Jon Ignatius B. Lacsina, Lawrence C. Caranto, Juan Jose T. David
College of Nursing, Benguet State University, La Trinidad, Benguet, Philippines
Correspondence to: Jon Ignatius B. Lacsina, College of Nursing, Benguet State University, La Trinidad, Benguet, Philippines.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Abstract
“No other disease is as challenging to us as dengue because the symptoms are so unpredictable and constantly changing” – Dr. Suresh Kumar (2009). This study examined the healthcare management rendered to with Dengue/DHF from the phenomenological point of view of three staff nurses at Kalinga Provincial Hospital. Interviews and storytelling were the main methods of data gathering. Employment of Colaizzi's strategy in descriptive phenomenology established the data analysis. With the findings in this study conclusions were drawn as follows: frequent assessment, monitoring and observing dengue patients even in its febrile phase helps prevent the progression of the condition. This study also presents that it is important that we should not rely on the warning signs a client is exhibiting because those signs may be indicative of other disease conditions. Hence, laboratory diagnostic should be done to confirm the condition. Though tourniquet test has relatively little predictive diagnostic value for the diagnosis of dengue infection as stated by Mayxay et al, this test might still be helpful as a diagnostic tool to places with no accessible health centers that has laboratories. Further, in order to provide a good health management to infected individual, we must learn the value of teamwork so for with collaborative healthcare management. In addition, measures in taking care of dengue case patients are simple but requires a complex attitude of being a nurse. In other words, all nurses must be dedicated in their vocation and profession and must possess the values of being a competent nurse such as: patience, honesty, and trust when it comes to collaborative healthcare measures. With the findings, we can also say that because dengue is systemic and dynamic, it has a challenging healthcare management. Thus, it is recommended that there should be clear guidelines or dengue protocol available in their institution to standardize the interventions provided by the HCPs in diagnosing and managing a dengue case patient. Furthermore, a session should also be arranged and scheduled regarding updates and trends about Dengue/Dengue Hemorrhagic fever and more information should be disseminated regarding dengue prevention. Moreover, another study should be conducted to build on the findings of this study. We recommend a research involving dengue case patients as their participants as to their views on how they are managed.
Keywords:
Dengue, Dengue hemorrhagic fever, Confirmatory, Medical management, Nursing management
Cite this paper: Jon Ignatius B. Lacsina, Lawrence C. Caranto, Juan Jose T. David, Plague Ground: Healthcare Management of Dengue/Dengue Hemorrhagic Fever, International Journal of Nursing Science, Vol. 5 No. 3, 2015, pp. 103-109. doi: 10.5923/j.nursing.20150503.03.
1. Introduction
Dr. Suresh Kumar said “No other disease is as challenging to us as dengue because the symptoms are so unpredictable and constantly changing” (Ramsay Sime Darby Health Care, 2009 [1]). Dengue is known worlwidw because of its mass affectation in many countries. In the Philippines, at least 42,207 dengue cases were estimated, 193 of them are fatal. These statistics has been recorded from January to the first week of June 2013 (ELR, 2013 [2]). Pangilinan said that there was a total of 5,781 dengue cases in the Cordillera Administrative Region, evenly distributed in the City of Baguio, and the provinces of Benguet, Abra, Kalinga, Mountain Province, Ifugao and Apayao. In the year 2012, however, cases of the said disease shoot up to 56.57% in the year 2013. Based on the report of the Provincial Epidemics and Surveillance Unit (PESU), dengue suspect cases in Kalinga shot up to 90 in July on the same year. (Galagac, 2014 [3]).“Health is individually defined by each person and is affected by so many factors,” (Taylor, Lillis, LeMone & Lynn, 2005) [4]. Therefore, it is difficult to find or impost a concrete definition of health. “Each person defines health in terms of his or her own values and beliefs. The family, community, and society in which one lives also influence one’s personal perception of health.” However, the most widely accepted definition of health is the definition of the World Health Organization which is “Health is characterized by complete physical, mental, emotional, and social well-being, not just merely the absence of disease or infirmity” (WHO, 1974). On the other hand, “Disease is a medical term that would mean that there is a pathologic change in the structure or function of the mind or body” (Taylor et al, 2005). In line with the WHO’s definition to health, Walker (2007) [5] gave meaning to illness which is, it is not just a physical discomfort, but also an imbalance in spiritual or psychological well-being, which implies a loss of mana as well as physical strength. As Taylor et al (2015) reviewed the different definitions of illnesses, they concluded that illness- “is the response of the person to the disease; where person’s level of functioning is changed compared with a previous level.” At this present time, we can’t get rid of the diseases existing in this world from time to time. As new human generation exist, new diseases also exist. As technologies upgrades, it’s like viruses, bacteria and fungi that causes this diseases also upgrades making it more burdensome to people. To be able to go on with plans in life, one must have to conquer hindrances most especially protecting his/her self against diseases so he/she can function well. Disease comes in a varying degree or severity, an alteration in health condition is a problem faced by an affected individual and health plays a vital role in one’s life affirmed by a quote from James Thomson; “Health is the vital principle of bliss, and exercise, of health”. Moreover, when a case of disease occur in excess of what would normally be expected in defined community, geographical area or season it is now called as an outbreak. It may occur in a restricted geographical area, or may extend over several countries that may last for a few days or weeks, or for several years. Outbreak can also be a single case of a communicable disease long absent from a population, or caused by a microorganism not previously recognized in that community or area, or the emergence of a previously unknown disease. If this arises, it must and should be reported and investigated (WHO, 2015). [6]In our present world, lots of diseases are emerging causing an outbreak in many countries. Some of these are SARS, Meningococcemia, Ebola virus, and Mers-Cov. On the list of the World Health Organization, Dengue/Dengue Hemorrhagic Fever is one of the diseases that caused a global outbreak. Dengue is a viral disease transmitted by one of the four dengue virus serotypes. This viral disease is not transmitted directly from person-to-person. It is a febrile illness that affects all ages with symptoms appearing 3-14 days after the infective bite (WHO, 2015). There is good evidence that sequential infection increases the risk of more serious disease resulting in DHF. Before 1970, only nine countries had experienced severe dengue epidemics. However, this disease is now endemic in more than 100 countries in Africa, the Americas, the Eastern Mediterranean, South-east Asia and the Western Pacific. The American, South-east Asia and the Western Pacific regions are the most seriously affected (American Journal of Tropical Medicine & Hygiene, 2014). [7]According to Kelley (2003) [8], the first epidemics of dengue fever were reported simultaneously in 1779 from Egypt and Indonesia and 1780 from the US. He also stated that the first recognized epidemic of dengue haemorrhagic fever occurred in Manila in the year 1953 and 1954. He also added that dengue fever was not considered a public health problem in the Americas until the latter part of the 20th Century.This disease is the most common mosquito-borne viral disease of humans that in recent years has become a major international public health concern. Globally, 2.5 billion people live in areas where dengue viruses can be transmitted. The geographical spread of both the mosquito vectors and the viruses have led to the global resurgence of epidemic dengue fever and emergence of dengue hemorrhagic fever in the past 25 years with the development of hyperendemicity in many urban centers of the tropics (Sharlach, 2014) [9]. CDC, 2014 [10] estimated that about 2.5 billion people, or 40% of the world’s population, live in areas where there is a risk of dengue transmission. In line with this, WHO (2014) [11] in their Global Alert Response Programme also estimated that up to 50 million infections occur annually with 500 000 cases of dengue hemorrhagic fever and 22,000 deaths mainly among children. With the increasing number of dengue incidence, we cannot deny that this disease is a threat to all humans, as the WHO, 2014 said: “that the presented figures of dengue incidence has grown dramatically around the world in recent decades and is a Global burden.”In agreement with the WHO, Simmons, Farrar, Vinh Chau, & Wills (2012) [12] “global burden of dengue is large and urban crowding (which is conducive to multiple infections from an infected mosquito) contributes to the inefficacy of the vector-control strategies. With the development of our modern world, it is difficult to make everyone do the same task on how to prevent dengue. News comes here and there about this deadly disease but still most people don’t follow ways on how to prevent acquiring the disease.”On the other hand, Gubler (1998), [13] states the difficulty in controlling dengue infection stems from three root causes, and that would be the presence of four different serotypes of virus, each with the independent ability to cause fatal disease, a lack of understanding of pathophysiology, non-availability of specific treatment, non-availability of a vaccine for prevention, and difficulties in controlling the vector population. Not only is the number of cases increasing as the disease spreads to new areas, but explosive outbreaks are occurring. In 2014, trends indicate increases in the number of cases in the Cook Islands, Malaysia, Fiji and Vanuatu, with Dengue Type 3 (DEN 3) affecting the Pacific Island countries after a lapse of over 10 years. An estimated 500 000 people with severe dengue require hospitalization each year, a large proportion of whom are children. About 2.5% of those affected die (Center for Disease Control, 2010) [14].The Department of Health in our country is providing public campaigns on dengue prevention because of the serious increasing cases of dengue. Health authorities advised community action to prevent dengue fever. On August 2, 1996, President Fidel V. Ramos, through an executive order, launched the National Tepok Lamok – Dengue Sapok program and the start of the 4 o’clock habit. The DOH led the whole country in a clean-up operation to eliminate all potential mosquito breeding places every 4:00 pm.The Aedes aegypti mosquito, the cause of dengue, breeds in clear, stagnant water accumulated in cans, old tires, flower vases, pots, pails and other containers. People were advised to eliminate these things in their homes, schools and offices. Only by cleaning up the environment and prompt medical attention can the vicious cycle of transmission be broken. Environmental sanitation is believed to decrease the morbidity rate but season makes it hard for the people (Fernandez, 2014) [15].In advance, health management plays an important role to those who are involved in the metaparadigm of nursing namely: person, environment, health and nursing. Medical Dictionary (2007) [16] defined Health management in general as “a system of preventive medicine that takes into account the whole being including social, psychological, physical, spiritual, and physiological factors that affects the health of individual with respect to relationships to other people as well.”Because Dengue/DHF is one of the global health issues, it is therefore important to provide or at least prove something is “worth it” when it comes to managing the said disease. Kalinga, as one of the provinces in the Cordilleras having a high number of dengue cases is a good place to conduct this study. Kalinga having a high morbidity rate has also low mortality rate and this gave us the interest to conduct this study-interesting to know the answer on “HOW” do they manage such case. And, we are more on community this time, as nurse, we are being taught on how to innovate or generate knowledge not only to ourselves but to the people whom we know we can inspire in our own little ways. Starting to make a difference is the beginning of making a change. Hence, this study was conducted.This study will be of great contribution to health/institutional care on managing dengue which will serve as a basis of courses of action to be done when managing dengue patients. This study will also strengthen the role of nurses as researchers. Furthermore, this will serve as a basis for other research undertakings or upcoming research works.
2. Methods
2.1. Research Design
According to Lambert & Lambert (2012) [17], “Qualitative descriptive approach needs to be the design of choice when a straight forward description of a phenomenon is desired. It is an approach that is very useful when researchers want to know, regarding events, who were involved, what were involved, and where did things take place.” This study utilized the descriptive phenomenological research design and integrating Colaizzi’s Strategy.Three (3) staff nurses were selected as participant of the study based on the following criteria: A) Current staff nurses of the institution where the study is conducted, B) They are willing to participate and share their knowledge and experiences, and C) They were able to take care of a dengue or DHF case patient in the institution of the study was conducted. A written consent was obtained from the participants prior to the actual interview. As written in the consent, the participant will not be identified therefore pseudo names were used instead.The main mode used in collecting the data was a semi-structured guided interview and storytelling. Consent was obtained to the participant prior to the actual interview as an ethical consideration. The first question asked was “What are your initial actions when a patient suspected with dengue is brought here in your ward?” Then it goes on up to the last question which is “What are your observations to your patient when the doctor is about to discharge them?”.Conversations from the recorded interviews and validated accounts were then transcribed to form the individual participant’s transcript. After the narrative transcripts were transcribed and generated, the thought gained in each narrative were then analyzed for thematic interlace. Themes were based on the time patients were admitted until being discharged in the institution and on the answers of the participants which led to the following broad domains: 1) Checking-in, 2) Staying-in, and 3) Checking-out.
3. Results and Discussion
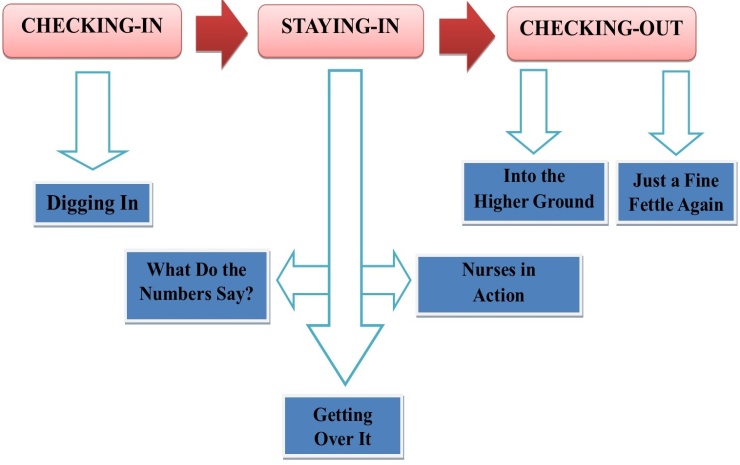
The broad domains and their subthemes are presented on Fig. 1 below. Fig. 1 shows three broad domains and their subthemes: (1) Checking-in with Digging In as a subtheme, (2) Staying-in with the following subthemes: What Do the Numbers Say, Notifying the Disease, Nurses in Action, and Getting Over It, and (3) Checking-out with the following subthemes: Into Higher Ground and Just a Fine Fettle Again.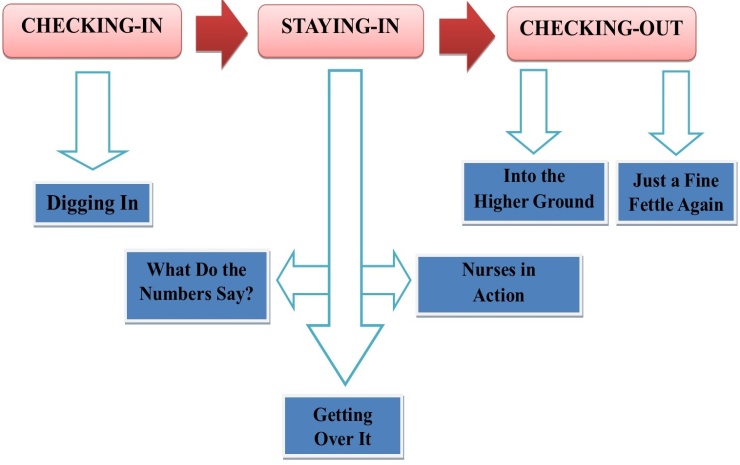 | Figure 1. Conceptual Map |
3.1. CHECKING-IN: This domain includes how the patient is being managed when he/she arrives in the medical ward or in this study is tagged as the “Checking-in’ of the patient in the medical ward.Digging for Evidence. Upon the arrival of the patient in the medical ward, participants (staff nurses) in the institution possessed a similar initial nursing action. Participants in this study stated that when a dengue suspected patient arrives in their ward, their initial action is to re-assess the patient for signs and symptoms of dengue. Nurse Rita said; “Pagdating ng pasyente dito sa ward, nag-aasses kami for progression physically kung meron lalo na sa bleeding.” (When the patient arrives here in the ward, we assess for progression physically especially when bleeding occurs). This is a good nursing action, to compare; dengue is like a nursing career- "it is systemic and dynamic". Let's consider this, according to the WHO (2009) [18], dengue has a wide clinical spectrum that includes both severe and non-severe clinical manifestations. Therefore, even though the patient was already assessed in the emergency department it is still important to re-assess the patient. Just like Nurse Sara said, “Assessment ulit. Importante kasi talaga. Observe for presence of rashes and bleeding.” (Re-assess because it’s really important. Observe for presence of rashes and bleeding.) Assessing, as defined by Taylor et al is "a systematic and continuous collection, validation, and communication of patient data. And these data reflect how health functioning is enhanced by health promotion or compromised by illness or injury." Assessing the patient helps them identify signs and symptoms of dengue that may lead to fatal condition that in the earliest time possible, it can be prevented. As explained by Barbara and Kozier [19], the purpose of the physical assessment includes: “Obtaining baseline data about the client's functional abilities, supplement, confirm, or refute data obtained in the nursing history, obtain data to establish care plans, identify areas for health promotion or disease prevention, and make clinical judgments about health status.” In this therefore, as a basic knowledge in nursing, assessment is very important. Nurse Dara: “Ina-assess ulit yung pasyente. May form lang akong finifil-apan, yung PIDSR. Ako kasi assign sa reports kaya may nagagamit akong form na pagbasehan.” (We assess the patient again, there's a form that I'm filling out the PIDSR form. I'm the one assign with the reports that's why I have a basis.) We should also look into this statement from the WHO (2015), "early clinical diagnosis and careful clinical management by trained physicians and nurses increases survival of patients." (WHO, 2009). Thus, in order to reduce dengue mortality, an organized process that guarantees early recognition of the disease and its management is required.3.2. STAYING-IN: This domain includes the patients’ stay (while being treated in their condition) in the institution-Medical Ward and how they are being managed by the healthcare providers.“For a disease that is complex in its manifestations, management is relatively simple, inexpensive and very effective in saving lives so long as correct and timely interventions are instituted. The key is early recognition and understanding of the clinical problems during the different phases of the disease, leading to a rational approach to case management and a good clinical outcome” (WHO, 2009).What Do the Numbers Say? “Numbers constitute the universal Language”- Nathanael West. In healthcare field, normal ranges are being taught as to fluid and electrolytes, blood components pressures and others. As a competent nurse, knowing that there is an increase or decrease on the numbers within normal limits, you can easily identify the possible problem/s of the patient. This theme includes the confirmatory test for positive dengue.The participants’ answers were similar from each other regarding to when will a patient be classified as having probable/positive dengue. A laboratory positive result of Dengue Dot came out to be the confirmatory of their thought in reference with their assessment. “Maliban sa assessed signs and symptoms for possible dengue, laboratory result pa rin ang hinihintay naming para maconfirm.” (Aside from the assessed signs& symptoms for possible dengue, we still wait for the laboratory result to confirm), said Nurse Sara. Center for Disease Control said that primary dengue infection is characterized by a slow and low titer antibody response. IgM antibody is the first immunoglobulin isotype to appear. As emphasized by the WHO (2009), laboratory diagnosis methods is important in confirming dengue. This coincide the CDC (2012) [20] report that “Dengue can be diagnosed by isolation of the virus, by serological tests, or by molecular methods. Efficient and accurate diagnosis of dengue is of primary importance for clinical care such as early detection of severe cases, and case confirmation.Participants also said that bleeding, abdominal pain or tenderness doesn’t necessarily mean that the patient is a confirmed dengue case because the said symptoms might fall into other health condition such as appendicitis, peptic ulcers and other health conditions that have a comparable signs and symptoms to dengue/DHF. As Nurse Rita stated, “Lab result ang hinihintay namin para maconfirm na dengue. Hindi kasi lahat ng may bleeding o abdominal pain o tenderness eh confirmed dengue case.” (We wait for the lab result to confirm it's a dengue. When there's a bleeding, abdominal pain/tenderness it doesn't mean it's a confirmed dengue case). According to the Medline plus (2013) [21], bleeding is most commonly caused by problems with the joints, or gastrointestinal or urogenital tracts. Therefore it’s challenging to take care of a dengue/DHF case patient with associated conditions that has dengue like signs and symptoms.As Nurse Dara said, “Pag positive ang laboratory result sa dengue dot, confirmed or positive case na. Obsolete na ang tourniquet test.” (If the lab result is positive for dengue dot, then it’s confirmed or it’s a positive case. Tourniquet test is obsolete.) A tourniquet test as defined by Dr. Ayush Goel the co-founder of medico notebook site [22], is also known as a Rumpel-Leede Capillary-Fragility Test or simply a capillary fragility test that determines capillary fragility. It is a clinical diagnostic method to determine a patient's haemorrhagic tendency. This test also assesses fragility of capillary walls and is used to identify thrombocytopenia (reduced platelet count). This test is also defined by the WHO as one of the necessary requisites for diagnosis of Dengue fever. However, a study conducted by Mayxay, Phetsouvanh, Moore, Chansamouth, Vongsouvath, Sisouphone, Vongphachanh, Thaojaikong, Thongpaseuth, Phongmany, Keolouangkhot, Strobel, & Newton [23] revealed that, conventional tourniquet test adds relatively little predictive diagnostic value for the diagnosis of dengue infection, with low sensitivity but good specificity. Because of the availability of more sensitive and specific laboratory tests, Tourniquet test is rarely used by most medical practitioners. However, HCPs must still be knowledgeable on how to perform the test because this can be a very important test to patients in the rural areas who have no access to healthcare centers with laboratories.Nurses in Action. To do what nobody else will do, a way that nobody can do in spite of all we go through; is to be a NURSE-Rawsi Williams. “The most important resource is trained doctors and nurses. (WHO, 2009)”“Monitoring vital signs, pagbibigay ng mga gamot. Pero pag yung time na madaming pasyente, inaadvise din namin mga watcher na i-observe ang mga pasyente for bleeding kasi baka hndi naming mapansin habang nasa ibang pasyente.” (Monitoring vital signs, medication administration. In times when there are many patients, we advise the watcher to observe bleeding. We might not be able to observe that there’s a bleeding while we are with the other patients) said Nurse Rita. Vital signs are indicators on how the circulatory, respiratory, neural, and endocrine body function effectively. Nurse Dara also said that “Mga routine nursing interventions lalo na sa vital signs monitoring. Mostly health teaching lang din at binabantayan din ang hydration.” (Routine nursing interventions especially vital signs monitoring. Mostly, health teachings and we also maintain their hydration.) Monitoring vital signs seems to be the most important thing to do to a dengue case patient based on the participants’ responses. This is supported by the Dengue Virus Net (2015©) [24] wherein it was stated that the mainstay of treatment is timely supportive therapy to tackle shock due to hemoconcentration and bleeding. Close monitoring of vital signs in critical period of the degue (between days 2 to day 7 of fever) is critical. As nurse Sara said, “Collaborative nursing interventions. Maliban sa vital signs taking, TSB and health teaching din lalo na sa diet. Minsan napagsasabihan pa kami ng mga doctors pag report kami ng report sasabihin nila na “basta kumakain at umiinom ng marami ang pasyente walang problema.” (Collaborative nursing interventions. Aside from vital signs taking and TSB, health teachings particularly on diet are also provided. The doctors also advise us to calm down when we frequently report the condition of our patient. They would say “As long as the patient is eating and drinks plenty of fluids, there’s no problem.). As part of the healthcare team, it is important that we work with each member of the team to provide the possible and appropriate nursing intervention. This coincides with the discussion paper of Mitchell, Wynia, Golden, McNellis, Okun, Webb, Rohrbach, & Kohorn, (2012) [25] which states that “high-performing team is now widely recognized as an essential tool for constructing a more patient-centered, coordinated, and effective health care delivery system.” Every discipline is integral. In the healthcare field, the relationship between the nurse and the physician is paramount. The physician orders necessary interventions, and the nurse is responsible for carrying it out. Further, Nurse Rita stated that “Pag severe case, kailangan ang close monitoring, pero pag hindi naman, monitor pa din for signs that may lead to severe condition” (If it’s a severe case, patients are closely monitored, but if not, we still monitor for signs that may possibly lead to severe condition). And Nurse Sara related with her statement that “Wala naman dapat pagkakaiba kasi ipreprevent nga na hindi maging severe condition kaya monitor, monitor, monitor as possible.” (There is no difference because we are preventing that it may lead to severe condition that’s why we keep on monitoring as possible.) However, Nurse Dara averred that “Sa severe cases mas minomonitor kasi posibleng maglead sa shock and altered sensorium.” (In severe cases, it is monitored more because of the possibility that it may lead to shock and altered sensorium.) This sustains this statement by the WHO (2009) that, in total population of dengue infected patients, 75% are asymptomatic. Symptomatic infection most commonly presents as mild to moderate, nonspecific, acute febrile illness. However, 5% develop to severe which is a fatal condition. Getting Over It. These are the medical management given to Dengue/DHF positive patients who are admitted in the institution. These include the medications, IV fluids and tests.In dengue/DHF, IV fluids are necessary due to the fever, the loss of appetite, bleeding and possible diarrhea that lead to increase fluid loss. The goal of IV fluid administration is to correct or prevent fluid and electrolyte disturbances. “IV Fluids, LRS ang binibigay. Paracetamol at ang walang kamatayang ascorbic acid.” (IV Fluids, LRS is the usual fluid given. Paracetamol and of course ascorbic acid) said Nurse Rita. Intravascular volume deficits should be corrected with isotonic fluids such as Ringer lactate solution (Medscape, 2015). Nurse Dara related, “Ang kailangan naman kasi dapat hydrated yung pasyente. Ang IVF nila PNSS o PLRS tapos nagrereseta din sila ng analgesic” (The patient must be hydrated. Their IVF is PNSS or PLRS and they also prescribe analgesic.) Fluids and electrolytes may be replaced through infusion directly into the blood rather than via the digestive system (Taylor et al, 2009). Aspirin which is an analgesic should not be given to dengue case patient because of its anti-platelet effect (Nursing Drug Handbook, 2012). So preferably, acetaminophen or paracetamol is given to reduce fever. As stated by Nurse Sara “Ang pain reliever nila is paracetamol. Yun ang prineprescribe ng mga doctors.” (Paracetamol is the prescribed pain reliever by doctors.)A routine laboratory is also ordered by doctors for them to observe the progression of the patient’s condition of the patient. “Routine laboratory ang isang pinaka importante sa mga inoorder ng mga doctor.” (Routine laboratory is one of the most important orders of the doctors.), as stated by Nurse Sara. Nurse Rita also said that “A routine laboratory is being ordered by doctors. It is either every 4°, 6° or 8°.” Nurse Dara affirmed, “Discretion ng doctor kung ano ang frequency ng Routine Labs.” (The frequency of the routine labs depends on the doctor’s discretion.) As the Tropical Medicine & International Health said, without serological tests as confirmatory diagnostic, patients whose true diagnoses are non-dengue infections, they can be misdiagnosed as dengue and thus will miss the chance of specific treatment or the other way around. Routine Laboratory works will allow the HCPs to provide appropriate interventions the patient needs.3.3. CHECKING-OUT. This domain includes the observation of the participants on the patient when he/she leaves the institution or in this study is tagged as the “Checking-out’ of the patient in the medical ward.Into Higher Grounds. This theme includes the responses of the participants as to when the patients are referred to other institution for further care and management.Nurse Dara stated, “Pag hindi na macontrol ang pagbaba ng platelet count, mag-oorder na ang doctor ng referral to CVMC (Cagayan Valley Medical Center).” (If the platelet count persists to decrease, the doctor will order a referral to CVMC.) Referral is the process of sending or guiding the patient to another institution. Participants said that the blood bank in the area doesn’t have platelet concentrate which makes the doctors refer the patients to other institutions especially when a patient is in shock or/and needs immediate platelet transfusion. “Wala kasing platelet concentrate dito kaya nagrerefer ang mga doctor sa CVMC para maagapan.” (There’s no platelet concentrate here that’s why patients are being referred by doctors to CVMC to prevent further impairment.), said Nurse Rita. When HCPs in an institution detect problems they cannot resolve because of lack of resources, to be able to render what’s best for the patient to achieve their optimum level of functioning, they make referrals to other institution that can provide such or that can better manage the underlying condition of the patient. Nonetheless, Nurse Sara said, “Depende sa doctor kung magrerefer siya. Kung hindi ma maintain ng interventions namin ang pasyente, o pag may signs of shock, magrerefer na ang doctor.” (Referral depends on the doctor’s discretion. If our interventions can’t maintain our patients’ condition, or when there are signs of shock, doctors might as well refer them.)Just a Fine Fettle Again. This theme looks into the ‘Fettle’ (-also known ‘condition’) of the patient before being discharged by the doctors.Wellness is a more active state, oriented toward maximizing the potential of the individual, regardless of his or her state of health. When clients are admitted, it simply means they have health problems. For sure all they want is to get well and be in good condition for them to be able to do their desired activities in life. “Pag wala nang fever ng mga 48 hours tapos stable na ang vital signs pwede ng i-discharge ng doctor” (If the patient has no fever for around 48 hours and has normal vital signs, the doctor can discharge the patient.) said Nurse Dara. According also to Nurse Rita and Nurse Sara “Depende sa doctor. Pero usually pag ok na yung pasente, na walang fever ng ilang araw tapos within normal levels na rin ang platelet count ididischarge na ng doctor yung pasyente.” (It depends on the doctor. But usually, when the patient is okay, no fever for how many days and platelet count is within normal level, the doctor will discharge the patient.)Surviving Dengue which is one of the challenging disease conditions on both HCPs and the patient can be considered a miracle in one’s life.
4. Conclusions
This study presented the healthcare management of dengue/DHF in Kalinga Provincial Hospital as to how patients with such case are managed in the whole course of the disease. On the insights gathered from the participants’ transcripts, conclusions were drawn as follows: frequent assessment, monitoring and observing dengue case patients even in its febrile phase help prevent the progression of the condition. This study also presents that it is important that we should not rely on the warning signs a client is exhibiting because those signs may be indicative of other disease conditions. Hence, laboratory diagnostic should be done to confirm the condition. Though tourniquet test has relatively little predictive diagnostic value for the diagnosis of dengue infection as stated by Mayxay et al, this test might still be helpful as a diagnostic tool to places with no accessible health centers that has laboratories. Further, in order to provide a good health management to infected individual, we must learn the value of teamwork so for with collaborative healthcare management. In addition, measures in taking care of dengue case patients are simple but require a complex attitude of being a nurse. In this case, all nurses must be dedicated in their vocation and profession and must possess the values of being a competent nurse such as: having patience, honesty, and trust when it comes to collaborative healthcare measures. With the findings, we can also say that because dengue is systemic and dynamic, it has a challenging healthcare management.With these, it is recommended that there should be a certain guideline or dengue protocol available in their institution to standardize the interventions provided by the HCPs in diagnosing and managing a dengue case patient. Furthermore, a session should also be arranged and scheduled regarding updates and trends about Dengue/ Dengue Hemorrhagic fever and more information should be disseminated regarding dengue prevention. Moreover, another study should be conducted to build on the findings of this study. We recommend a research involving dengue case patients as their participants as to their views on how they are managed.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the Kalinga Provincial Hospital’s Chief Nurse for allowing this study to take place in their institution, and the participants for their valuable contributions in making this study possible. And also to the following people for making the publication of this paper possible: Mr & Mrs Manuel S. Agyao, and Mr & Mrs Jun Sto. Domingo.
References
| [1] | Ramsay Sime Darby Healthcare, 2009 [Online]. Available: http://www.ramsaysimedarby.asia/eng/company-info/media/news-articles/spot-vital-dengue-signs-early-doctors-are-told-news-straits-times. |
| [2] | GMA News, 2013. |
| [3] | Sunstar Newspaper: DOH: More effort vs dengue in 2014, Aure Galacgac, January 2014. |
| [4] | Fundamentals of Nursing: the Art and Science of Nursing Care, Sixth Ed, Carol Taylor., Carol Lilis., Priscilla LeMone., Pamela Lynn, Walnut St. Philadelphia, PA 19106, 2008, Health & Illness (4) p. 65-77. |
| [5] | American Journal of Nursing, Duane D. Walker, Lippincott Wolkers & Wilkins, 2009. |
| [6] | WHO| Disease Outbreak, 2015© [Online]. Available: http://www.who.int/topics/disease_outbreaks/en. |
| [7] | NCBI| The American Journal of Tropical Medicine “Economic Impact of Dengue”, 2015©. [Online]. Available: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3029168/. |
| [8] | Textbooks of Military Medicine: Military Preventive Medcine, Mobilization. Vol.1. Patrick W. Kelley. USA.2003. (21) p.479-480. |
| [9] | The Scientist: New Dengue-Detecting Antibodies, Molly Sharlach, December 2014. [Online] Available: http://www.the-scientist.com/?articles.view/articleNo/41666/title/New-Dengue-Detecting-Antibodies/. |
| [10] | Center for Disease Control and Prevention| Dengue Epidemiology, June 2014. [Online] Available: http://www.cdc.gov/dengue/epidemiology/. |
| [11] | WHO| Dengue, 2014© [Online]. Available: http://www.who.int/mediacentre/factsheets/fs117/en/. |
| [12] | The New England Journal of Medicine, 2012 Massachusetts Medical Society. |
| [13] | PubMed.gov, Gubler DJ, 1998 [Online]. Available: http://www.ncbi.nlm.nih.gov/pubmed/9665979. |
| [14] | Center for Disease Control and Prevention | Epidemiology, 2012 [Online]. Available: http://www.cdc.gov/dengue/epidemiology/. |
| [15] | UNILAB | How to Prevent Dengue, Rhoel Fernandez, 2014 [Online]. Available: http://www.unilab.com.ph/consumers/articles-and-advisories/physical/how-to-prevent-dengue/. |
| [16] | The Free Medical Dictionary, Farlex, 2012 [Online]. Available: http://medical-dictionary.thefreedictionary.com/health+management. |
| [17] | Streubert, H. J., & Carpenter, D. R. 2002. Qualitative Research in Nursing: Advancing the Humanistic Imperative, 3rd Ed., Philadelphia: Lippincott Williams & Wilkins, (10)p. 171-181. |
| [18] | Dengue Guidelines for Diagnosis, Treatment, Prevetion & Control, 2009 Edition, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland. |
| [19] | Fundamentals of Nursing: Australian Edition, 7th ed, Barbara & Kozier, Pearson Australia, 2014. |
| [20] | Center for Disease Control and Prevention | Laboratory Guidance and Diagnostic Testing, 2012 [Online] Available: http://www.cdc.gov/dengue/clinicalLab/laboratory.html. |
| [21] | Medline Plus | ADAM | Jacob L. Heller, 2013 [Online]. Available: http://www.nlm.nih.gov/medlineplus/ency/article/000045.htm. |
| [22] | Medico Notebook. [Online]. Available: http://www.mediconotebook.com/2011/08/rumpel-leede-test.html. |
| [23] | NCBI | Tropical Medicine & International Health, Predictive diagnostic value of the tourniquet test for the diagnosis of dengue infection in adults; Mayfong Mayxay, Rattanaphone Phetsouvanh, Catrin E Moore, Vilada Chansamouth, Manivanh Vongsouvath, Syho Sisouphone, Pankham Vongphachanh,1 Thaksinaporn Thaojaikong, Soulignasack Thongpaseuth, Simmaly Phongmany, Valy Keolouangkhot, Michel Strobel, &Paul N Newton, 2011 [Online]. Available: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3073123/. |
| [24] | Dengue. Dengue Virus Net. 2014. [Online]. Available: http://www.denguevirusnet.com/diagnosis.html. |
| [25] | Core Principles & Values of Effective Team-Based Health Care: Discussion Paper, Pamela Mitchell, Matthew Wynia, Robyn Golden, Bob McNellis, Sally Okun, C. Edwin Webb, Valerie Rohrbach, and Isabelle Von Kohorn, Institute of Medicine, Washington, D.C., p. 2-6, October 2012. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML