Amira Refaat Said Ahmed
Obstetrics & Woman's Health Nursing Department, Faculty of Nursing, Benha University, Egypt
Correspondence to: Amira Refaat Said Ahmed , Obstetrics & Woman's Health Nursing Department, Faculty of Nursing, Benha University, Egypt.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
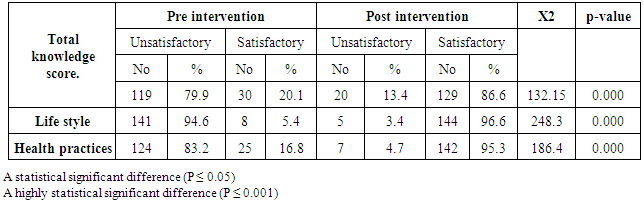
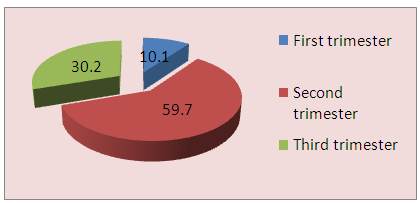
Background: Assessment of fetal wellbeing during pregnancy is very important for both mother and fetus to identify the risks, moreover is considering as a routine part of nursing care. Therefore; the nurses have an optimal role to enhance the full assessment of women during pregnancy for mother and fetus wellbeing. Aim of the study to evaluate the effect of counseling intervention on women’s knowledge, practices and lifestyle of fetal wellbeing among Primigravidae. Methods: A quasi-experimental research design was used in this the study composed of 149 primigravidae from antenatal clinic at Banha University Hospital. Data were collected using a structured interview questionnaire to assess women's knowledge, practices and lifestyle Results: the finding shows that, most of women were at the age 20 to 30 years, rural, housewives with moderate education. (59.7%) of the women were in the second trimester. There was a highly significant difference (P ≤ 0.001) after application of the counseling intervention. Moreover the majority of the women (96.6 %) follow healthy life style practices after application of the intervention. Conclusions: The study concluded that level of woman's knowledge, health practices and life style increased after application of the intervention as compared with before and most of women were satisfied after application of the intervention. Recommendations: The study is recommended that implementation of educational program for women are important to assess fetus for wellbeing during pregnancy for preventing maternal and neonatal morbidity and mortality. Enhance that periodical educational classes for pregnant women are considering a part of routine part of nursing care.
Keywords:
Fetal wellbeing, Pregnancy, Antenatal care, Counseling
Cite this paper: Amira Refaat Said Ahmed , Effect of Counseling Intervention on Women's Knowledge, Practices and Lifestyle of Fetal Well-being among Primigravidae, International Journal of Nursing Science, Vol. 6 No. 4, 2016, pp. 87-93. doi: 10.5923/j.nursing.20160604.01.
1. Introduction
Assessment of maternal and fetal wellbeing begins at the initial antenatal visit and continues throughout the pregnancy. The initial visit is an ideal time to screen for factors that might place the woman and her fetus at risk for problems such as preterm labor, birth defects, low birth weight and other preventable health problems. Moreover it considers an optimal time to begin by educating and counseling the woman about physiological changes which occur during pregnancy that will affect her life [1]. There are many complications can develop during pregnancy and can affect maternal and fetal wellbeing as well as pregnancy outcome. The abortion is the most common complication occurs at early pregnancy and in approximately 25% of pregnant women [2]. However; health education and counseling of the pregnant woman and her partner are very important to ensure health outcomes for mother and her infant. Therefore pregnant women and their partners frequently have many of questions, misinformation, or misconceptions and beliefs about what to eat, weight gain, physiological & psychological discomforts that occur during pregnancy, travelling, drug and alcohol use, sexuality, and the birthing process [3]. Moreover, a pregnant woman has the rights to participate in decisions involving her well-beings. Understanding women’s perspectives and experiences of antenatal care services is particularly critical as engagement of women in care is important for enhancing effectiveness of healthcare delivery through encourage their to be aware of and report changes in fetal activity and making antenatal care services more responsive to women’s needs and expectations [4]. Counseling intervention plays crucial role for women and their partners in the childbearing period of their lives in providing information to allow the woman and her partner to make an informed decision about assessment of fetal wellbeing. Supporting women and their families through encourage her to allow time to answer questions, provide anticipatory guidance and counsel during the pregnancy and to make appropriate community referrals to meet the needs of these women to address these issues and foster the overall well-being of pregnant women and their fetuses [5]. Significance of the study: Various complications can develop during pregnancy which may affect maternal and fetal wellbeing as well as pregnancy outcome. Maternal assessment for fetal wellbeing during pregnancy and adequate prenatal care is very important to identify fetal welling by detecting any abnormities of the fetuses such as intrauterine injury and death so that intervention and delivery at the expected date can prevent progression to stillbirth. Ideally, antenatal monitoring and follow up would decrease fetal death without putting large numbers of healthy fetuses at risk as preterm labor and the associated morbidity and mortality [6]. Therefore, the present study aims to highlight the importance of assessment for fetal wellbeing among primigravidae. ObjectivesThe study aims to study the effect of counseling intervention on selected antenatal care among primigravid women. This aim was attained through:-- Assessing the level of knowledge, health practices and life style among primigravidae before counseling intervention.- Identifying the level of knowledge, health practices and life style among primigravidae after counseling intervention.- Evaluating the effectiveness of counseling intervention among primigravidae.
2. Subgects & Methods
Research design A quasi experimental study design is used to carry out this study to examine the effect of a counseling intervention on knowledge, health practices and lifestyle regarding assessment of fetal wellbeing among primigravidae. Setting of the study: The present study is carried out among women at antenatal clinic in Benha University Hospital.The hospital receives large numbers of women each month who seek care for follow up during pregnancy from different areas (urban & rural area). Almost the hospital receives about 500 primigravidae women annually who seek care during pregnancy (from official records). Sample of the studyThe total sample consisted of 149 primigravidae selected by convenient sampling techniques among those attending the antenatal care clinic. All women were chosen according to the following selection criteria: - Primi gravidae.- Can read and write.- No past or present history of medical disorder. Tools of data collection Two tools were used to collect the necessary data about the study subjects as follows: Tool I: Interviewing questionnaire: Designed in Simple language Arabic by the investigator. It included the following sections: Part 1: Socio-demographic data such as age, weight, height, duration marriage, education level, marital status, occupation, monthly income and gestational age in weeks.Part 2: It consists of 11 questions about medical history. Part 3: It consists of 23 questions related to knowledge about antenatal care: objectives (aims), importance of monitoring fetal growth, movement & assessment of fetal wellbeing, balanced diet, weight in each antenatal visit, immunization, ultrasonography and warning signs during pregnancy in addition to health practices about nutrition, dental care, supplementation intake, rest and sleep.• The women's total score of knowledge was classified as the following:▪ Adequate: ≥ 60% of total score.▪ In adequate: < 60% of total score.• The women's total score of practices was classified as the following:▪ Satisfactory: ≥ 60% of total score.▪ Unsatisfactory: < 60% of total score.Tool II: Modified likart scale sheet, which included statements about woman's life style regarding pregnancy, it consists of 20 items. The degree of satisfaction was scored as follow:- 3 degree if the response in answering the question was correct. It was considered “a positive attitude”.- 2 degree if it was “sometimes”- 1 degree if it was incorrect. It was considered “a negative attitude”. • The women's total score of attitude was classified as the following:▪ Positive attitude: ≥ 60%▪ Negative attitude: < 60%Methods:The study was carried out after gaining the necessary approval from the director of Benha University Hospital & chairman of obstetrics & Gynecology department through a formal letter from Dean of Faculty of Nursing at Benha University, data were collected through 6 months period (from the first of July 2013 to the end of December 2013). The objectives of the study were explained to women. The investigator ensured that the research work does not affect or delay the work in the clinic. All primigravidae attended ante natal care was recruited in this study. The investigator started by introducing herself, explaining the purpose of the study and obtaining verbal consents, as well as the main items and procedures to be covered. The women were assured that all information will be confidential and will be used only for the purpose of the research. Women interviewing for three days per week from 9am to 1pm. Thereafter the questionnaire was completed by the investigator and pregnant women were instructed to freely talk with the investigator to express her feelings about the pregnancy. The time taken to complete questionnaire was 25-30 minutes. Each woman was advised to report immediately any danger signs that denote physical and psychological complications in relation to pregnancy; the women were asked to attend the follow-up scheduled visits according to the gestational age.Pilot studyA total of 15 women (10 % of the total sample) were recruited for the pilot study to test the research feasibility, clarity, and objectivity of the tools as well as to estimate the time needed for data collection. Piloting indicated that the tools of data collection are feasible, the interviewing questionnaires were clear for women and these women are excluded from the sample.Statistical design: The collected data were coded and verified prior to computerized data entry, and then all data of questionnaire were computerized, revised, categorized, tabulated, and statistically analyzed. Statistical analysis was performed with the SPSS VER 20.0 for windows statistical package presented in descriptive and association form [i.e. frequency, percentage, and mean + standard deviation (SD)]. Statistical significance was ascertained using the chi-square test (x2) for differences in qualitative variables at 95% confidence interval (CI) were computed. A P-values of (P ≤ 0.05) was considered statistically significant, and highly significant when P- values was less than or equal (P ≤ 0.001).
3. Results
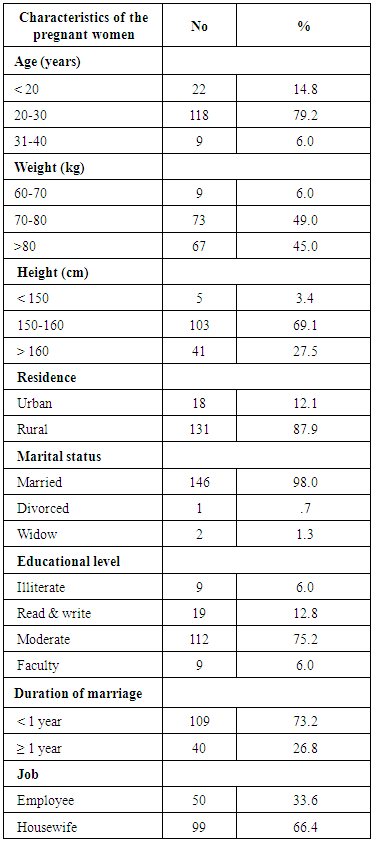
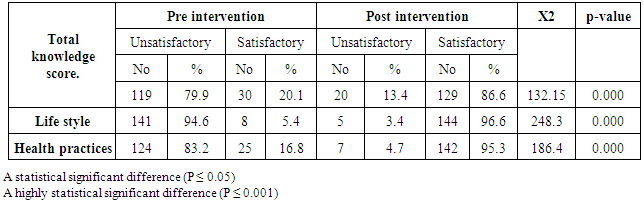
Table (1): shows that, (79.2 %) of sample were between 20-30 years, about (49.0%) of women were between 70-80 kilograms, while (69.1%) of them were between 150-160 cm. The majority of women live at rural areas, while (12.1%) of them live in urban area. About two thirds of studied women (66.4%) were housewives while more than half of them had enough income. About (73.2%) of women are married at less than one year. (98.0%) of women were married and about half of them had moderate education. Table (1). Socio-demographic characteristics of study sample (n=149)
 |
| |
|
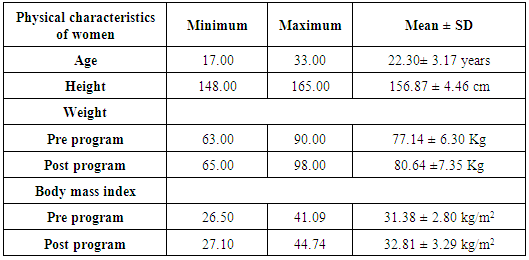
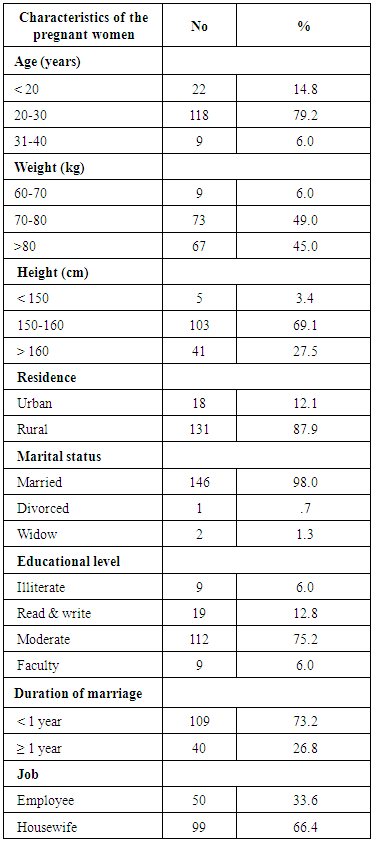
Table (2): reveals that; Mean age ± SD was (22.30 ± 3.17). Mean height ± SD was (156.87 ± 4.46) cm. Mean Weight ± SD was (77.14±6.30 Kg). Mean Body Mass Index ± SD was (31.38 ± 2.80 kg/m2) before counseling intervention. While Mean Weight ± SD was (80.64 ± 7.35 Kg). Mean Body Mass Index ± SD was (32.81 ± 3.29 kg/m2) after counseling intervention.Table (2). Mean and standard division of Physical characteristics of women measurement (n= 149)
 |
| |
|
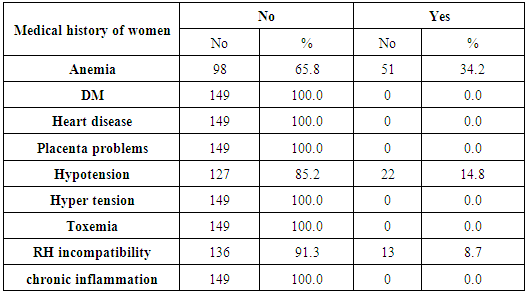
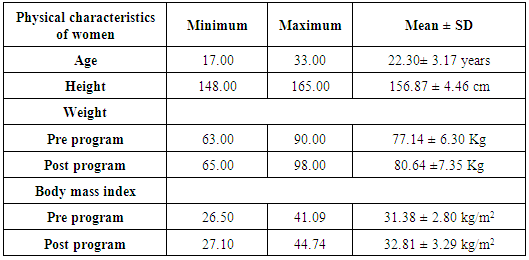
Table (3) reveals that, (34.2%) of studied women had anemia, while (14.8%) of them had hypotension, and (8.7%) of them had RH incompatibility.Table (3). Medical history of studied women (n=149)
 |
| |
|
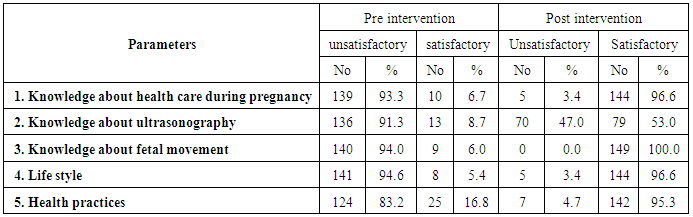
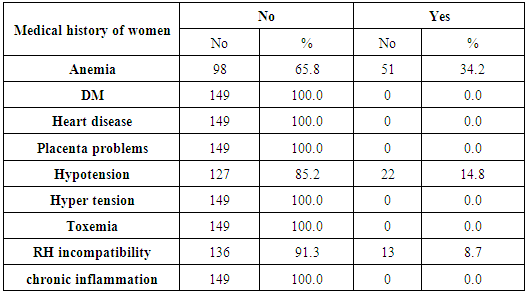
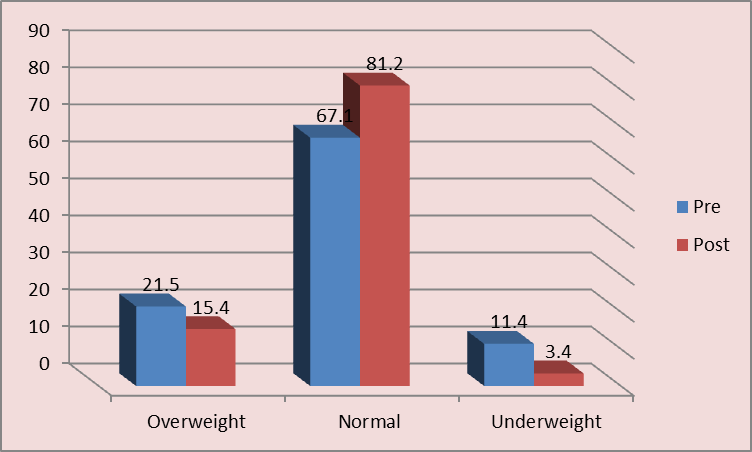
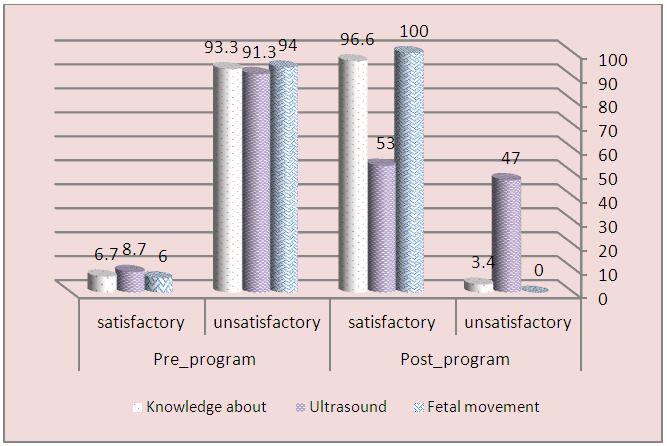
Table (4) clarifies that, most of them had inadequate knowledge (93.3%) about health care during pregnancy. (94.0%) about fetal movement, (91.3%) about ultrasonography before application of the counseling intervention. and also most of them had inadequate practices regarding life style (94.6%) and health practices (83.2%) as compared with after application of the counseling intervention.Table (4). Distribution of the study sample knowledge regarding health care during pregnancy
 |
| |
|
Table (5): reveals that, there was a high significant difference regarding their knowledge, health practices and life style after application of the counseling intervention as compared with before application of the counseling intervention (p < 0.001).Table (5). Comparison of the study sample total scores (n=149)
 |
| |
|
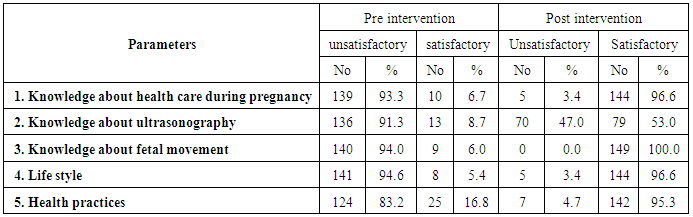
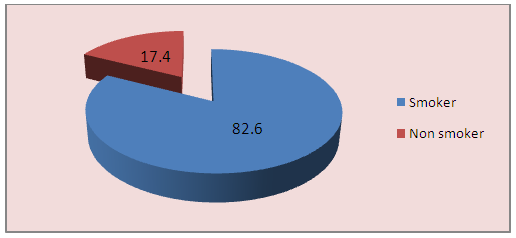
 | Figure (1). Frequency distribution of studied sample regarding body mass index pre and post intervention |
 | Figure (2). Percentage distribution of studied women regarding gestational age |
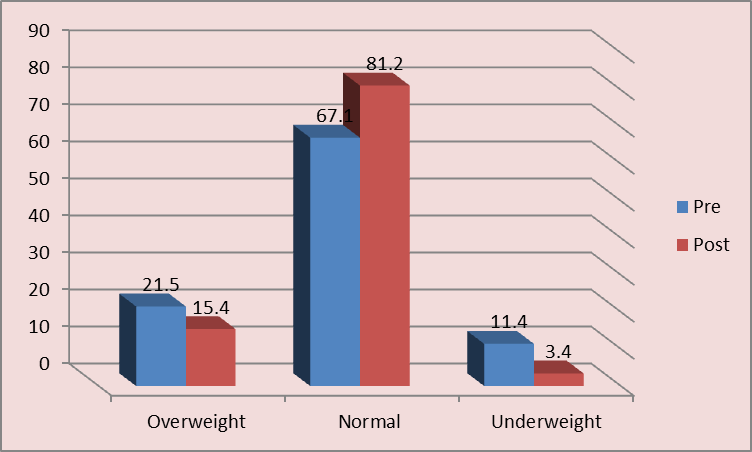
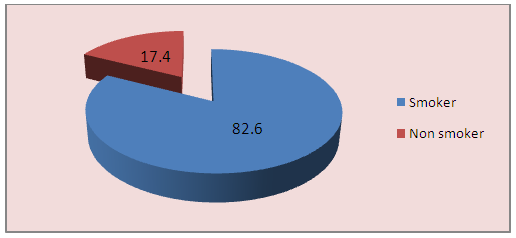
 | Figure (3). Percentage distribution of studied women regarding husband smoking |
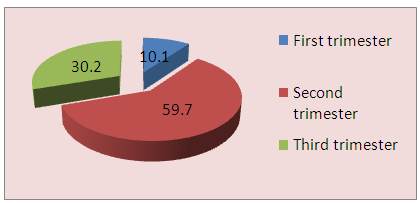
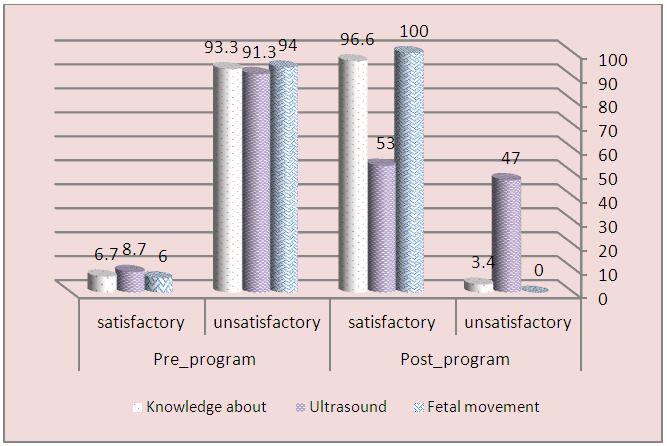 | Figure (4). Frequency distribution of studied women regarding knowledge about ultrasound and fetal movement |
4. Discussion
The prenatal assessment for maternal and fetal wellbeing focuses on the relationship between nurse- woman to develop an atmosphere conducive to interviewing, support, education and counseling. Because many women are excited and anxious at the first ante-natal visit, the initial psychosocial-cultural assessment is general. The prenatal education includes fetal growth and development, prenatal maternal exercise, Physiologic and emotional changes, nutrition and healthy eating habits, Teratogens and their impact on the fetus, rest sleep and danger signs that may occur during pregnancy [7]. The results of the present study showed that (81, 2%) of women after intervention were body mass index within normal as compared with pre intervention. This result agrees with Rasmussen and Yaktine, reported that pre pregnancy body mass index (BMI) is an independent predictor of many adverse outcomes of pregnancy. overweight throughout the reproductive cycle are related to short and long term maternal health risks, including obesity, gestational weight gain, diabetes, dyslipidemia, and cardiovascular diseases [8]. To improve maternal and child health outcomes, women should weight within the normal BMI range when they conceive. High rates of overweight and obesity are common in population subgroups already at risk for poor maternal and child health outcomes, compounding the need for intervention. In the present study, most common health conditions of primigravidae had anemia (34.2%), hypotension (14.8%). This result agrees with Chowdhury, et al who reported that anemia is the commonest hematological disorder that occurs in pregnancy. The most common cause of anemia in normal pregnancy, the hemoglobin concentration becomes diluted according to the increase in the volume of circulating blood. Lack of iron anemia during pregnancy caused by caused by folic acid deficiency, also reported that 80% of pregnant women are anemic because most of them from low socio-economic groups, so iron and folic supplementation are indicated during pregnancy to prevent iron deficiency and folic acid deficiency anemia [9]. The results of the present study showed that most of pregnant women reported that their partners were smokers. This result is in agreement with Anita, who reported that toxic substances from passive (second hand) smoke cross the placenta to affect the fetus directly, putting the fetus at increased risk for neonatal and perinatal morbidity and mortality and also suggests that the pilot intervention is a promising approach that health care institutions and health care providers can use to help educate and empower pregnant women to reduce passive smoking at home and in the workplace [10].As regards women's knowledge regarding health care during pregnancy, most of women had inadequate knowledge (93.3%) about antenatal care during pregnancy. (94.0%) about fetal movement, (91.3%) about ultrasonography before application of the intervention before application of the intervention. and also most of them had inadequate practices regarding life style (94.6%) and health practices (83.2%) as compared with after application of the intervention. This result is in agreement with Ugwu, et al who confirmed that mothers have deficient knowledge on the normal physiologic change that occurs during pregnancy. Most of women expressed that it is important to feel the fetal movements, because this is a sure sign that the fetus is alive, more over added that the significance of fetal movements as an indication that the fetus is growing well which is not the accurate reason for perceiving fetal movement [11].Moreover, Zachary, et al stated that many pregnant women may lack vital information that could contribute to a healthy pregnancy such as counseling, physical activity, and nutrition during pregnancy [12].In addition, the women in developing countries request for determination of the sex & position of the baby, expected date of delivery, and the reassurance that the baby is in a good healthy condition, from these expectations suggested that all this limitations due to poor health education and counseling [13].This trend has been reported by Erica and John, who said that; Fetal movement counting is an evaluation & non-invasive method of screening that indicator of fetal well-being which all pregnant women can easily count the fetal movements they feel between 16 and 20 weeks’ gestation. Decreased fetal movement alerts her of a deteriorating fetal condition, hence she can then bring to health care providers who can evaluate further and intervene as needed to prevent asphyxia & fetal death. Because it can be performed each day, or multiple times daily, it has advantages than other fetal tests which cannot practically be performed this frequently. This may be due to most of mothers during pregnancy had ignorance of prenatal education & counseling, inadequate services and low socioeconomic status [14]. Moreover; Deierlein, et al, mentioned that Physical activity during pregnancy is very important for woman’s overall health status. Accordingly, in a low-risk pregnancy, moderate physical activity does not increase risk of early pregnancy loss, low birth weight, and preterm delivery [15].The maternal healthy diet and lifestyle modification effect on the long-term health of the maternal and her infants [16]. This may be due to a healthy lifestyle includes regular physical activity and avoidance of harmful practices. However; pregnant women report very low levels of counseling about gestational diabetes mellitus, physical activity, and nutrition the majority of health care providers reported counseling patients on gestational diabetes mellitus, physical activity, and nutrition and were able to identify appropriate gestational diabetes mellitus for patients with obesity [17]. In the present study there was a high significant difference regarding knowledge, health practices and life style after application of the counseling intervention as compared with pre application of the counseling intervention (p<0.001). This is considered a high rate of satisfaction and it might lead to save mother & fetus and which have a positive implication on woman's perception regarding fetal wellbeing. This trend has been reported by Sujatha et al, who showed that a significant difference in the level of knowledge on antenatal care after structured teaching program (87.0%) [18]. This may be due to increase level of awareness and best practice guidance in the sample of this study which emphasis on routine screening, testing, counseling and health education topics.
5. Conclusions
In the light of the study findings, it can be concluded that there was a statistically significant improvement in maternal’ knowledge, health practices and life style after application of the counselling intervention as compared with before, as well as the implementation of counselling intervention was effective and significantly improved women’s satisfaction after application of the counseling intervention. Furthermore, the above mentioned findings proved and supported the research hypothesis.
6. Recommendations
On the basis of the most important findings of the present study, the following recommendations are suggested: • Educating pregnant women and their families about the importance of assessment of fetal wellbeing during pregnancy, what actions they should take when warning signs or problems arise, with access for special populations of women including adolescents & old age women.• Conducting periodical educational classes for pregnant women about importance of assessment of fetal wellbeing, risk factors, and warning signs, personal hygiene, nutrition, family planning, physiological changes during pregnancy.
References
| [1] | Frieden, F. J., & Chan, Y. (2007): Antepartum care. In R. E. Rakel & E. T. Bope (Eds.), Conn’s current therapy (Section 16; pp.1169–1174), Philadelphia: Saunders Elsevier. |
| [2] | Gonzaga MA, Kiguli-Malwadde E, Francis B, Rosemary B (2009): Current knowledge, attitudes and practices of expectant women toward routine sonography in pregnancy at Naguru health centre, Uganda. Pan Afr Med J. PP; 3:18. |
| [3] | Hackley, B., Kriebs, J. M., & Rousseau, M. E. (2011): Primary care of women: A guide for midwives and women’s health practitioners. Sudbury, MA: Jones and Bartlett Publishers. |
| [4] | Sword W, Heaman MI, Brooks S, Tough S, Janssen PA, Young D, Kingston D, Helewa ME, Akhtar-Danesh N, Hutton E. (2012): Women’s and care providers’ perspectives of quality prenatal care: a qualitative descriptive study. PP; 12: 29. |
| [5] | American College of Obstetricians and Gynecologists (2010): Planning for your pregnancy and birth (6th Ed.) Washington. |
| [6] | Barker D, Barker M, Fleming T, et al. (2013): Developmental biology: Support mothers to secure future public health. Nature. PP; 504: 209–210. |
| [7] | Arenson, J., & Drake, P. (2007): Maternal and newborn nursing. Sudbury, MA: Jones and Bartlett Publishers. |
| [8] | Rasmussen KM, Yaktine AL, (2009): Weight Gain During Pregnancy: Reexamining the Guidelines. Washington, DC: National Academies Press; http://www.nap.edu/openbook. |
| [9] | Chowdhury S, Rahman M, Moniruddin (2014): Anemia in pregnancy’, Medicne Today, Volume 26 Number 01, PP. 49-52. |
| [10] | Anita H Lee (2009): A Pilot Intervention for Pregnant Women in Sichuan, China on Passive Smoking Patient Educ Couns. Author manuscript; available in PMC. |
| [11] | Ugwu A, Osungbade E, Erondu F (2009): Maternal perspectives of prenatal sonogram in a north-eastern population in Nigeria. Libyan J Med.; PP. 4:140. |
| [12] | Zachary M Ferraro Kaitlin S Boehm, Laura M Gaudet, and Kristi B Adamo (2013): Counseling about gestational weight gain and healthy lifestyle during pregnancy: Canadian maternity care providers’ self-evaluation Int J Womens Health. PP; 5:PP 629–636. |
| [13] | Stanton K, Mwanri L. (2013): Global maternal and child health outcomes: The role of obstetrics ultrasound in low resource setting. J Prev Med. PP; 1:22–9. |
| [14] | Erica O'neill and John Thorp (2012): Antepartum Evaluation of the Fetus and Fetal Well Being. Clin Obstet Gynecol. Sep; 55(3): 722–730. Available in PMC Jun 17. |
| [15] | Deierlein AL, Siega-Riz AM, Evenson KR. (2012): Physical activity during pregnancy and risk of hyperglycemia. J Women's Health; 21(7):PP.769-775. |
| [16] | Tobias DK, Zhang C, Chavarro J, et al. (2012): Prepregnancy adherence to dietary patterns and lower risk of gestational diabetes. Am J Clin Nutr; 96(2):PP.289-295. |
| [17] | McDonald SD, Pullenayegum E, Bracken K, et al. (2012): Comparison of midwifery, family medicine, and obstetric patients’ understanding of weight gain during pregnancy: a minority of women report correct counselling. J Obstet Gynaecol Can; 34(2): PP.129–135. |
| [18] | Sujatha V, Radhiga C, Sudha R, Devika K, Buela priyadarshni, Shalini R (2013): Effectiveness, structured teaching programme Primigravid women. Antenatal care and knowledge. Obstetrics and Gynecological Nursing, Sri Venkateswara, India. www.mcmed.us/journal/ijner |



 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML