-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2016; 6(2): 35-47
doi:10.5923/j.nursing.20160602.02

Ebola Preparedness and Nurses' Awareness Regarding Caring for Patients with Suspected Ebola Virus Disease
Magda M. Mohsen 1, Nahla Ashour Safaan 1, Wafaa Hassan Abdulah 2
1Community Health Nursing, Faculty of Nursing-Menoufia University, Egypt
2Adult Health Nursing, Faculty of Nursing-Menoufia University, Egypt
Correspondence to: Magda M. Mohsen , Community Health Nursing, Faculty of Nursing-Menoufia University, Egypt.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: The Ebola virus causes an acute, serious illness which is often fatal if untreated. Almost all healthcare workers are at risk for exposure to blood-borne pathogens, but nurses are the group that is most affected. The aim of this study was to examine Ebola preparedness and nurses' awareness; knowledge, intention o behave and practice, regarding care of patients under investigation of suspected Ebola virus disease in hospital wards versus outpatient facility. Design: Descriptive and analytical research design was utilized. Setting: The study was conducted at the outpatient department and in patient ward at Shebin El-Kom and Menof Fever Hospitals, in Menoufia Governorate, Egypt. Subjects: A convenience sample of 288 nurses was selected. Tool: I. Self-Reported Semi-Structured questionnaire: It was developed to a. assess the characteristics of nurses, b. nurses' knowledge, intention to behave toward Ebola Disease, the use of infection control and standard universal precaution. 2) Universal Precaution Observational Checklist: to assess nurse's practice regarding to standard Universal Precaution measures. Results: more than 80% representing the presence of Preparedness; the Availability of Infection Control Strategies/ and the use of list of prevention recommendations in the studied hospitals. Nurse's awareness on the knowledge of Ebola disease, showed that; 50% of inpatient nurses knew the Ebola disease meaning compared to 28.5% of the outpatient nurses. Regarding total Intention; 80% of inpatient nurses had positive to behave toward Ebola Virus disease. Whereas, clean infected surface with antiseptic solution 95.1% of the total studied nurses did it correctly whereas, conducting hand washing represents 64.2% of the total studied nurses who did it correctly. Conclusions: Preparedness level for the safe management of Suspected Ebola was on fair level. B).Overall, Ebola awareness was on the fair level based on the total score of knowledge, intention to behave and practice. A positive Correlation was found between Total Knowledge Score & Total Practice Score. Recommendation: All nurses are in need for continuous training for strengthening the capacity with adequate knowledge of prevention, is required, focusing on the concept of universal precautions that target all health workers.
Keywords: Ebola Hemorrhagic fever, Preparedness and Awareness, Infection control and Standard Universal Precaution
Cite this paper: Magda M. Mohsen , Nahla Ashour Safaan , Wafaa Hassan Abdulah , Ebola Preparedness and Nurses' Awareness Regarding Caring for Patients with Suspected Ebola Virus Disease, International Journal of Nursing Science, Vol. 6 No. 2, 2016, pp. 35-47. doi: 10.5923/j.nursing.20160602.02.
Article Outline
1. Introduction
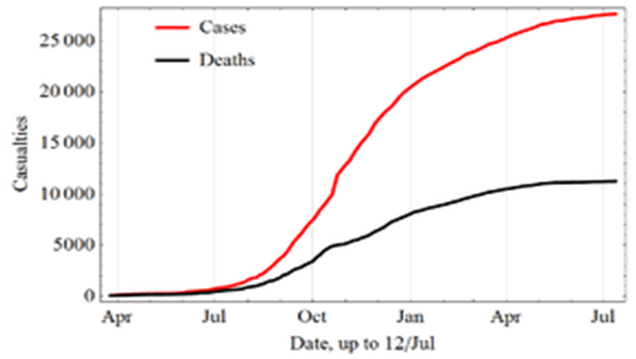
- Ebola Virus Disease "EVD" is now a major epidemic affecting most parts of West Africa, and is beginning to invade other countries as well. The international response to the Ebola outbreak was truly assertive, and needs an urgent public health intervention. Controlling the outbreak required the combined efforts of ordinary citizens, political and religious leaders, community workers, and None Governmental Organizations [1].Ebola viruses Disease "EVD" is a zoonotic infection. However, infections can also occur between humans through direct contact with broken skin or mucous membranes [2]. Ebola viruses were first discovered in 1976 near the Ebola River, from which the disease takes its name, in what is now the Democratic Republic of the Congo. The outbreaks had occurred in what are now in Nzara, South Sudan, and the other countries. Two imported cases, including one death, and two locally acquired cases in healthcare workers were reported in the United States. Ebola outbreak has spread between countries by air traveler to Nigeria and USA and by land to Senegal and Mali travelers [3].The seven countries have previously reported a case or cases imported from a country with widespread [5]. The average EVD case fatality rate is around 50%. Case fatality rates have varied from 25% to 90% in past outbreaks. Early recognition of EVD is critical for infection control. Health-care providers should be alert for and evaluate any patients suspected of having EVD [1].WHO aims to prevent Ebola outbreaks by maintaining surveillance for Ebola virus disease and supporting at-risk countries to developed preparedness plans? When an outbreak is detected WHO responds by supporting surveillance, community engagement, case management, laboratory services, contact tracing, infection control, logistical support and training and assistance with safe burial practices [6]. Preparedness of Ebola exposure was emphasized. The Preparedness Dashboard demonstrates an increase in overall preparedness at the country level from 19% (at baseline) to 62% (31 December 2015) among the priority countries. Furthermore, 11 of the 14 countries have achieved a score of 50% against the Ebola Preparedness Checklist, which signals they are equipped to test their response systems [7]. Are you as a nurse prepared to face it?Almost all healthcare workers are at risk for exposure to blood-borne pathogens, but nursing profession are the most contingent among health professionals that provide direct care to patients, making them vulnerable to the risks of biological exposure during medical practice [9-11]. It has been estimated that > 50% of nurses will experience at least one needle-stick injury in their careers [12]. The Communicable Disease Control provides guidance regarding identification and management of patients with suspected Ebola Virus Disease. The infectious virus have been reported to be present in bodily fluids such as blood, sweat, stool, urine, saliva, semen and breast milk of infected people [13, 14]. Infection can also occur if the broken skin or mucous membranes of a healthy person comes into contact with environments and items that have become contaminated with an EVD patient’s infectious fluids such as soiled clothing, bed linen, or used needles. The virus can be viable in semen up to ninety days after clinical recovery from the illness [14]. Recently, the possibility of sexual transmission has also been reported [15-17]. In healthcare settings, Ebola is spread through direct contact with blood or body fluids of a person who is sick with Ebola or with objects. Personal Protective Equipment (PPE) that fully covers skin and clothing and prevents any exposure of the eyes, nose, and mouth is recommended to reduce the risk of accidental self-contamination. All PPE must be used in the context of a comprehensive infection control that follows CDC recommendations and applicable Occupational Safety and Health, including PPE, and Respiratory Protection standards [18].The Standard Universal Precautions have been shown to reduce risk of blood or body fluid exposure among health care workers. It was shown that lack of knowledge about modes of transmission, work experience barriers to safe practice [2, 14] heavy workload, uncomfortable personal protective equipment (PPE), inaccurate risk assessment, and belief that compliance to universal precautions is unnecessary [16, 10] were associated with non-compliance to universal precautions. The Standard Universal Precautions (SUP) include specific recommendations for hand washing, appropriate waste management, use of gloves, gowns, masks, and protective eyewear when contact with blood or body secretions containing blood is anticipated. According to the Centers for Disease Control and Prevention (CDC) guidelines, universal precautions should be consistently used for all patients regardless of their blood-borne infection status [19].To protect healthcare workers, health care facilities must provide adherence to safely using personal protective equipment (PPE), and implement administrative and environmental controls with continuous safety checks through direct observation of healthcare workers [18].Hand Washing; it has been estimated that between 20-40% of all hospital acquired infections are caused by cross-infection from the hands of healthcare workers [19, 20]. Hands should be washed or alcohol-based rubs should be used between patient contacts and after gloves are removed. Hands should be washed after contact with blood, body fluids, secretions, excretions, and contaminated equipment. It may be necessary to wash hands between tasks on the same patient to prevent cross-contamination of different body sites [21-23]. A need for a preparedness plan that includes rigorous education, training and practice of any staff that directly interact with or care for patients is critical to ensure safe management of patients with EVD. In out-patient/or Emergency and Medical Admission Departments, prompt recognition and appropriate infection control management of patients with Highly Infectious Diseases [17].
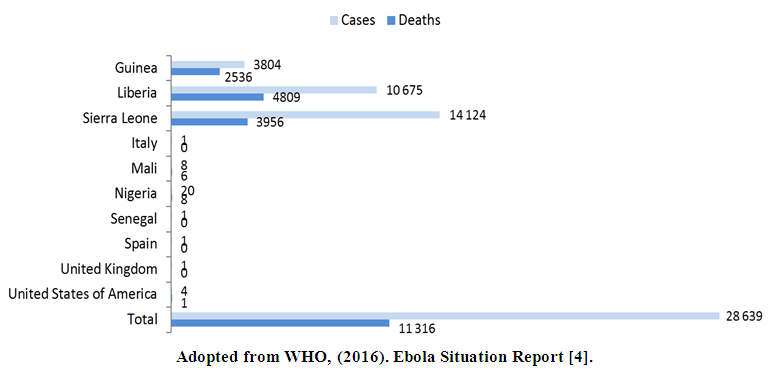 | Figure 1. Confirmed. probable, and suspected EVD cases Worldwide (data up to 13 March 2016) |
2. Aim of the Study
- The aim of this study was to examine Ebola preparedness and the nurses' awareness; "knowledge, intention to behave and practice" toward care of patients under investigation of suspected Ebola virus disease (EVD) in hospital wards versus outpatient facility.Research Questions:1. What is the level of Ebola' preparedness for Ebola suspected patients in hospital wards versus outpatient facility?2. Is the personal protective equipment in hospital satisfactory?3. What is the level of nurses' awareness; "Knowledge" regarding caring for Ebola suspected patients in hospital wards versus outpatient facility.4. What is the level of nurses' awareness "intention to behave" regarding caring for Ebola suspected patients in hospital wards versus outpatient facility.5. What is the level of nurses' awareness "Standard universal precaution practices" regarding caring for Ebola suspected patients in hospital wards versus outpatient facility?Operational Definition: Awareness: was operationally defined as common knowledge or understanding about a scientific, or social. It forms a basic concept of the theory having knowledge of, feel of, or sense of, and practice. This information is incredibly useful as intended to behave toward this information and critical transformed into performance / practice [24, 25]. Preparedness: was defined as the state of being prepared or ready, for particular situation or the Process of ensuring that the facility has complied with the preventive measures, is in a state of readiness to minimize loss of life, injury, and damage to property, and has the capability and resources to continue to sustain its essential functions [26].The main component of preparedness activities included:-Infection control protocols/strategies, the revision of protocols, the use of list of national prevention recommendations, formation of a hospital outbreak management team, the availability and use of personal protective equipments, training of nurses and other healthcare workers.
3. Subjects and Method
- Design: Descriptive and analytical research design was utilized for this study. Setting: The study was conducted at the outpatient department and in patient ward at Shebin El-Kom and Menof Fever Hospitals, Menoufia Governorate, Egypt (as they are the two main hospitals which have the largest flow of patients).Subjects:A convenience sample of 288 nurses was chosen. The sample was drawn from the two hospitals. Nurses who are working in the above settings during the period of the study were selected. Sample was selected according to the following criteria: nurses who form all level and who were agreeing to participate in the study.Calculation of the sample:The sample size was calculated to estimate the average nurses working in fever hospitals assuming average at clinics to be:-§ The total number of nurses who are working at the outpatient department and in patient ward at Shebin El-Kom and Menouf Fever Hospital, (hospital which considered reference hospital for fever cases in this area).§ With a 95% level of confidence, significance level of 0.05 and a power of 80% (error=20%). Using the Epi-info computer software program the required sample size was 250 subjects. So, the researcher increase sample size up to 288 nurses in order to overcome the drop out from the study.Tool for Data collection: Tool I. Self-Reported Semi-Structured questionnaire: It includes questions to be checked that related to personal characteristics, nurses self reported knowledge about Ebola virus Disease, Nurses' intention to behave towards patient about under investigation of suspected Ebola virus disease. It was developed and utilized by the researchers based on review of related literature. It includes the following parts:Part (1): Personal characteristics: It comprised of questions about: age, qualification, work experience, type of clinic, and nurses' job title.Part (2): Nurses' Self reported knowledge about Ebola virus Disease: It was comprised of questions related to: What is Ebola Disease? The vulnerable group for Ebola infection? Signs and symptoms of Ebola?, when the Signs and symptoms appear? When you ask for medical care? How a person infected with Ebola? Did Ebola have a vaccine against it? Did you will report to health units or center if you observe a person with suspected Ebola? What is the most important question you ask for person with suspected Ebola? What is the Mode of transmission of Ebola viruses? They were rated according to either by yes or no. Part (3): Nurses' intention to behave towards patient about under investigation of suspected Ebola virus disease (EVD) in hospital wards versus outpatient facility. It included 3 main items; test for detecting Ebola, Action to behave and Transmission of infection. They were rated according to either by yes or no. Part (4): Presence of Infection control protocols, the revision of protocols, the use of list of national prevention recommendations, blood specimen or body fluid collected in special place, formation of a hospital outbreak management team, the availability and use of personal protective equipments "PPE" and the satisfaction from hospital equipment? They were rated according to either by present and not/ yes or no.Part (5): Presence of Infection control strategies for Ebola, training program about Ebola for nurses and other healthcare workers. They were rated according to either by yes or no. Scoring system: Each question was given a score from one to three in which one indicated poor score, 2 indicate fair score, while score, 3 indicated good score. Each part of the questionnaire was collected separately to give a total percentage score that was classified into three categories as follows:Score of 60 and > means the high score The moderate score from 40 to <60 means Fair score The Low score less than 40 means poor scoreTool II. Universal Precaution Observational Checklist: It was developed by the researchers based on the current related literatures [27, 28]. This tool measures was used to assess nurse's practice regarding to standard Universal Precaution measures. It included 8 type items on various practices (hand washing, gloving, exchange gloves after finishing, clean infected surface, sterilization of instruments, eye protection, wearing gowning, protection against blood and body fluids); with responses done =1, not done =0, Scoring system: The total percentage of total practice score was classified into three categories as follows:The high score 80 and > means Good practice.The moderate score from 40 to <80 means Fair practice,The Low score less than 40 means poor practice.Procedure for data collection:Ÿ Study period: This study was conducted during the period starting from January 2015 to the end of October 2015. Ÿ An official letter from the Faculty of Nursing was delivered to the administrators of the two Fever Hospitals (Menof and Shebin El-Kom), in Menoufia Governorate- Egypt, where the data were collected to conduct the study after an explanation of the purpose of the study. The researchers introduced themselves to every participant, explain the purpose of the study and assured them that confidentiality would be maintained throughout the study then a verbal consent was obtained from each participant.Ÿ Ethical consideration: protection of nurse's rights, oral consent was obtained from nurses to participate in the study; the researchers initially introduced themselves to every participant, explain the purpose of the study and assured them that confidentiality would be maintained throughout the study. Each nurse was notified about the right to refuse to participate in the study. Anonymity and confidentiality of the information gathered was ensured.Ÿ Validity; Instruments were reviewed and tested for validity by 5 experts in medical surgical nursing and community health nursing, modification were done accordingly to ascertain relevance and completeness. Ÿ Reliability: The internal consistency of the questionnaires was calculated using Cronbach's alpha coefficients. Test-retest was used. The Cronbach’s alpha of the questionnaire was 0.94 indicate good reliability.Ÿ Pilot study, a pilot study was conducted on 10 nurses to evaluate the developed tools before starting the actual data collection. The pilot sample was not included in the total sample of the research work to ensure stability of the answers. Based on the results of the pilot study, modifications, and rearrangement of some questions were done. It also helped to estimate the time needed to fill in the questionnaire. Ÿ The time taken for every questionnaire to be completed was about 20-30 minutes for each nurse and faculty of nursing staff. Ÿ Nurses who agreed to participate in the study are requested to complete the required tool. The researchers introduced themselves to the respondents, and explained the aim and objectives of the study to the nurses in the study settings. Ÿ Then, the designed questionnaire was distributed to them, with instructions about its filling. This was repeated in each place of the study setting. The researchers were present all the time to clarify any ambiguity.Ÿ Then the preparedness questionnaire was filled out and the Universal Precaution scale was conducted.Statistical analysisUp on completion of data collection, the data collected were coded, data entry, tabulated and statistically analyzed by personal computer and statistical package SPSS version 16. Data were presented using descriptive statistics in the form of frequencies and percentages for qualitative variables and means and standard deviations for quantitative variables. Variables like nurses’ knowledge, intention to behave and practice were compared using chi-square test. Correlation analysis was used for assessment of the inter-relationships among quantitative variables. Statistical significance was considered at p-value <0.05. P value, Highly significant difference if P < 0.001.
4. Results
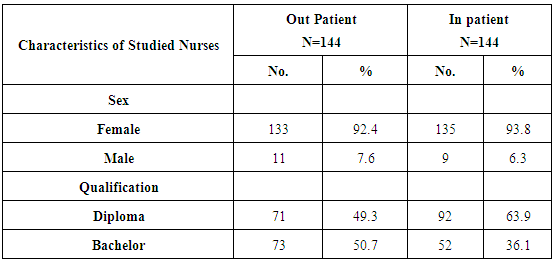
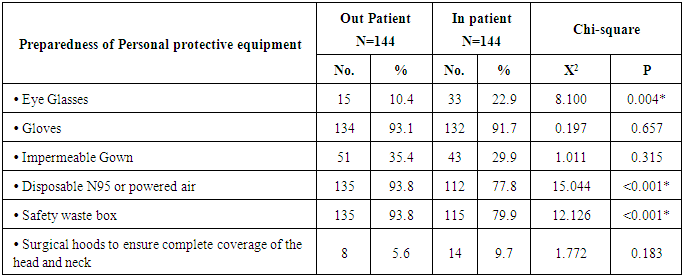
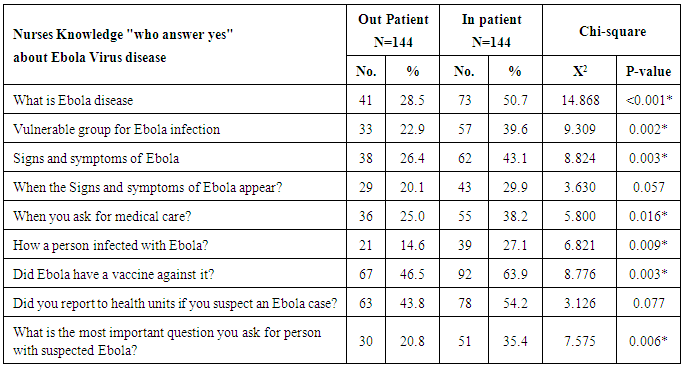
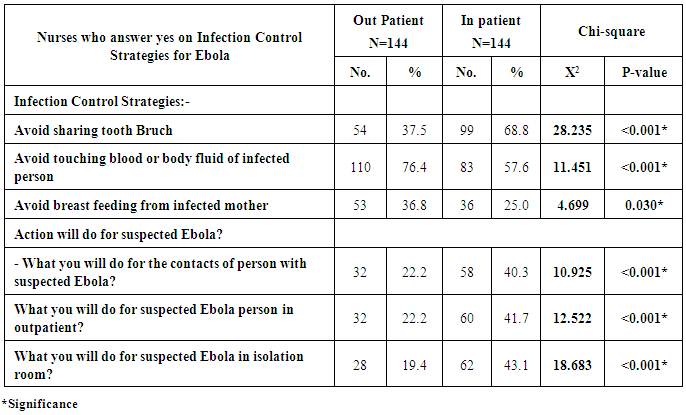
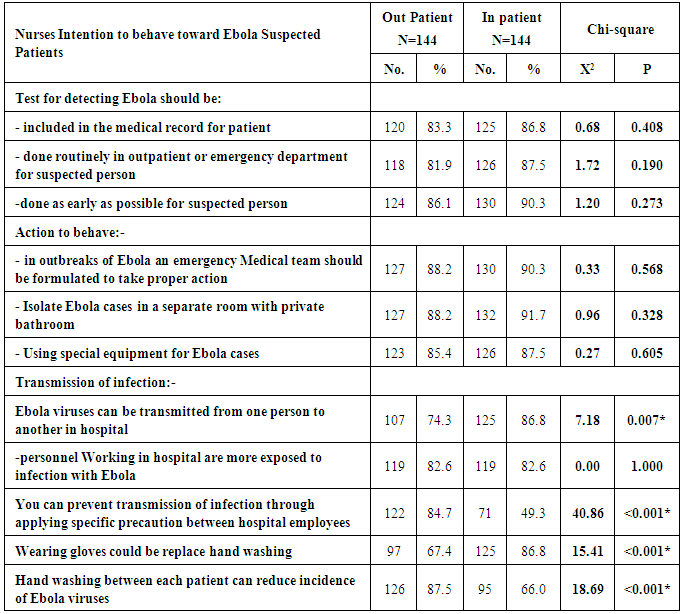
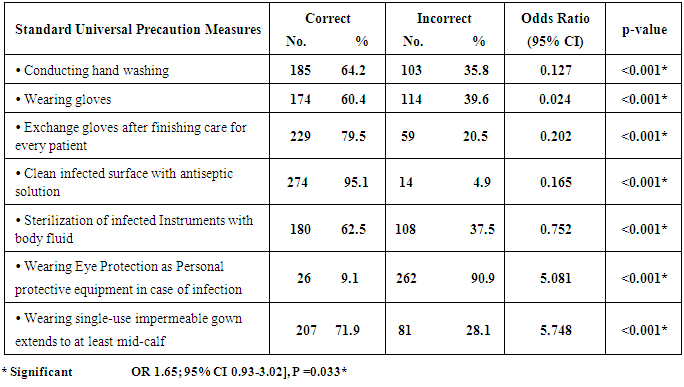
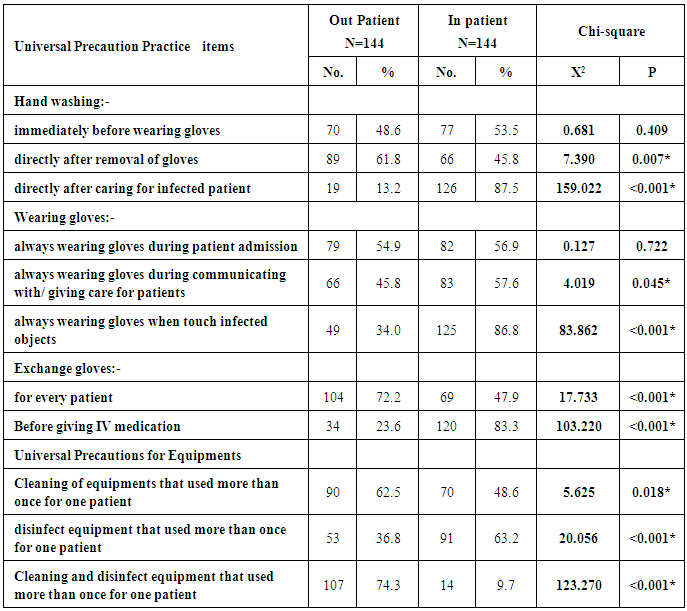
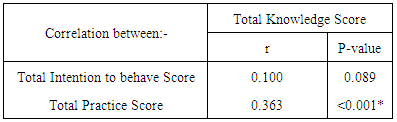
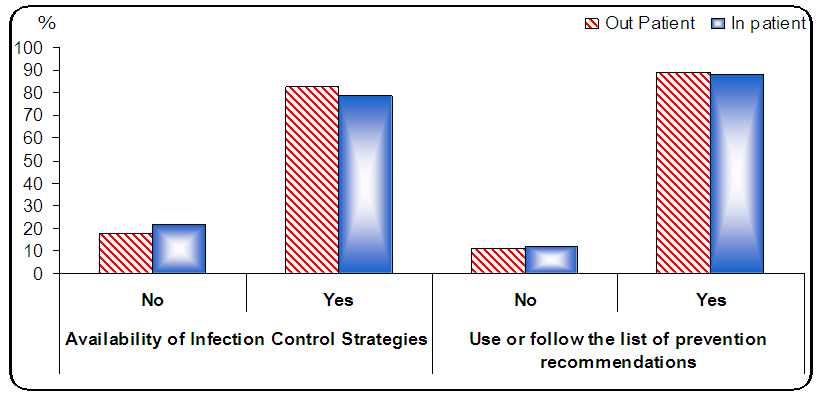
- Table (1) shows the characteristics distribution of studied nurses that; 50.7% of outpatient studied nurses have bachelor degree in nursing science compared to 36.1% of inpatient studied nurses, whereas, 92.4% and 93.8% of outpatient studied nurses and inpatient studied nurses respectively were females.Figure (3) showed the distribution of Preparedness for Ebola; the majority of nurses working in out-patient and in-patient answer yes regarding the Availability of Infection Control Strategies and also for use of list of prevention recommendations Figure (4) clearly showed that 80 % of all studied nurses took training program about Ebola Virus disease; presence of infection control strategies for Ebola and specific precaution for Ebola Table (2) clearly showed that there was a statistical significant difference between out-patient and in-patient Preparedness and the use of personal protective equipment in hospital facilities as regards "Safety waste box and Disposable N95 or powered air" P= <0.001*, whereas no statistical significant difference in the other personal protective equipment in hospital facilities. Figure (5) Studied Nurses Satisfaction with Hospital equipment. It showed that more than half of the studied nurse working in out-patient departments was mostly satisfy with hospital equipments higher than nurses in in-patient ward departments. Whereas, more than half of the studied nurse working in in-patient departments was "to some what satisfy" than nurses in out-patient ward departments. Table (3) revealed the studied nurses knowledge about Ebola disease. It shows that half of the studied inpatient nurses knew the Ebola disease meaning compared to 28.5% of the outpatient nurses with a highly statistical significant difference p=<0.001. Regarding how a person infected with Ebola? it was reveals that only 14.6% of the studied outpatient nurses, knew the source of infection compared to 27.1% of the inpatient nurses with the highly statistical significant difference p=<0.009. Figure (6) Studied Nurses who Answer Yes on the Mode of transmission of Ebola viruses. It clarified that most of studied Nurses working in in-patient as well as out-patient departments answer "yes" about the most common Mode of transmission of Ebola viruses as blood and body fluid. Table (4) shows Distribution of Nurses who answer "yes" on the Infection Control Strategies for Ebola Virus. Regarding the action the nurse will do with suspected Ebola person in outpatient or hospital reception; 22.2% of the outpatient nurses knew what to do with compared to 41.7% of the inpatient nurses with a highly statistical significant difference p=<0.001. A highly statistical significant difference was found between all items of action will be done for suspected Ebola and inpatient and outpatient nurses answers, P <0.001*.Table (5) showed the Distribution of Nurses who have a positive Intention to behave towards Ebola Suspected Patients. It reveals that 86.8 % of the inpatient nurses knew that; Test for detecting Ebola should be included in the patient medical record compared to 83.3 % of the outpatient. Also Test for detecting Ebola should be done as early as possible or emergency for suspected person compared to 81.9% & 86.1% of the outpatient nurses respectively with no statistical significant difference.As regards transmission of infection the same table shows that 86.8% of the inpatient nurses intended that Ebola viruses can be transmitted from one person to another in hospital compared to 74.3% to the outpatient nurses with a statistical significant difference p= 0.007, additionally 84.7% of the outpatient nurses can prevent transmission of infection through applying specific precaution among hospital employees compared to 49.3% of the inpatient nurses with a highly statistical significant difference p= <0.001.Table (6) showed distribution of studied nurses regarding standard universal precaution Measures in Hospital. It revealed that most of universal precaution measures in Hospital were done correctly with different percentage ranging from 95.5% till 62% for studied nurses, except for one items only; 9.1% wearing Eye Protection as Personal protective equipment in case of infection.Table (8) shows that nearly 48.6% and 53.5% of studied nurses in out patient and in patient respectively who did hand washing immediately before wearing gloves whereas, 13.2% of studied nurses in out-patient compared to 87.5% of studied nurses in-patient respectively who did hand washing directly after caring for infected patient with highly statistical significance difference, X2= 159.022, P <0.001*. Regarding wearing gloves; 86.8% of in patient studied nurses compared to 34.0% of out-patient studied nurses respectively, always wearing gloves when touch infected objects. Figure (7) showed that the total general infection control measures score among the studied nurse was fair, "mostly higher in nurses caring out-patient ward than in studied nurses caring in in-patient departments. Also the specific precaution score for Ebola was also faire, but is higher among studied nurses of in-patient than the nurses of out-patient wards. Figure (8) Overall, Ebola awareness was on the fair level based on the total score of knowledge, intention to behave and practice about Ebola Virus. Approximately half of studied nurse's working in inpatient had poor knowledge about Ebola compared to less than half of studied nurse's working in out-patient had poor knowledge in the total score of the Knowledge while studied nurse' practice was considered above average whereas the least was considered poor practice among nurses working in outpatient and in-patient ward. Table (8) revealed the Correlation between total nurses' Intention to behave score, Total practice score and total knowledge score. It showed that mean the increase of knowledge will show an increase of practice.
|
 | Figure (3). Distribution of Preparedness; the Availability of Infection Control Strategies/ and the use of list of prevention recommendations |
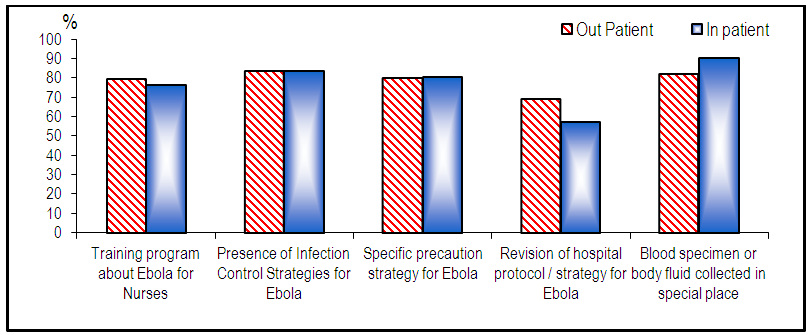 | Figure (4). Distribution of Preparedness about the presence of Ebola specific precaution measures in Hospital |
|
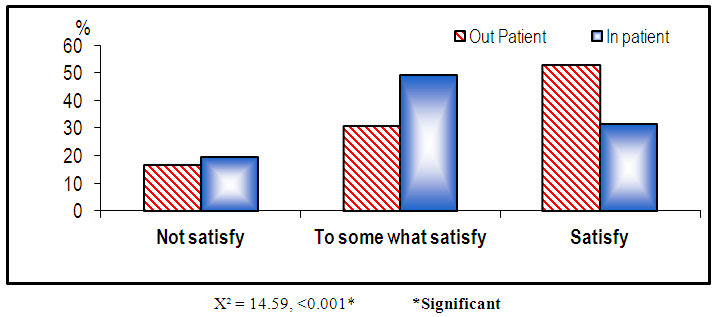 | Figure (5). Studied Nurses Satisfaction with Hospital equipment |
|
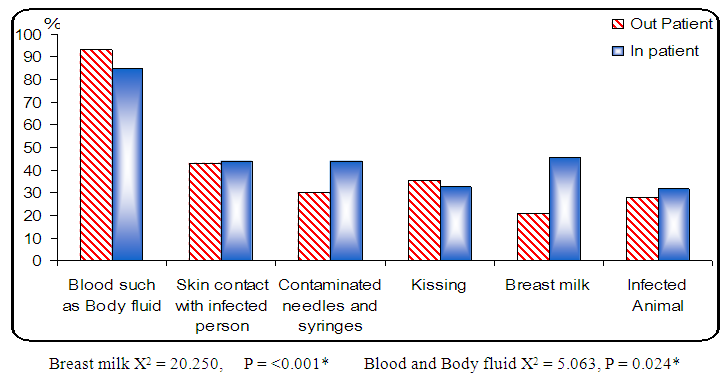 | Figure (6). Studied Nurses who Answer Yes on the Mode of transmission of Ebola viruses |
|
|
|
|
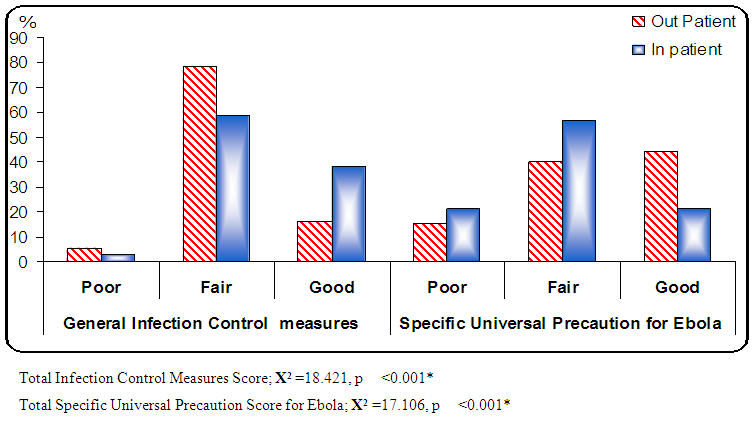 | Figure (7). Percentage Distribution of general infection control measures score and specific universal precaution score for Ebola |
|
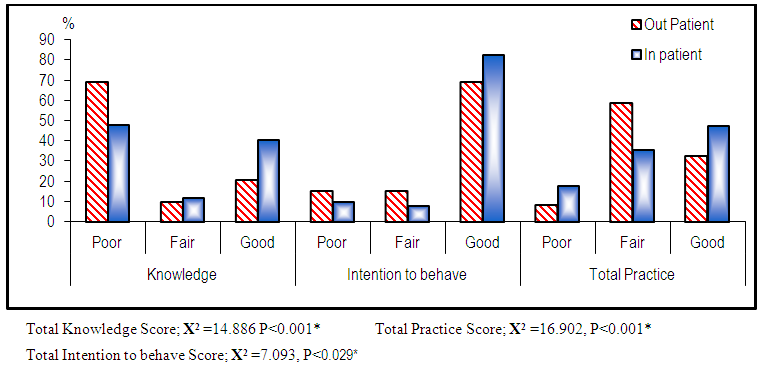 | Figure (8). Percentage Distribution awareness; "Knowledge score, Intention to behave score and practice score" among studies nurses in outpatient and inpatient wards |
5. Discussion
- Ebola virus outbreak was occurred around the world [29, 30]. Based on this epidemic, the health care workers should be aware and review the mode of transmission, clinical manifestation, diagnosis, treatment, and prevention of Ebola virus disease. Thus the aim of this study was to examine Ebola preparedness and the nurses' awareness; "knowledge, intention to behave and practice" toward care of patients under investigation of suspected Ebola virus disease (EVD) in hospital wards versus outpatient facility.All healthcare facilities should be prepared to safely manage the suspected Ebola patient presenting to their Out-Patient Departments and/or "Admission Departments. Regardless of whether a facility is able to provide ongoing care for suspect or confirmed Ebola patients, facilities should be prepared at a minimum to safely manage such patients in their out-patient departments while awaiting transfer to another facility [31]. This view was considered in the current study setting. The current study clarify that the total general infection control measures score among the studied nurse was fair, "mostly higher in nurses caring in-patient ward than in studied nurses caring in out-patient departments. Also the specific precaution score for Ebola was also faire, but is higher among studied nurses of out-patient than the nurses of in-patient wards. The current study results was in line [32], They stated that Out-Patient Departments and/or "Admission Departments" are high-risk areas for disease transmission in hospitals, since they are overcrowded, and potentially infectious patients and susceptible individuals may wait in close proximity for several hours. Moreover, the identification and isolation of potentially infectious patients may be delayed, because of high work burden, lack of specific training and skills, or unavailability of adequate isolation procedures or areas. Whereas, [33, 34] added that in particular, Highly Infectious Diseases, pose a special risk for nosocomial outbreaks, if not adequately isolated and appropriately managed Regarding the availability of infection control strategies/protocol, the current study revealed that it is mostly available, also mostly for the use and application of list of prevention recommendations was assured. Also 80% of studied nurses took training program about Ebola Virus disease; they mentioned that they knew the specific precaution strategy for Ebola. This was contradicted with [35]. They found that half of the nurse participants opined that their workplace had not provided proper training for nurses to care safely for confirmed EVD patients. Nurse perceptions also revealed opportunities for improvement in the workplace for the training of nurses and ancillary service staff to safely provide care for patients. The current study result and the later result was inline with [7]. They developed preparedness for optimum Infection Prevention and control "IPC" capacity, to ensure safe working conditions within healthcare facilities. They emphasized on Strengthen infection prevention and control with basic hygiene, sanitation, disinfection, PPE, and services, Equip and adequately train health-care workers with priority for those in first contact with patients and at all isolation units and treatment centers.Considering the personal protective equipments "PPE" use in hospital facilities, [36] concluded that all healthcare workers involved in care of EVD patients should wear personal protective equipment for protection of healthcare workers and prevention of spread. The result of current study revealed that, mostly of studied nurses from Out-Patient facility and in patient wards usually wears gloves, compared to few of studied nurses from in patient wards and studied nurses from Out-Patient facility usually wear Glasses. The Current study was congruent with [27] who pointed out that; to protect healthcare workers they should adherence to safely using PPE. Also [7] develop a preparedness plan that provides specific information on procedures and protocols to be used in hospital or healthcare setting for identifying and caring for a patient with suspected Ebola Virus Disease (EVD).Standard universal precautions are strategies for protecting healthcare professionals from occupational transmission of organisms. Given that, all body fluids and secretions with the exception of sweat should be considered potentially infectious and, barrier precautions should be used routinely to protect the healthcare worker from exposure [37]. The current study result to some extent follow Standard universal precautions of hand washing was represented as higher among studied nurses in in-patent ward “majority than half” of out-patient, immediately before wearing gloves. Whereas, majority of studied nurses in in-patent ward compared to more than half out-patient always wearing gloves during communicating with/ giving care for patients. Whereas regarding to nurses in out-patient department more than half always wearing gloves during patient admission. Regarding the Universal Precautions for Equipments majority of nurses in out-patient department two third Clean and disinfect equipment that used more than once for one patient compared to few of studied nurses in in-patent ward. This result was inline with Hand-washing is the most important measure to reduce the transmission of microorganisms [38], and hand washing reduces infection rates, even in high-risk patient populations [39]. Whereas, the current study revealed that clean infected surface with antiseptic solution correctly by most of total studied nurses. This result was emphasized by [40] who concentrated on daily cleaning and disinfection of hard, nonporous surfaces should be done, before disinfecting a surface, cleaning should be performed. Use a rigid waste receptacle designed to support the bag to help minimize contamination of the bag's exterior. New elements of standard precautions have been added. These elements include safe injection practices and the use of masks and possibly head coverings [41].Regarding nurses knowing about the Ebola hemorrhagic fever, the current study revealed that half of the inpatient studied nurses knew about meaning of Ebola disease compared to one third of the outpatient nurses. Regarding how a person infected with Ebola? it was revealed that slightly less than one third of the inpatient studied nurses compared to less than one fifth of the outpatient studied nurses, knew the source of infection of Ebola viruses with the highly statistical significant difference p=<0.009. The current study result was inline with [42] who wrote about “the disease has gained its momentum in spreading across different nations”. Also [43] conclude that although knowledge and awareness about Ebola is high among the participant, there are still misconceptions about the disease. The current studied nurses had already a training program about Ebola By 80%. But they are in need for strengthening the capacity for all nurses with adequate knowledge of preventing, diagnosing, and managing EVD cases. All health workers need continuous education on EVD. Also, [44; 43] the training should focus on the concept of universal precautions, which must be observed by every nurse while interacting with every patient Active monitoring requires that travelers who are considered High-risk" travelers are quarantined upon arrival in their homes, or other location, and also are observed for daily temperature checks [45]. Regarding Clinical Manifestation, the patients with suspected symptoms, including unexplained hemorrhage and risk factors within the last 3 weeks should be evaluated for Ebola hemorrhagic fever is a fatal disease [36]. Knowing when the Signs and symptoms of Ebola appear? The current study revealed that nearly more than one third of the inpatient studied nurses knew when the disease appears, compared to less than one third of out-patient studied nurses with no statistical significant difference between in-patient and out-patient studied nurses P < 0.057 (Table 2). The current study result was inline with [36] who stated that the incubation period range is 2-21 days (average 5-6). Fortunately, the disease is not transmissible until the patient becomes symptomatic, but it continues to be contagious, even postmortem In relation to the question, "did you report to health units if you suspect an Ebola case?" The current study result, was more than half of studied nurses, say they will report immediately to health units. This result was contradicted with the result of [47]. They studied in Khartoum and White Nile states, Sudan". They reported that 83.5% said they would notify health authorities about cases of suspected EVD. The discrepancy between the two results may be attributed to the current study participants need to be much aware of the problem.Overall, Ebola awareness was on the fair level based on the total score of knowledge, intention to behave and practice about Ebola Virus. Approximately half of studied nurse's working in inpatient had poor knowledge about Ebola compared to less than half of studied nurse's working in out-patient had poor knowledge in the total score of the Knowledge while studied nurse' practice was considered above average whereas the least was considered poor practice among nurses working in outpatient and in-patient ward. The current study was consistent with [48]. They reported that, nearly half of nurses had appropriate knowledge compared to other health workers and this association was statistically significant, over half of the respondents had poor knowledge of EVD. Nearly half had good knowledge of EVD, most knew that EVD is a viral infection. American Nurses Association [49] encourages all nurses to develop a preparedness plan that provides specific information on procedures and protocols to be used in hospital or healthcare setting for identifying and caring for a patient with Ebola Virus Disease (EVD). Early identification of Ebola Virus Disease through effective triage is critical to preventing the spread of infection. Also to use the highest level of PPE recommended by the CDC at all times when in contact with a suspected/confirmed Ebola patient. Preparedness Plan.
6. Conclusions
- The current study revealed several important areas of concern as; A) Preparedness level for the safe and appropriate management of Suspected Ebola VD was on fair level in outpatient and in-patients wards. B) Overall, Ebola awareness was on the fair level based on the total score of knowledge, intention to behave and practice about Ebola Virus. C) The majority of studied nurse's working in inpatient and out-patient had positive intention to behave toward Ebola. D) A Positive Correlation was found between Total Knowledge Score & Total Practice Score. That mean the increase of knowledge will show an increase of practice.
7. Recommendations
- Nurses as well as health care workers are in need for strengthening the capacity with adequate knowledge of prevention, infection control policy about EVD is urgently required, focusing on an the concept of universal precautions that target all health workers. Also, an emergency preparedness towards possible EVD is necessary.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML