-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2017; 7(4): 84-90
doi:10.5923/j.nursing.20170704.02

Influential Components of Caring Nurse-Patient Interaction (CNPI) in a Tertiary Hospital in the Philippines: Towards Improving Health Outcomes of Patients
Anelle F. Fortuno 1, Delia B. Oco 2, Michael A. Clores 3
1Anaheim Regional Medical Center, Anaheim, CA, USA
2College of Nursing, Ateneo de Naga University, Naga City, Philippines
3College of Science and Engineering, Graduate School, College of Nursing, Ateneo de Naga University, Naga City, Philippines
Correspondence to: Michael A. Clores , College of Science and Engineering, Graduate School, College of Nursing, Ateneo de Naga University, Naga City, Philippines.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

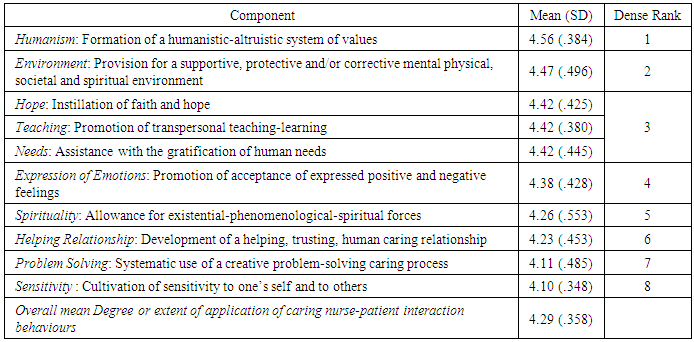
This study was conducted to explore the influential components affecting the Caring Nurse-Patient Interaction (CNPI) in the Philippine setting. It specifically determined the extent by which the nurses apply the CNPI behaviours in clinical practice and identified the influential dimensions that characterize the CNPI. This triangulated component mixed method research design used the Nurse–Patient Interaction Caring Scale (CNPI-Scale) by Sylvie Cossette, Chantal Cara, Nicole Ricard, Jacinthe Pepin (2005) and open-ended questionnaire to collect the data. Results showed that among the CNPI behaviours, those that pertains to “Humanism” (behaviours that help in the formation of a humanistic-altruistic system of values) ranked highest (M = 4.56, SD = .384). This was followed by “Environment” (behaviours that include provision for a supportive, protective and/or corrective mental physical, societal and spiritual environment) (M = 4.47, SD = .496). Qualitative data analysis showed that there are four dimensions of CNPI: “what really affects nurse-patient interaction” “what behaviours show caring nurse-patient interaction”, “realistic caring nurse-patient interaction behaviours” and “how nurses can improve caring interaction with patients”.
Keywords: Nurse-Patient Interaction (NPI), Nursing Care, Philippines
Cite this paper: Anelle F. Fortuno , Delia B. Oco , Michael A. Clores , Influential Components of Caring Nurse-Patient Interaction (CNPI) in a Tertiary Hospital in the Philippines: Towards Improving Health Outcomes of Patients, International Journal of Nursing Science, Vol. 7 No. 4, 2017, pp. 84-90. doi: 10.5923/j.nursing.20170704.02.
Article Outline
1. Introduction
- Have you ever witnessed a health care professional pushing on the abdomen of a mother whose about to give birth in an attempt to hasten the chilbirth process? All the while another health care professional is taunting the mother, “why are you crying in pain when you had a good time in making it.” You may have seen also a health care professional doing rounds in the middle of the night to avoid talking to the patients. There are also patients who had been waiting all day for a chance to talk to their nurses. How many times have you witnessed a nurse scolding the patient and family because of stress and exhaustion? These are harsh realities but are very much common occurrences that characterize nurse-patient interaction in some hospitals in the Philippines today.Caring Nurse-Patient Interaction (CNPI_ is essential to nursing practice. A high-quality level of nurse-patient interaction is defined as a therapeutic relationship with the patient wherein the nurses determine the client’s most relevant concerns, evaluate the client’s perceptions, provide venue for the client to express emotions, provide information and training to the client and family the needed self-care skills, identify the client’s needs, employ interventions to meet the client’s needs, and facilitate the client’s recovery (Videbeck, 2011).In an ideal nursing care environment, nurses tend to be more caring, reliable and responsive to the patients’ needs. The nurse should possess the following attributes: compassion, humility, empathy, commitment, cheerfulness, dedication, tact, confidence, subtlety and sincerity (Gunther and Alligood, 2002).The nurse, being the immediate influential interaction force of a patient, definitely has a great role in a patient’s total healing environment. Patients seek help from nursing staff for all kinds of reasons, such as information, reassurances, advice, or just to have a conversation (Freshwater, 2003). Nursing care means more than just giving medicines to patients. It involves so much more. Subsequently, if nurses do not have enough skills to face stressful situations or effectivelt communicate with patient and colleagues, they may lack the ability to provide outstanding patient care is at risk (Dingley, et al., 2008).Today, finding time for a quiet interaction with patients is difficult. The fast pace of the hospital setting, presence of goal driven nurses, and hospital-limiting overtime contribute to this difficulty. In addition, the possibility of lawsuits requires nurses to document every procedure, laboratory results, and various therapies, decreasing the time for nurses to talk to their patients or to help them in eating, toileting, and self-care (Smith, 2014). When patients were asked what they remembered in their hospital stay, the patients would remember their nurses well (Shattell, 2002). Although, nurses were mostly described by patients as nice, patients longed for nurses’ deeper connection with them. Patients felt that nurses do not care enough about them and just stayed away at the nurses’ station except for medication time. Also, they felt that hospital technologies and procedures totally disconnected them from the world they exist in and yearned for the nurses to communicate more with them (Coatsworth-Puspoky, 2006). In the Philippines, nurses are generally underpaid, and overburdened because of the low nurse and high patient ratio, thus, further limiting the time for quality interaction between the nurse and patient. Galvez-Tan (2005) revealed that the latest nurse to patient ratio in The Philippines is 1:50. The international standard for the ideal ratio of nurses to patient in hospitals is 1:4. Even at the Philippine General Hospital (PGH), a premiere hospital in the country, the ratio of nurse to patient average from 1:15 up to 1:25. It was also reported that in many hospitals in the Philippines, the ratio would even reach 1:50 up to 1:100 (Galvez-Tan, 2005). Many nurses in the Philippines also report of having to extend their duty hours. In an urban hospital of 100-bed capacity, nurses are only expected to be on duty for 40 hours per week. But, when no reliever is available, nurses had to be on duty for 56 hours per week, sometimes for 16 hours straight (Makilan, 2005). Despite conducting communication technique trainings, seminars, workshops, and classes to prepare and mold nurses to interact with patients effectively such as being composed, caring, and acting professionally, effective nurse-patient interaction is still overlooked as far as nurse-patient relationship is concerned. This study was conducted to explore the influential components affecting the CNPI in the Philippine setting. It specifically sought to answer the following determine the extent by which the nurses apply the CNPI behaviours in clinical practice and identify the most influential dimensions that characterize the CNPI?
2. Research Methods
- The mixed method research which is the blending of the quantitative and qualitative research designs in one single project was used in the study to determine the influential components of CNPI from the point of view of the nurses. The quantitative part of the study used the nonexperimental, descriptive design while the qualitative part of the study used the grounded theory research design to “discover theoretical precepts about social psychological processes and social structures, grounded in data” (Polit and Beck, 2012, 268). In this study, the triangulated mixed method design was used to capture the same phenomenon, with the focus on convergence and increased validity (Polit and Beck, 2012).
2.1. Participants of the Study
- All the eighteen (18) staff nurses in one tertiary hospital in Philippines participated in the study.
2.2. Research Instruments
- Two major research instruments were used to gather the data:1. Nurse–patient interaction caring scale (CNPI-Scale) by Sylvie Cossette, Chantal Cara, Nicole Ricard, Jacinthe Pepin (2005), which was originally developed to assessing nurse–patient interaction from a caring perspective. The 70-item Likert questionnaire instructed the respondents to indicate the degree or extent to which they adopt or apply the specific attitudes/behaviours in clinical practice on the scale of 1 to 5: 1 = not at all/never; 2 = not really/ rarely; 3 = undecided/every once in a while; 4 = somewhat/sometimes; 5 = extremely/ always.2. Open-ended questionnaireFour main questions were asked in the questionnaire:a. What do you think are the most important factors for a nurse to apply the CNPI behaviours? Why?b. What specific instances do you feel you are able to show CNPI behaviours to patients?c. As a nurse, what do you think are realistic CNPI behaviours?d. What possible programs or interventions do you think you need further as nurses to improve your CNPI behaviours?
2.3. Ethical Considerations of the Study
- All the participants of the study were asked to sign the informed consent form which is included in the front matter of the survey questionnaire. They were assured of anonymity and confidentiality.
2.4. Data Analysis
- To answer the first research problem which determining the degree by which the nurses apply the CNPI behaviours in clinical practice, the mean score and standard deviation of the CNPI behaviours in clinical practice were computed. Then the dense ranking of items was determined.The mean scores obtained from each of the ten (10) components of CNPI and each of the items within each component was interpreted based on the following interpretation scale:1.0 to 1.4 = not at all/never1.5 to 2.4 = not really/ rarely2.5 to 3.4 = undecided/every once in a while 3.5 to 4.4 = somewhat/sometimes4.5 to 5.0 = extremely/ alwaysThe qualitative data from the open-ended questionnaires were analyzed following general analytical steps suggested by Polit and Beck (2012) and he grounded theory approach described by Bernard and Ryan 92010). The result of the bottom-up method emerges from the process of data collection, coding and analysis. Constant comparative method of analysis was used to determine data saturation and identify core categories and central themes. An audit trail of the data as a form of validation was conducted by the third author.
3. Results and Discussion
3.1. Extent by which the Nurses Apply the Caring Nurse-Patient Interaction (CNPI) and Behaviours in Clinical Practice
- The CNPI behaviours that pertains to “Humanism” (the behaviours that help in the formation of a humanistic-altruistic system of values) ranked highest (M = 4.56, SD = .384) indicating that this the most extremely applied component. This is followed by “Environment” (behaviours that include provision for a supportive, protective and/or corrective mental physical, societal and spiritual environment) (M = 4.47, SD = .496) (Table 1).Three sets of behaviours ranked third, such as “Hope” (which is the instillation of faith and hope) (M = 4.42, SD =.425), “Teaching” (which refers to the promotion of transpersonal teaching-learning) (M = 4.42, SD =.380), and “Needs” (which are about assisting the patients with the gratification of human needs) (M = 4.42, SD =.445) (Table 1).The most applied CNPI behaviours are “showing the patients with respect—as well as to those closest to them” and “encouraging them to speak their thoughts and feelings freely” (M =4.77). The next set of behaviours includes “not having a scandalized attitude,” “showing that they will be there for them if they need me,” “respecting their privacy (e.g., do not expose them needlessly)” and “helping them with the care they cannot administer themselves” (M = 4.69).On the other hand, the CNPI behaviours which obtained the lowest mean scores indicating that these are only sometimes applied by staff nurses are the following: “asking the patients how they would like things to be done,” “helping the patients to see things from a different point of view” and “helping them to look for certain equilibrium/balance in their lives” (M = 4.08). Another set of CNPI behaviours that staff nurses only sometimes applied are: “not seem busy or otherwise occupied when I am taking care of them” and “helping them to explore the meaning that they give to their health condition” (M = 4.00). “Helping the patient to channel their difficult emotions” is also only sometimes applied (M =3.85). The CNPI behaviour which obtained the lowest mean score in terms of extent of application is “making the patients aware of the way those closest to them are experiencing their situation” (M = 3.69).
|
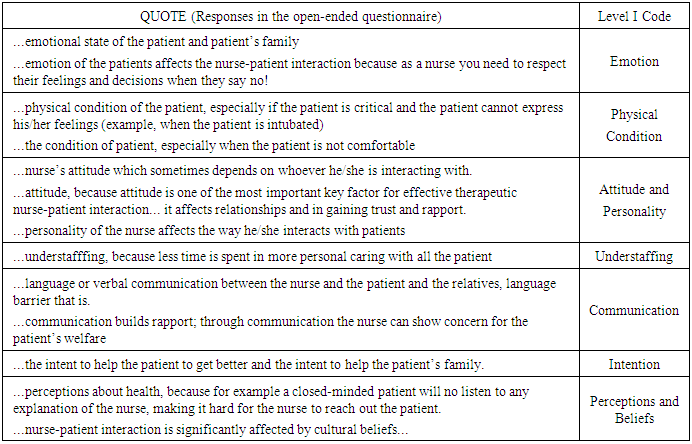
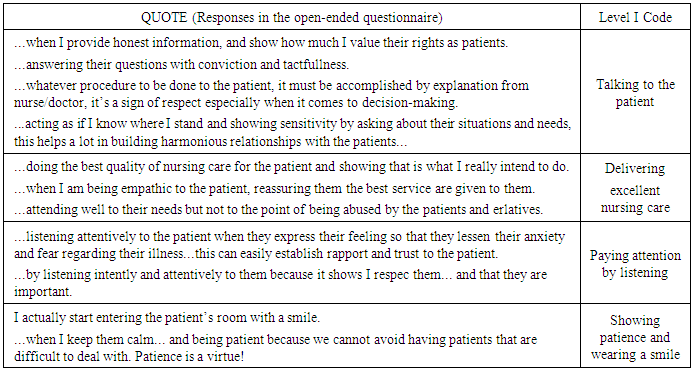
3.2. Dimensions of the Influential Components of Caring Nurse-Patient Interaction (CNPI)
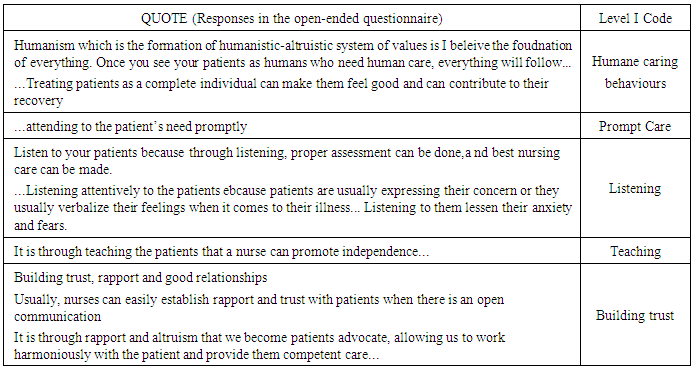
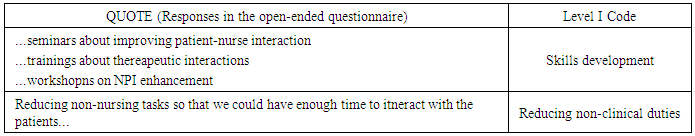
- As depicted in Figure 1-4, there are four dimensions of the influential components of CNPI: “what really affects nurse-patient interaction,” “what behaviours show caring nurse-patient interaction,” “realistic caring nurse-patient interaction behaviours,” and “how nurses can improve caring interaction with patients”. Each dimension was inferred from level I codes (or themes) which were derived from thorough analysis responses of the staff nurses in the open-ended questionnaire. Excerpts of the typical responses which were used to generate themes and categories are presented in Tables 2-5 below.
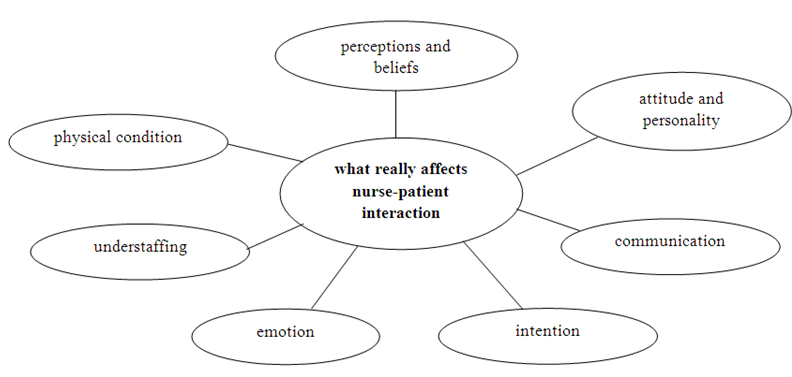 | Figure 1. Collapsed level I codes into level II code of “what really affects nurse-patient interaction” based on the Grounded theory analysis of nurses’ responses in the open-ended questions |
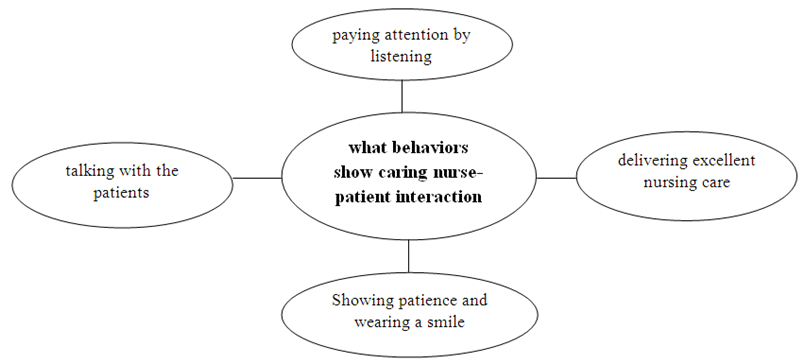 | Figure 2. Collapsed level I codes into level II code of “what behaviours show caring nurse-patient interaction” based on the Grounded theory analysis of nurses’ responses in the open-ended questions |
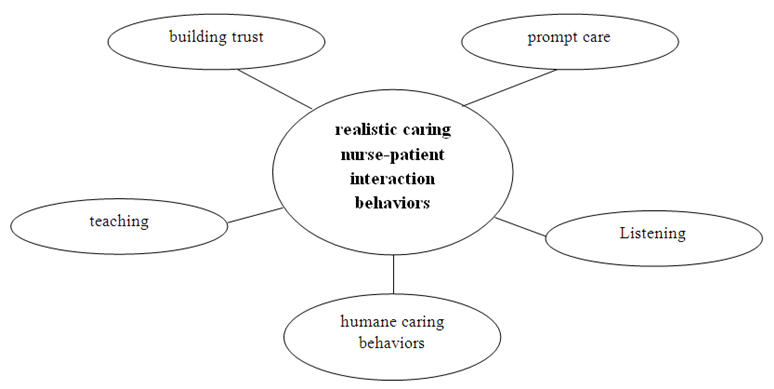 | Figure 3. Collapsed level I codes into level II code of “realistic caring nurse-patient interaction behaviours” based on the Grounded theory analysis of nurses’ responses in the open-ended questions |
|
|
|
|
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML