-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2016; 6(4): 103-107
doi:10.5923/j.nursing.20160604.03

Use of StatSeal Advanced Disc to Decrease Time to Hemostasis in Transradial Cardiac Procedures/ A Quality Improvement Project
Helen Condry 1, 2, Cesar Jara 3, 4
1Instructor, Institute of Nursing & Health Sciences, Eastern Florida State College, Palm Bay, FL, USA
2Interventional Prep & Recovery, Holmes Regional Medical Center, Melbourne, FL, USA
3Interventional Cardiologist, Health First Medical Group, Melbourne, FL, USA
4Volunteer Faculty at University of Central Florida and Florida Institute of Technology, FL, USA
Correspondence to: Helen Condry , Instructor, Institute of Nursing & Health Sciences, Eastern Florida State College, Palm Bay, FL, USA.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: A quality improvement project to evaluate the difference in time to hemostasis for radial access between the standard protocol of the Terumo Band and the StatSeal Advanced Disc with the Terumo Band for reducing nursing hours. The secondary objective was to compare radial patency and vascular complications between the 2 protocols. Background: The use of transradial access for cardiac catheterization is slowly increasing in the United States and in our cardiac catherization lab. Hemostasis is achieved at our institution with the Terumo Band and up to 4 hours of pressure post procedure, under close supervision by a registered nurse. There was interest in reducing time to hemostasis to 1 hour with the combined use of the Terumo Band and the StatSeal Advanced Disc. Methods: Data was collected for 2 weeks on 23 transradial procedures with the standard protocol of the Terumo Band and then for 3 weeks on 25 procedures using the StatSeal Advanced Disc in conjunction with the Terumo Band. Results: There was a significant difference in the combined time to hemostasis for the standard protocol group (n=23) 205 +/-52 minutes versus 77 +/- 20 minutes for the StatSeal group (n=25) (p<0.01) with no statistical difference in bleeding or radial patency. Conclusions: The use of Terumo Band in conjunction with the StatSeal Advanced Disc for radial hemostasis is safe, with significant reduction in nursing hours with an expedited hemostasis for radial procedures.
Keywords: Transradial, Cardiac catheterization, Hemostasis, Angiogram, Transradial coronary intervention
Cite this paper: Helen Condry , Cesar Jara , Use of StatSeal Advanced Disc to Decrease Time to Hemostasis in Transradial Cardiac Procedures/ A Quality Improvement Project, International Journal of Nursing Science, Vol. 6 No. 4, 2016, pp. 103-107. doi: 10.5923/j.nursing.20160604.03.
Article Outline
1. Background
- Although transradial access for cardiac catheterization has been shown to be safe and effective [1, 2] the United States has lagged behind other countries in converting from femoral to the radial approach. According to the National PCI registry, the incidence of radial approach is slowly increasing and 1 in 6 percutaneous coronary intervention (PCI’s) procedures in the US are performed through the radial artery [3]. Reflecting the national trend, our institution, a 514-bed tertiary referral center with a six-room cardiac catheterization lab has also increased transradial procedures from less than 10% in 2015 to 15% in 2016. The cardiac catheterization lab performs 2600 diagnostic and interventional procedures per year, both inpatients and outpatients. Radial access hemostasis is achieved with several different devices. A large, randomized study in China compared 2 different methods of radial artery hemostasis post transradial PCI [4]. Three hundred patients were treated with a radial artery compression device called the Terumo (TR) Band (a dual compression balloon device) and 300 patients were treated with a chitosan-based pad (a carbohydrate derivative chitin). Their study found a significant difference in compression time and lower rates of radial artery occlusion favoring the chitosan-based pad [4]. A randomized study that compared the TR Band and the Radistop compression device (compression pad with wrist immobilizer) after PCI with 749 patients found no difference in complications between the 2 devices but did find more discomfort with the Radistop and a significant increase in time to hemostasis with the TR Band [5]. Another non-randomized study compared 2 hemostatic devices, the TR Band and the Hemoband (tourniquet style band with molded compression pad) after 500 diagnostic catheterizations. They found significantly less radial artery occlusion with the TR Band [6].A hospital in New Zealand conducted a non-randomized study with 100 diagnostic catheterization patients accelerating the time to removal of air from the TR Band from 2 hours to 1 hour [7]. Although they did find a significant difference in time to hemostasis, the incidence of oozing was 17% in the accelerated group compared to 4% in the normal protocol. A retrospective study done in 2007 compared 3 different compression adjuncts including Statseal powder (called Quick Relief Powder in 2007) on arterial, venous, and arteriovenous dialysis access procedures [8]. It found the Statseal powder to be superior in reducing manual compression time with no difference in vascular complications [8]. This study did not evaluate radial access sites. Radial artery hemostasis is achieved at our institution with the TR Band. We follow the manufacturers guideline, which consists of 2 hours inflation for PCI’s and 1-hour inflation for diagnostic procedures, with at least 1 more hour for deflation. In spite of several studies showing that radial access decreases nursing workload compared to the femoral approach [9, 10], we found that the increase in radial access put a strain on our nursing staff. Our institutions’ policy mandates that all patients must remain in the recovery area until the band is deflated (some cases up to three to four hours), paradoxically at times taking longer for discharge or transfer than the femoral approach. There was interest in reducing time to hemostasis to 1 hour with the combined use of the TR Band and StatSeal Advanced Disc. Hemostasis with both devices in combination can shorten the time of recovery and observation with a standard protocol of 1 hour for both diagnostic and interventional cases. The disc is a compressed mixture of hydrophilic polymer and potassium ferrate that seals both access tract and puncture site and works independent of the clotting cascade (http://statseal.com/index.php/statseal-advanced). The disc is centered over the insertion site and covered with a transparent dressing. The TR Band is then secured around the wrist and inflated with 8ml of air prior to removing the arterial sheath. See figure 1 for radial site with a TR Band and figure 2 for a radial site with a Statseal Advanced Disc and TR Band.
 | Figure 1. Radial site with TR band |
 | Figure 2. Radial site with Statseal Advanced Disc and TR Band. Photos by Tifton Fordham, RN of Biolife, LLC |
2. Objectives
- The primary objective in this quality improvement project was to evaluate the difference in time between hemostasis using the standard protocol of the TR Band and the StatSeal Advanced Disc in conjunction with the TR Band with the ultimate goal of reducing nursing hours. The secondary objective was to report and evaluate the incidence of vascular complications of bleeding and hematomas as well as evaluating radial patency.
3. Method
- Data was collected on all patients for transradial cardiac catheterization for a 5-week period. Data was collected on 18 diagnostic cases and 5 PCI’s for a total of 23 patients using the right radial approach with the standard TR Band protocol for 2 weeks in April of 2016. Following the manufacturer’s application guidelines, the balloon in the TR Band was filled to 18cc, the sheath removed, air was slowly released until bleeding occurred, and then an additional 1-2cc was added. Typically, 12-16cc of air remained in the TR Band when the patient arrived in recovery. Data was then collected for the next 3 weeks in May of 2016 on 13 diagnostic and 12 PCI’s for a total of 25 patients using the right radial access with the StatSeal Advanced Disc and TR Band combination. The disc was applied to the radial access site and then the TR Band was applied with 8cc air for all the patients. After 20 minutes, 3cc of air was removed, and then 5cc was removed after another 20 minutes. The TR Band was removed after another 20 minutes had passed for a total of 60 minutes for both PCI’s and diagnostic cases. Additional information also collected included patient age, sex, body mass index (BMI), platelet count, international normalized ratio (INR), and the anticoagulant used during the procedure. All patients had a Barbeau test, a combined plethysmography and pulse oximetry with return of waveform within 7 seconds checked prior to the procedure to confirm safety in using the radial artery [11]. Depending on physician preference, 27 of the combined 31 diagnostic cases received between 3000 and 5000 units of unfractionated heparin to prevent radial artery occlusion [12]. All of the PCI patients were given a weight-based dose of heparin or bivalirudin. A 5F or 6F sheath was used for all the patients. The cardiac catheterization lab staff applied the compression device and removed the sheath at the end of each case. The patients were then transferred to the recovery area. As this was a quality improvement study, IRB approval was not required. We used the Bleeding Academic Research Consortium definition for bleeding to standardize the descriptions [13]. It states that type 1 bleeding does not require any medical intervention and type 2 is bleeding that requires nonsurgical intervention. More serious bleeding is designated from type 3 to 5b but no such incidences occurred in this evaluation. Radial patency was evaluated by assessing the radial and ulnar pulses both prior and after the procedure. Time to hemostasis was defined as the time it took from removal of the sheath to removal of the TR Band.
4. Results
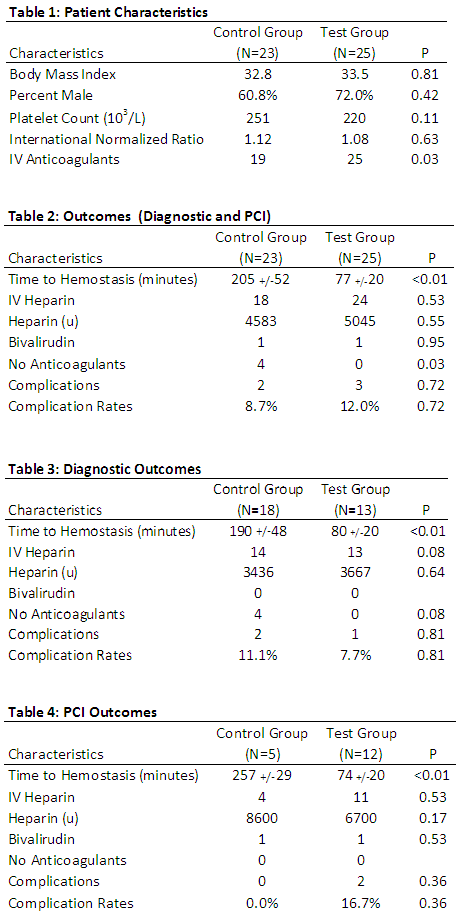
- There were no statistical significant differences in the standard protocol group compared to the test group for age, male to female ratios, BMI, platelet counts, INR, of the number of patients receiving intravenous anticoagulants. See table 1 below for demographics. Pooling the results of the diagnostics and PCI’s, there was a significant difference in the combined time to hemostasis for the control group (n=23) 205 +/-52 minutes versus 77 +/- 20 minutes for the Statseal Advanced group (n=25) (p=<0.01). See table 1. By separating the diagnostics from the PCI’s, there was still a significant difference in combined time to hemostasis in both groups. The diagnostics control group (n=18) was 190+/-48 minutes versus Statseal group (n= with 80+/-20 minutes (p=< .01). There was no statistical difference in the pooled results of bleeding and hematoma complications between the groups (p=0.708). The combined standard protocol groups had two out of 23 patients with minor type 2 bleeds that required extra balloon inflation time for an 8.7% complication rate. The Advanced Statseal groups had three type 2 bleeds but these were small hematomas (2cm or under) with a complication rate of 12%. The hematomas resolved with manual hold times of 5 minutes or less or extra balloon inflation time. See table 2. When the results were unpooled, there was still no significant difference in complications. The diagnostic control group (n=18) had 2 minor type 2 bleeds with a complication rate of 11.1% versus the test group (n=13) with 1 type 2 bleed with a complication rate of 7.7% (p=0.81). See table 3 for results. The PCI control group had only 5 subjects with a complication rate of 0%. The PCI test group (n=12) had 2 type 2 bleeds with a complication rate of 16.7% but this was still not statistically significant (p =0.36). See table 4. Radial artery patency was preserved in all the groups, confirmed with the presence of a radial and ulnar pulse post procedure. Of note, one of the patients in the diagnostic Advanced Statseal group had a femoral crossover during the PCI due to tortuosity of his artery. He had an elevated INR and developed a very large (12x12cm) hematoma in the groin post arterial sheath removal but a minor (2x2cm) hematoma in the radial area 75 minutes after the TR Band was removed. The radial hematoma resolved within 5 minutes of holding pressure but the groin hematoma required 45 minutes of manual compression, a Femostop for 2 hours, and vascular ultrasound to confirm the absence of a pseudoaneurysm.
5. Discussion
- Although Dai, and et al found fewer radial artery occlusions with the chitosan-based pad compared to the TR Band [4], our institution prefers the TR Band as the pad requires manual compression by the cardiac catheterization staff which increases procedure time and impacts the number of procedures that may be done each day.Several other studies found the TR band is favored over other hemostasis devices [5, 6]. Our institution has used the TR Band for many years without any major vascular complications but found the time to hemostasis was a burden on the nursing staff in the recovery area. There was a significant decrease in time to hemostasis with the use of the Advanced Statseal for both diagnostic cases and PCI’s. A US nursing labor costs study conducted by the KPMG Healthcare and Pharmaceutical Institute in 2011 showed that the average all-inclusive cost for a full-time hospital registered nurse was calculated to be $45 per hour [14]. Depending on the disposition of the patient, he or she could either be admitted to the nursing floor sooner or be discharged earlier, perhaps by one to two hours, saving a significant amount for our unit for each patient. The decreased time to hemostasis is especially important in cases done later in the evening so that our nursing staff does not work overtime. The new protocol treats both diagnostic and PCI patients the same, making it less difficult to recall the protocol for both the catheterization staff and the recovery staff, decreasing the possibilities of distractions and delay in discharge.PCI patients receive a larger dose of intravenous anticoagulant, a weight-based dose of heparin or bivalirudin compared to diagnostic procedures to prevent thrombus when placing a wire or stent into the coronary artery [15]. Therefore, this group of patients is at higher risk for bleeding. As the control PCI group was so small (only 5), it was difficult to compare the unpooled results. In spite of this, there was still no statistically significant difference in complications. Consequently, there was no trade in safety, with the same incidence of minor bleeding as well as radial patency post-hemostasis. The estimated rates of radial artery occlusion vary from study to study. A recent meta-analysis by Rashad et al of 66 studies found the reported rates varied from <1% to 33% [16]. The meta-analysis also recommended shorter compression times to decrease the incidence of radial artery occlusion [16]. Cubero et al [17] found that radial artery occlusion decreased significantly when the amount of air inserted into the TR Band was guided by the mean arterial pressure rather than a standard 15 ml of air. The new protocol uses a very minimal amount of air and less compression time, theoretically decreasing the likelihood of an occlusion. At our institution, we routinely check for radial artery occlusion by palpation and Doppler, but not with ultrasound. This policy is supported with a recent study that found no indications for the routine use of ultrasound to monitor for radial artery occlusion due to the low incidence [18].
6. Limitations
- This small study was completed at the introduction of the product when the staff was learning how to use the product. Therefore, it is likely that the complications will decrease in number as staff becomes proficient with the Statseal Advanced Disc. We continue to monitor complications with our quality improvement policies.This was a small sample size and was not randomized. The control and treatment groups were not concurrent to prevent the staff from confusing the 2 different protocols and contaminating the results. In addition, the PCI control group was very small making it difficult to adequately compare the two. There are no peer-reviewed studies using both the TR Band and the Statseal Advanced Disc to compare this study to although Wang, et al found the Statseal Powder to be more effective than other products [8]. Future research could evaluate the proposed 1-hour standard protocol with a TR Band and Statseal Advanced Disc combination in a randomized trial.
7. Conclusions
- As the incidence of transradial procedures increases in our cardiac catheterization lab, the burden to our nursing staff was also increasing. This quality improvement process change revealed a significant reduction in time to hemostasis to 1 hour with no significant increase in bleeding complications or radial occlusions. Saving nursing hours with an expedited radial process will decrease costs and improve throughput in the cardiac catheterization lab without compromising patient safety with a cost efficient protocol.
ACKNOWLEDGEMENTS
- We would like to acknowledge the assistance of Kelley Keene of Biolife, LLC with the statistics and table. We would also like to acknowledge Tifton Fordham, RN of Biolife, LLC for his support regarding the product and photographs.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML