-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2017; 7(5): 103-106
doi:10.5923/j.nursing.20170705.01

Deep Breathing Exercise and Its Outcome among Patient with Abdominal Surgery: A Pilot Study
Shashi Tripathi1, Rakesh Sharma2
1Tutor, TMU College of Nursing, Moradabad, Uttar Pradesh, India
2Faculty Nursing, College of Nursing AIIMS, Raipur, Chhattisgarh, India
Correspondence to: Rakesh Sharma, Faculty Nursing, College of Nursing AIIMS, Raipur, Chhattisgarh, India.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Changes in pulmonary dynamics after abdominal surgeries are well documented. Deep breathing exercises with incentive spirometry, may help counteract Post-operative decreased vital capacity; however, the evidence for the role of incentive spirometry in the prevention of postoperative complications are not clear. Method: A pilotstudy was conducted with quasi-experimental research design to assess the effectiveness of deep breathing exercise by spirometry on post-operative pulmonary complications with abdominal surgery. A total 40 study participants, 20 in experimental and 20 in control group based on inclusion and exclusion criteria. Data collection questionnaire were prepared with extensive review of previous literatures. Data collection tools includes, demographic profile, clinical profile of patient and Incentive Spirometer (IS). Deep breathing exercise (DBE) was taught and practiced by the patients in experimental group and in control group routine treatment was followed. Result: The scores in respiration rate was significantly different in experimental group and the volume of the spirometry scores were higher in post-operative phase after DBE with IS. The oxygen saturation remain constant in experimental group while there was a reduction in control group significantly. Patient with Incentive Spirometry deep breathing exercise did not develop any respiratory complication post-operatively. Conclusion: In present pilot study, we found that implementing deep breathing exercise during pre-operative phase with incentive spirometer was effective in terms of enhancement of lung capacity and prevention from post-operative complications.
Keywords: Deep Breathing Exercise, Incentive spirometer, Abdominal Surgery, Post-operative Pulmonary complications
Cite this paper: Shashi Tripathi, Rakesh Sharma, Deep Breathing Exercise and Its Outcome among Patient with Abdominal Surgery: A Pilot Study, International Journal of Nursing Science, Vol. 7 No. 5, 2017, pp. 103-106. doi: 10.5923/j.nursing.20170705.01.
1. Introduction
- It is known that surgical procedures in the abdominal area promote changes in pulmonary function and respiratory mechanics, leading to post-operative pulmonary complications (PPCs) [1]. Some of the main changes that lead to PPCs are: (a) decreased diaphragm mobility; (b) depressed central nervous system; (c) changes in the ventilation-perfusion ratio; (d) reduced cough efficacy; (e) increased respiratory rate; and (f) reduced pulmonary volumes and capacities [2-4]. Chest therapy with breathing exercises after surgery is directed towards maximal inspiration in an attempt to prevent overt atelectasis and allow for the early re-expansion of collapsed alveoli. In a previous clinical trial we demonstrated equivalence when we compared incentive spirometry with physiotherapy for patients under- going abdominal surgery [4]. Nearly one-quarter of deaths occurring within 6 days of surgery are related to postoperative pulmonary complications [5].Post-operative pulmonary complications, such as atelectasis, pneumonia, respiratory failure, sputum retention and shortness of breath, is of major concern after abdominal surgery [6]. Surgery is a great stressor to patients and causes large physiological changes, ranging from tissue trauma, immobility and systemic effects to psychological distress and reduced quality of life [7]. After Major Abdominal Surgery (MAS), 35% of the patients experience postoperative complications. The majority of these are pulmonary (pneumonia and respiratory failure), which occur in 9% of all patients after major abdominal surgery. Overall 30-day mortality was 10%. Improvement of their functional capacity by means of Preoperative Exercise Therapy (PEXT) may enhance physical capacity at the moment of hospital admission and may facilitate better recovery after surgery [8].
2. Material and Method
- A pilot study was conducted with quasi-experimental research design to assess the effectiveness of deep breathing exercise among patients with abdominal surgery and to reduce postoperative pulmonary complications. Data collection questionnaire were prepared with extensive review of previous literatures. Data collection tools includes, demographic profile and clinical profile of patient and spirometer. A total 40 study participants, 20 in experimental and 20 in control group based on inclusion and exclusion criteria. Patients were selected those with a planned surgery, without any respiratory problem, not having any diseases with related endocrine, renal, and cardiovascular system. Patients, who has refused to participate, restricted by doctor to include in the study were excluded from the study. Data were collected in two phase to prevent contamination of sample. In first phase, 20 patients were selected for control group and data were collected. During second phase, 20 patients were selected and all were taught about deep breathing exercises (DBE) with Incentive Spirometry (IS) at the beginning and asked to repeat 4-6 cycle for 8-10 times in a day. They were given a note book with the printed instructions, timing and one Incentive spirometry to do procedure. Data were collected on preoperative and postoperative period. During preoperative phase, first assessment was on day – 1 (24hours) prior to surgery, second assessment in the day of surgery in pre-operative room, 2-3 hours before surgery. While, in post-operative phase, four times data were collected, at 8th hours, 12th hours, 24th hours and 36th hours of after surgery. Ethical considerationStudy was conducted after administrative approval from the university research committee. All the participants were explained about the study and a written consent was obtained.
3. Results
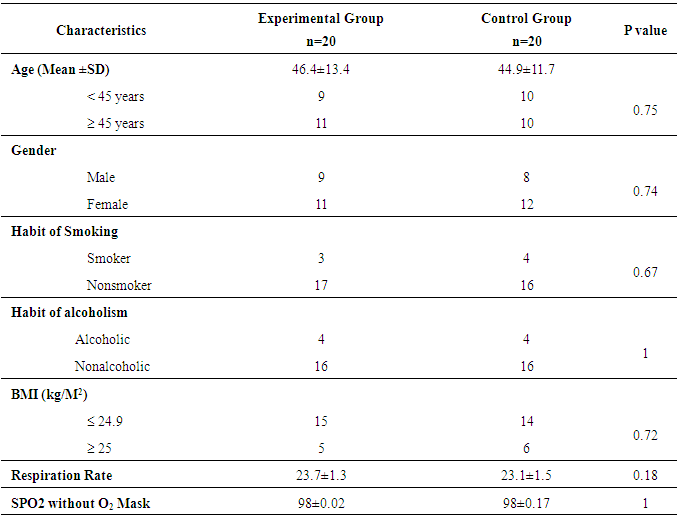
- A total 40 cases with abdominal surgery were involved in the study. Table 1 displays the baseline characteristics of patients in experimental and control groups. At the baseline all the study participant from both the groups were statically equal. Hence, patient’s characteristics did not influence in the intervention of the study.
|
|
|
4. Discussion
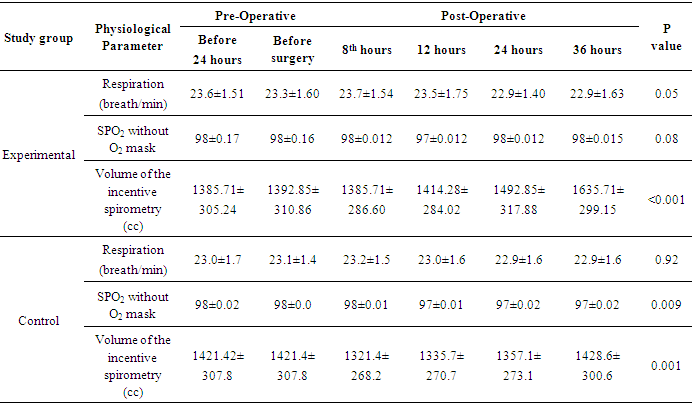
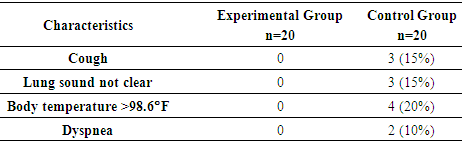
- Post-operative respiratory insufficiency is common in operative patients, and this is a very complicated and costly too. It had been evident that some of lung expansion strategies like deep breathing exercise, incentive spirometry, continue airway pressure if implemented during pre-operative phase and continued in post-operative phase may decline the post-operative pulmonary complications [9]. In the present investigation, it was found that deep breathing exercise with incentive spirometer improves respiratory functions and prevent from postoperative pulmonary complications. In present study, respiration rate among experimental group had a significant reduction, whereas in control group there was no significance difference. Patients in experimental group maintained oxygen saturation and did not show any significance difference, while in control group there was a significant reduction in oxygen saturation rate. Practicing deep breathing exercise increases the lungs capacity, which have seen in the results. The volume of incentive spirometry was high in experimental group in post-operative phase then the patients without DBE with IS, in both the group the volume of IS had shown a significant difference from pre-operative to post-operative phase. Study [10], also reported of better lung capacity postoperatively in patient with spirometry exercises. All the patients were assessed for post-operative complications specifically presence of cough, lung sound, hyperthermia and difficulty in breathing. There were no complication developed among experimental group. Whereas, control group patients developed cough, lung sound was not clear, body temperature was more than normal and difficulty in breathing (dyspnea). Study by Wren and colleagues [11] experimented with a pulmonary care program to reduce the post-operative respiratory complications. In their program, they had included post-operative nursing intervention with IS, oral care, head elevation and educational activities. This program was found effective, similarly we trailed with pilot study including deep breathing exercise with incentive spirometer, found effective in experimental group with no post-operative complications.
5. Conclusions
- Post-operative pulmonary complications are always complicated, life threatening and creates a great financial burden on patient. In present pilot study, we found that implementing deep breathing exercise during pro-operative phase with incentive spirometer was effective in terms of enhancement of lung capacity and prevention from post-operative complications.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML