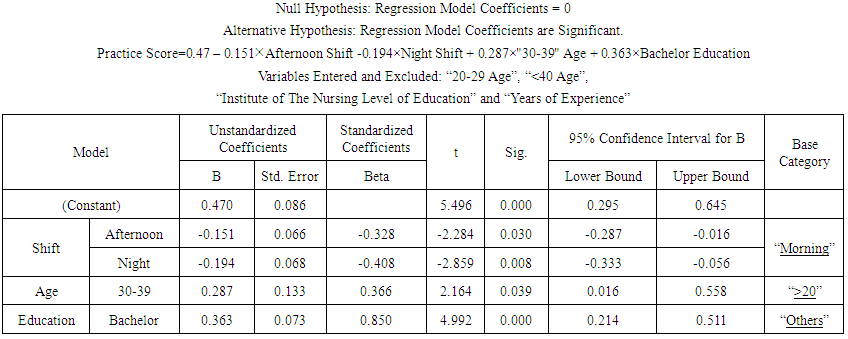 | Table 8. Regression Model for Practice Score: |
4. Discussion
- In the present study seven areas of the staff nurses' role at the Obstetric and Gynecology unit were examined to assess the expectation of the staff nurses' role and their actual role at south valley university hospital, and it was revealed that Nearly half 47.5% of the study sample were working at morning shift; followed by the afternoon shift 27.5% and the night shift 25%, the age of the most of the staff nurses was ranged between (20-29 yrs.) and minority of them were (>40 yrs.). This result was supported by that of [18-20] who reported approximately similar findings. As regards level of education, slightly more than one third of the study sample was holding the baccalaureate degree, while the others were either graduated from Technical Institute or School of Nursing, or any other degrees, this could be explained by the fact that the college education programs are much smaller compared to the technical programs. Also, the hospital administrators resort to technical nurses to manage nursing manpower shortage [21]. It was noted that hospital administrators make optimum utilization of the available baccalaureate nurses by assigning them to leadership positions. In congruence with this, [18]. Found that the majority of nurses had a technical nursing school certificate, and stated that, the nurses' level of education showed a great impact on their knowledge and skills for patient care.As regard years of experience, most of the staff nurses had less than five years of experience, while the others had (5-10 yrs.) of experience. This result is in accordance with the study of [18], that was carried out at El- Demerdash University Hospital. On a 120 staff nurse to develop an assessment of training needs tool, as the investigator emphasized that insufficient knowledge and practice of some nursing tasks, could be the result of lack of experience in a particular area of clinical nursing with proper instruction and supervised practice. Concerning the staff nurses Antenatal care role , the study findings revealed that there was a statistically significant difference between the staff nurses expectation of their direct care tasks and their actual observed practice in the sub-items of Evaluate the pregnancy women condition and take patient history " and " Provide care of cannula", As the respondents already doing these activities, but they didn’t expect them as their own role, this means that they perform some activities while they didn’t aware that its apart of their role. And in the sub-items of "Help in preparing for and carrying out gynecological tests and pregnancy and delivery-related screenings ", "Administer the medication according to the physician instructions. i.e. tables, injections, infusions" As these items were expected by the respondents as their own role but they weren’t actually performing them, due to workload, lack of time, or inadequate facilities. This result was in accordance with [22] that investigating the perception of 104 staff nurses and their 31 nurse managers regarding their role during working at El Helmeya military hospitals in different departments, and the investigator found statistically significant differences were revealed between staff nurses' perception of their perceived actual and expected roles as caregivers. The differences were always in favor of the expected rather than the perceived actual roles. This reflects a high awareness of these staff nurses about what should be done, although they might not be doing it due to workload, lack of time, or inadequate facilities. It also indicated that most of the sub-items of the antenatal care role were expected by the respondents as their own roles and admitting they performed them and they were actually performing them, because these activities are mainly nursing role and their supervisors focused only on these activities and it was the main concern during their round, these result supported by [23] who found the nurses consumed more than half of their working hours in the direct patient care activities. It's also noted that the sub-items such as " Perform bed making", "Perform obstetrics-related duties, including assessing the fundal level and monitoring FH sound", and " Maintain personal hygiene and comforts of the pregnancy women " weren’t expected by the respondents as their own responsibilities and they weren’t actually performing them . This means that the staff nurses were lacking knowledge of the holistic responsibility of their antenatal care role as a result of an absence of supervision to nurses during work and inadequate training, in addition to their role description was not disseminated to them. this result was supported by [24] as they stated that the lack of supervision, standardized training and continuing education of staff nurses working in hospitals contributed to shifting of their comprehensive role as providing holistic nursing care to patient and appear to be more focused on providing personal care and supportive services than on performing technical skills as physical examination and observation of patient.On studying Effect of Clinical Supervision on Quality of Care and Job Satisfaction On 37 first-line nurse managers and 100 of their staff nurses, the investigator stated that, For nurses with less clear role perception, supervision and direction would help them to perform their job, thus increasing their satisfaction and performance. Moreover, observation for different situations in clinical care areas revealed that first-line nurse managers have little knowledge and experience in personnel management especially staff supervision [25].Regarding to the staff nurses post-natal nursing care role ,the study findings reveled that there was a statistically significant difference between the staff nurses expected role and their actual observed practice among most of the responses of study participant's, at <0.05 As the respondents expected them as their own role but they weren’t actually performing them, this may be due to nursing shortage and increase workload, inadequate training, poor physical workplace, supplies not all around loaded, numerous family needs, and incapable communication among multidisciplinary colleagues, as stated by [26]. In their study that included evidence from 31 studies from low- and center wage nations on factors that impact the arrangement of intrapartum and postnatal care among talented birth orderlies including specialists, maternity specialists, nurses, assistant attendants and their administrators..as they stated that Nurses did not always comply with protocols and guidelines, even when aware of them. For example, when providing postpartum care, they did not always monitor bleeding and uterine involution or check vital signs every 15 minutes [27]. Some studies described how health workers continued to practice ineffective procedures because they were considered routine [28] due to lack of time; because health workers lacked the autonomy not to follow what they knew to be inappropriate care [29] or when it was unclear who was responsible for carrying out specific tasks, such as using a pantograph [30]. They also stated that the Staff shortages were widely reported as a problem [28, 31-35] and led to increased workloads [32, 36, 37] which in turn sometimes compromised the quality of care [20, 32, 34]. For instance, one study reported that heavy workloads limited the time that health workers had for conducting thorough assessments of women, and only women suspected to have complications were examined [20]. Heavy workloads could also lead nurses to omit some aspects of care, such as changing gloves or hand hygiene [36, 38] also In settings where staff shortages were a major problem, informal task-shifting was possible because nurses had vague job descriptions that led them to perform tasks that were beyond their expertise or scope of practice [39].Lack of equipment also limited health workers’ ability to provide quality care to mothers and their babies. For instance, studies reported a lack of stethoscopes and blood pressure machines [30] cord clamps and delivery kits [37, 40] complete vacuum evacuation sets [41] instruments to repair lacerations [33] Ambu bags (and oxygen) for neonatal resuscitation [30] sterilizing equipment such as autoclaves [31, 33] and laboratory and diagnostic tools [32].Some mothers and their babies received poor quality care as a result of this lack of equipment. In some studies, neonates were not resuscitated due to lack of Ambu bags or oxygen [30]; monitoring of mothers and their babies was insufficient due to lack of equipment [30] and lacerations were left unrepaired due to lack of instruments [33].Inadequate pre-service and in-service training sometimes limited nurses skills and their ability to provide care. Some studies described how health workers sometimes lacked training in communication and were thus limited in their ability to share information with mothers and sometimes also lacked sufficient training to manage complicated pregnancies or deliveries. [32, 42].Regarding to the staff nurses Administrative role, It was showed that there was a statistically significant difference between the staff nurses expected role and their actual observed practice among most of responses of the study participant's, at <0.05, As these items were perceived by respondents as their own role but they weren’t actually performing them, and this may be due to nursing shortage and increase workload, In addition to lack of supervision emphasized the need for indirect nursing tasks as a part of nursing role, also there is no well-planned job orientation program to explain the roles and responsibilities properly, as stated by [43] in her article titled " No end in sight to nursing shortage: bottleneck at nursing schools a key factor " the researcher indicated that the supply of nurses is not sufficient to meet the present demand, and the shortage is anticipated to develop more extreme as future demand increments. At the point when a nursing shortage happens, the workload increments for those who stay at work. Likewise in light of increasing health care costs, hospitals reduced their nursing staffs and executed required extra time policies to meet surprisingly levels of high demands, which essentially expand nursing workloads. Regarding the staff nurses' communication role, the study findings indicated that there was a statistically significant difference between the staff nurses expected role and their actual observed practice on the sub-items of "communicating verbally and write any changes in patient health status to the physician", and " Asking easily for advice from nurses in this unit " and this may be due to the shortage of nursing staff, increasing work hours and workload. For The remained activities there was a similarity between expected and actual role as there were slight difference between actual and expected staff nurses communication role, As there were a little expectation and actual performance for their role in communication, From the researcher point of view, this could be due to absence of awareness about the policies and content of verbal reports, there is no clear rules for verbal transmission of information, differing opinions, even among nurses, Frequent interruptions and distractions. This result was supported by [44] in the article titled "Nurses’ Role in Communication and Patient Safety" indicated that Lack of structure, policies, and procedures related to the content, timing, or purpose behind verbal reports. No shared mental model or structure for verbal healthcare communication. No rules for verbal transmission of information, either face-to-face or via the telephone. Contrasting opinions, even among nurses, frequent interruptions and distractions were the major communication barriers for nurses.Also, [36] stated that some nurses did not value communication with mothers, communicated poorly, or said they had problems with communication. Some studies reported that health workers considered communication with mothers as a waste of time. [29, 36].Additionally, Disrespectful communication, lack of trust, poor teamwork and coordination, and inadequate opportunities to discuss clinical practice could lead to poor inter-professional relations. Tensions could also arise when health workers did not recognize each other's’ capabilities or when they acted in a way that reinforced clinical hierarchies. Some studies reported instances of disrespectful inter-professional communication [30, 36]. For instance, when doctors shouted at midwives, midwives could feel humiliated and lack confidence and lead them to believe that they were not trusted, or that their opinions were not welcomed and could delay the delivery of care [30].As regard the respondents expected and actual educational role behavior, it's noted that there was an insignificant difference between the staff nurses expected role and their actual observed practice, For The remained activities there was a slight difference between their expected and actual role, As there were a little expectation and actual performance for their educational role, and this might be due to their lack of knowledge regarding teaching patient, and the hospital does not provide continuing education in this field. In agreement with this explanation, [45] have stated that staff nurses cannot provide the best in their role as educators to meet the demands of patients care due to lack of knowledge and attitude, in addition to the absence of equipment. Also, this result supported by [46] who studied the Nurses’ Perception of Performance and Responsibility of Patient Education and he noted that Shortage of time is reported to be the biggest constraint to carrying out the role as an educator, a shortage of healthcare professionals and time constraints are long-standing problems that nurses face.The results of the Sindh, Pakistan (2007), a study revealed that only 31% of women were given instructions about perinatal care [47]. These findings indicated that nurses \were either neglect or having no educational skills.But it is not consistent with the study of [48] who examine how postpartum care was delivered in three postnatal hospital clinics in ADares Salaam, Tanzania on 10 nurse and three obstetricians, as they believed that education was an essential and urgent practice that helped improve mothers’, babies’, and families’ health and well-being. While their beliefs and practices fit well with the values within the health discourse, lack of time and space limited their effective provision of health education to and uptake of knowledge by mothers. Despite all these challenges, participants applied various teaching strategies to facilitate mothers’ and families’ acquisition of knowledge that would assist mothers and their babies to stay healthy throughout the postpartum period.For the staff nurses role in nursing student training and evaluation, [49] studied the impact of staff nurses on clinical learning. The authors found that staff nurses play an important and vital role in the clinical education of students. Students who received constructive feedback from the nurse manifested enhanced analytic skills and socialization in the clinical setting. [49] summarized that students felt constructive feedback from staff nurses was perceived in a positive manner and was beneficial to the nursing student and helped the nursing student to understand areas where improvement was needed and offered them an opportunity to improve their performance. Instructors can perform these same actions but coming from a staff nurse it means more and is more beneficial to the student.Concerning the staff nurses' advocacy role, the study findings indicated that there was a statistically significant difference between the staff nurses expected role and their actual observed practice on the sub item of " Ensuring the pregnancy woman to choose treatment options without coercion " as there was a 20 % of them were expected it as their role , but 37.5% of them were actually doing it .from the investigator point of view, it could be due to absence of empowerment or training the staff nurses to be a creative member and inhibition of nursing autonomy.For The remained activities, there was slight difference between actual and expected staff nurses advocator role, As there was a little expectation and actual performance for their advocator role, From the researcher point of view, these activities were not expected or performed by the staff nurses for some reasons, lack of awareness of national law and code of ethics, and inadequate time to connect with patients and families. This result supported by the investigation of [50] on 248 nurses working in labor and delivery for a half year as staff or charge nurses , As the examiner asserted that nurses are aware of the best thing to do and they have a positive attitude toward patient advocacy [51-55] however because of institutional barriers are kept from taking any action. Empirical literature supports this view as labor and delivery nurses do not perceive themselves as having power or influence in their work setting to make the change [56]. Also, Nurses sometimes conducted procedures without asking mothers for their opinion [29] or did not seek feedback from mothers about practices or outcomes but expected mothers to co-operate [19].Inconsistency with this [57] from the data analysis of their study of Patient advocacy: barriers and facilitators, several fundamental subjects rose to portray the variables that hindered or facilitated patient advocacy, Nurses in their study recognized powerlessness, the absence of support, lack of national law and code of ethics, restricted communication, physicians leading, risks of advocacy, eminence to peers, absence of inspiration and inadequate time to cooperate with patients and families are the greatest obstacle to advocacy is the healthcare institution.As regards the respondents expected and actual researcher role behavior, it was noted that there was an insignificant difference between the staff nurses expectation of their role and their actual observed practice, and there the slight difference between actual and expected staff nurses researcher role. As there were a little expectation and actual performance of their role, and this may be due to absence of communication and interpersonal skills, lack of standardized training and continues education of nursing staff and lacking knowledge of the Ethical Principles for Medical Research Involving Human Subject, disappointment because of inability to apply research findings to clinical practice, Lacking of leadership and organizational support, absence of time, and absence of assets. This result was as per [58] as they contemplated the basic role of the clinical research nurse, in their Clarification of staff nurses roles and obligations in the clinical research they recommended that nurses must have an excellent communication and interpersonal skills. They not just need a comprehensive understanding of the specialty in which they are working, but also an extensive knowledge of the research process and research-related legislation. Furthermore, they require a variety of computer-based aptitudes, particularly in the utilization of the word processing, spreadsheets, database and presentation software, and the capacity to embrace internet seeks.When comparing the staff nurses' total expectation of all dimensions of their role and their actual observed practice, there was a statistically significant difference between the staff nurses expectation of their post-natal care role and their actual observed practice, and the highest percentage of agreement (70%, 72.5%) for both the expected and actual role respectively was recorded for the Ante natal nursing care role, while the lowest percentage (27.5%) of agreement was for the Advocator role, And for the Educational and Researcher role (32.5%) in their actual practice, This could be due to lack of role clarity and/or inconsistency on performing these activities.The findings of the study showed that the staff nurses expectation / actual observed practice wasn’t affected by their working shifts or any of their demographic characteristics such as age, experience, but it was found there was a statistically significant difference with their educational level for both the expected and actual role. This result supported by the research that was led by [59] in mainland China, to analyze the developing literature relating to job satisfaction between nurses, it was noted that nurses’ educational level is an impacting factor on nurses’ perspectives and experiences of their working lives, with the results it was noticed that the level of education of nurses influenced how they play out their obligations. A nurse whose level of education is high has more options, for instance, in conduction her work. There are times when critical decisions must be made by the nurse without her counseling anyone for different reasons. A nurse with grounded education will have the capacity to confront any difficult circumstance wisely. In concurrence with this [5] expressed that the care providers demographic features additionally impact the nature of antenatal care. In an extensive review, the outcomes demonstrated that quality of antenatal care was connected with the nurses’ demographic characteristics such as their level of education, a span of employment experience, and participation in training programs initiating a high quality of antenatal care. Practice score for base categories (“morning” shift, “<20 yrs” age and “others” level of education) the staff nurses expectation /actual performance for those in “morning’ shift is better than “afternoon” shift by 0.151 in average, and for those in “morning” shift is better than “night” shift by 0.194 in average, and for those who are “30-39” years is less than those who are “<20” years old by 0.287 in average, and for those who have “bachelor of nursing” as level of education is better than those who have “others” as level of education by 0.363 in average.
5. Conclusions and Recommendations
- Based on the study findings, it's concluded that there was an adequate expectation of the staff nurses only at their Antenatal nursing care role, Administrative and communicator role, and adequate actual performance only in their Antenatal nursing care role. And there was low expectation of the staff nurses to various dimensions of their role, especially in Postnatal nursing care role, Educational, Advocate and Researcher role and poor actual performance for all dimensions of their role except the Antenatal nursing care role, Also there was a statistically significant difference between the staff nurses expectation of their role and their actual observed practice. In their Postnatal nursing care role, and this could be due to lack of role clarity and/or inconsistency on performing these activities, these discrepancies could be related to lack of awareness about the job description and would lead to role ambiguity. The results of the study stated that the staff nurses expectation / actual observed practice wasn’t affected by their working shifts or any of their demographic characteristics such as age, experience, but it was found there was a statistically significant difference with their educational level for both the expected and actual role, those who have bachelor degree of nursing have better expectation and actual performance than those who have other levels of education by 0.363 in average. Recommendation:- • Job descriptions should be drawn up in consultation with employees; to increase commitment and improving productivities. • A written job description should be provided and explained to new nurses during the orientation. • Periodic training courses and workshops regarding applying updated antenatal care standards should be designed and conducted for the maternity nurses.For nurse managers and supervisors:-• Managers ought to guarantee an adequate number of staff and qualification according to work condition and an adequate number of professional nurse's in the hospital at all times and shifts.• Change in policies, role, and procedures should be communicated to all nurses to avoid conflict and ambiguity.• Nursing/maternity specialists leaders ought to be engaged in policy-making within an appropriate legal framework• Women satisfaction regarding antenatal care services should be continuously evaluated.• Lastly, identification and elimination of factors hindering the performance of expected and actual roles are proposed.Further researches are proposed to:-• Investigate the clinical issues and obstacles confronting the nurses in providing high-quality nursing care in various obstetric settings.• Raise women’s awareness regarding the importance of antenatal care and follow up visits.• Evaluate the effectiveness of training programs on nurses’ knowledge and practices in other obstetrical.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML