-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2015; 5(2): 41-46
doi:10.5923/j.nursing.20150502.01

Patient Perceptions and Experience of Pain, Anxiety and Comfort during Peripheral Intravenous Cannulation in Medical Wards: Topical Anaesthesia, Effective Communication, and Empowerment
Fwo Yi Tee , Christine Siew Lan Low , Patricia Matizha
Nursing Division, International Medical University (IMU), Kuala Lumpur, Malaysia
Correspondence to: Fwo Yi Tee , Nursing Division, International Medical University (IMU), Kuala Lumpur, Malaysia.
| Email: |  |
Copyright © 2015 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Peripheral intravenous cannulation (PIVC) is one of the most common invasive procedures that healthcare personnel perform daily, often a source of patients’pain, anxiety, dissatisfaction and discomfort. Despite the importance of increasing patient’s comfort in medical care, this need has being increasingly overlooked during PIVC, especially in the current busy clinical settings. Doctors and nurses play a significant role in providing effective, easy-to-implement pharmacological and non-pharmacological management to help patients cope with pain, distress, and anxiety in the frequently performed cannulation. Objective: To assess adult patient perceptions and experience of comfort, pain and anxiety during PIVC in medical wards. Design and Setting: A cross-sectional descriptive study was carried out on 120 adult patients admitted to medical wards. Methods: Patients aged 18 to 65 who had undergone PIVC for 24 to 48 hours, with an 18 gauge Vasofix cannula and were alert and conscious during cannulation were included in the study. The study was guided by Kolcaba’s Theory of Comfort. A structured face-to-face survey was used to collect data. Descriptive statistics were used to analyse the data. Results: One hundred and fourteen patients (95%) experienced pain and 88 patients (73.3%) reported anxiety during PIVC. Forty-seven patients (53.2%) stated that they were afraid of needle pain, 26 patients (30.2%) were afraid of staffs’ability during PIVC, and 12 (13.5%) were afraid of blood or bleeding. Ninety-two patients (76.6%) indicated that their healthcare professional only pricked them once during cannulation. Only a small number of patients (11.7%) were offered topical anaesthesia and very few patients (15.8%) were given the option to choose their preferred site for cannulation. The majority of patients, 110 (91.7%), expressed the need for topical anaesthesia and 116 patients (96.7%) reported effective communication for pain relief. One hundred and eighteen patients (98.3%) said they thought they would have been more comfortable if they had been able to choose the site for cannulation. Conclusions: The results may raise awareness of the need to reduce patients’pain and anxiety during PIVC. Using both pharmacological and non-pharmacological approaches, including topical anaesthesia, effective communication (friendly and informative staff) and empowerment to choose the site for cannulation; patients will be more relieved and subsequently reduce negative experiences that aids recovery.
Keywords: Anxiety, Cannulation, Comfort, Communication, Experience, Perception, Pain, Topical anaesthesia
Cite this paper: Fwo Yi Tee , Christine Siew Lan Low , Patricia Matizha , Patient Perceptions and Experience of Pain, Anxiety and Comfort during Peripheral Intravenous Cannulation in Medical Wards: Topical Anaesthesia, Effective Communication, and Empowerment, International Journal of Nursing Science, Vol. 5 No. 2, 2015, pp. 41-46. doi: 10.5923/j.nursing.20150502.01.
Article Outline
1. Introduction
- Peripheral intravenous cannulation (PIVC) is a common procedure performed on patients. Up to 80% of patients have a peripheral intravenous cannula inserted while in hospital [1]. Regarded as a minor surgical procedure, it is also one of the most common invasive procedures that healthcare personnel perform [2]. Peripheral intravenous cannulae are an inexpensive method of delivering medications, blood products, and diagnostic reagents to assist with diagnosis, parenteral intravenous nutrition or infusion over periods of days to months [3].However, placing a cannula brings pain and anxiety, and interferes with activities of living (ALs), which negatively affects patient comfort [4, 5]. Distress was more likely to be reported if there was no understanding of why the intravenous cannula was placed, as PIVC is a source of pain and anxiety [4, 6]. It was previously reported that the practitioner’s manner and approach will have a direct bearing on the patient’s experience [7]. Most research literature on intravenous cannulation focuses on technical practice and mechanistic care of PIVC [1, 6]. However, only few studies had highlighted concerns on patient’s discomfort [4]. In the usual practice, patients are usually not well informed prior to a PIVC procedure, seldom offered with topical anaesthesia before cannulation, and the patient is not allowed to choose the insertion point [3, 4, 8]. In fact, patient’s perceptions, experiences of comfort and emotional involvements should be acknowledged as well [9, 10].The experience of having PIVC during hospitalisation can be distressing and traumatising for most patients and may result in dissatisfaction with treatment [11]. Therefore, the objective of the study is to determine patient perceptions and experience of comfort, pain and anxiety during PIVC in medical wards. The study was guided by Kolcaba’s Theory of Comfort, which emphasises the understanding of comfort as having one’s comfort need met in four contexts –physical, psychospiritual, sociocultural and environment [12, 13]. We found that by using appropriate measures to raise awareness on PIVC among healthcare personnel, patient’s perceptions and experience of pain, anxiety and comfortcan be minimise to aid in recovery.
2. Methods
- PubMed, Google Scholar and Web of Science databases were searched for publications of relevant studies between 1990 and 2013, using the following search terms: peripheral intravenous cannulation, comfort, pain, anxiety, perception and experience.
2.1. Sample and Setting
- A cross-sectional descriptive design was carried out on a sample of 120 patients with PIVC in the adult medical wards of a district hospital in Malaysia. Inclusion criteria were: (i) aged 18 to 65 years old, (ii) admitted in medical wards, (iii) alert and conscious during the peripheral intravenous cannulation procedure, and (iv) had PIVC for 24 to 48 hours, with an 18 gauge Vasofix cannula. Patients were excluded if they had altered cognitive function and mental status, were unable to communicate or understand and converse in English or Malay, if they had a central venous cannula or were receiving chemotherapy. The sample size was calculated based on power at 0.80 with an alpha of 0.05, confidence level of 95%, and response distribution of 63%. The required sample size for the study was 108. Twelve subjects were added in this sample size to cater for 10% of attrition and the total sample size for this study was 120.
2.2. Instrument
- The Peripheral Intravenous Cannulation Instrument (PICI) was a structured, self-designed questionnaire based on Theory of Comfort and previously relevant published articles [4, 8]. The content was based on physical and psychological comfort. A panel of academic professionals, researchers and healthcare personnel discussed and analysed the validity and feasibility of the instrument. A pilot study with six patients in another hospital who met the inclusion criteria was used to test reliability, face validity and feasibility. The panel of experts reached consensus on the format and contents of the amended items after two formal meetings. An alpha coefficient of Cronbach was included in the interval [0.70, 0.72] corresponded with satisfactory internal consistency after two items were identified and removed (using the Omitted Item Statistics Sections of the output) to improve reliability.
2.3. Data Collection
- Patients consented to the study purpose, its duration, potential benefits and potential risks. Written patient consents were obtained. The survey was done after PIVC was placed and generally took 20 to 25 minutes to complete. It was administered through face-to-face interviews, either in English or Malay, depending on the patient’s language preference. All identifiable information and research data was coded.
2.4. Statistical Analysis
- All analyses were performed using SPSS, version 18.0 and statistical significance was set at P<0.05. The internal consistency of the self-designed instrument items was determined by Cronbach’s alpha. Descriptive statistics: mean, standard deviation, percentages and frequencies were used to illustrate the data.
2.5. Ethics Approval
- The study was approved by research ethics review boards at both the International Medical University Joint-Committee of the Research and Ethnics Committee [Ref: BN101/2010(07) 2013] and the Medical Research and Ethics Committee [Ref: KKM/NIHSEC/800-2/2/2/P13-239). The Director of the hospital granted permission to conduct the study. The study was registered with the National Medical Research Register [Ref: NMRR-12-1276-14450].
3. Results
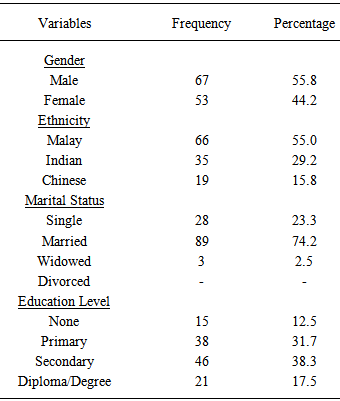
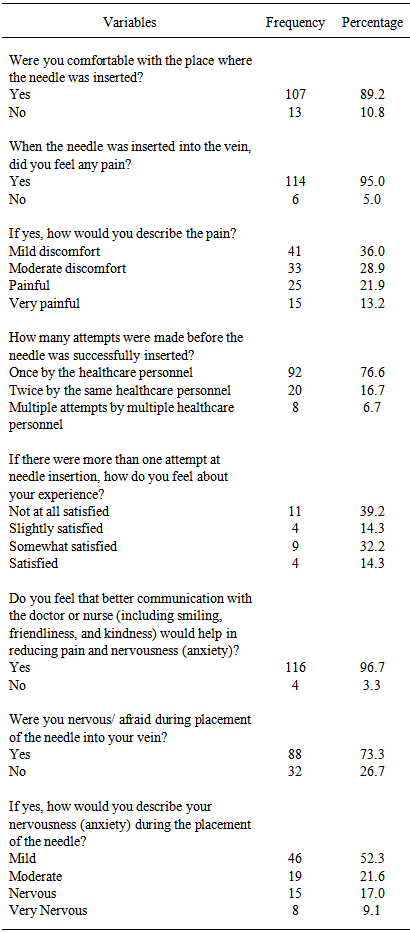
- A total of 132 patients were approached in the medical wards; 120 (91%) responded. Of these, two declined to participate due to the lack of time and 10 did not meet eligibility criteria. Patient demographics are listed in Table 1. The patients comprised of 67 males (55.8%) and 53 females (44.2%). The mean age was 44.2 (SD 14.3) years (range 18 – 65). On ethnicity, 66 (55%) were Malay, 35 (29.2%) were Indian, and 19 (15.8%) were Chinese. Average hospitalisation lasted 36.2 (SD 7.3) hours (range 24 – 48). There were 101 patients (84.2%) who stated that they had been admitted to the hospital before, while 19 patients (15.8%) stated that they had never been admitted to the hospital. In accordance, 42 patients (35%) were admitted for uncontrolled diabetes mellitus, 41 patients (34.2%) had hypertension, 14 patients (11.7%) were admitted for asthma, 12 patients (10%) were admitted for gastrointestinal tract problems, 6 patients (5.3%) were admitted for unknown origin fever, 3 patients (2.4%) were admitted for burn injuries, and 2 patients (1.4%) were admitted for urinary tract infection and food poisoning. Of their experience with cannulation, 94 patients (78.3%) stated that this was not their first time. Patients stated the reason(s) for PIVC as follows: administration of medications, 98 patients (81.7%); administration of fluids, 88 patients (73.3%); blood test, 27 patients (22.5%); blood transfusion, 9 patients (7.5%); and one (0.8%) for unknown reason.
|
|
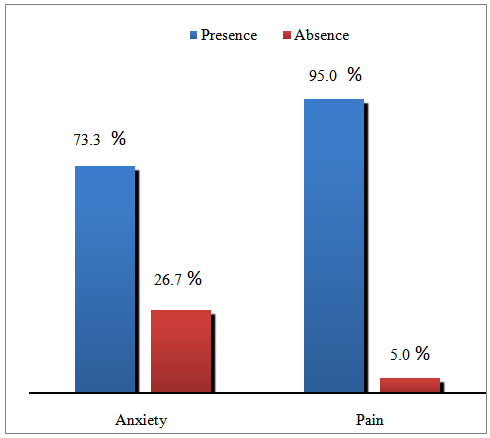 | Figure 1. Patients’ experiences of pain and anxiety during PIVC (n=120) |
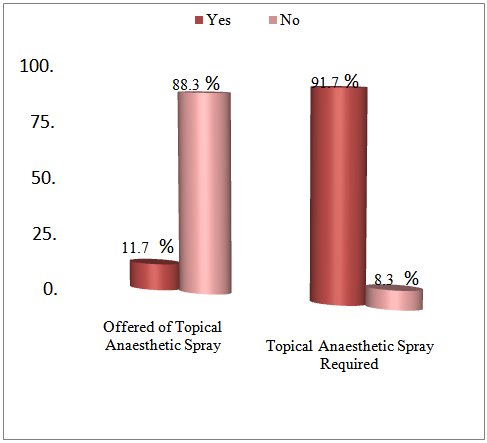 | Figure 2. Offered of topical anaesthetic spray by the healthcare personnel; patients who required topical anaesthetic spray during PIVC (n=120) |
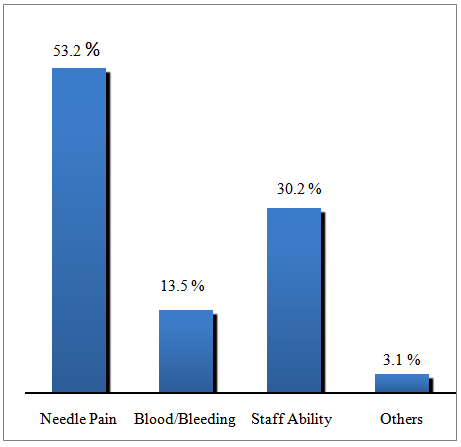 | Figure 3. Causes of patients’anxiety during PIVC (n=120) |
4. Discussion
- The mean age of respondents was 44.2 (SD 14.3) years (range 18 – 65), which indicated that the majority of the patients were in the middle age developmental group. Most of the patients (55%) in this study were Malay (n=66). Pain was experienced by 95% of the patients during PIVC. This finding is similar to a study conducted by Halter and colleagues, which reported that 75% of patients experienced pain when the intravenous cannula was placed [4]. Intravenous cannulation is a very painful and distressing procedure, which may even stop patients from seeking healthcare and refusing to undergo cannulation [14]. This implies that patients may benefit from pharmacological and non-pharmacological pain management to reduce pain during PIVC. Positive and effective communication with patients to address their concerns may help in alleviating pain. The findings was supported by a previous study, 70% of patients indicated that they would request topical anaesthesia for cannulation [5]. Puntillo and colleagues [15] reported that patients who were experiencing pain before a procedure were more likely to receive analgesia during the procedure. It may indicates that healthcare personnel might not be sensitive to the patients’ comfort needs in regards to pain. Fourteen patients (11.7%) patients who had topical anaesthesia prior to cannulation experienced mild to moderate pain. This also suggests that the use of topical anaesthesia prior to PIVC is an efficacious comfort measure that can significantly improve the quality of care and comfort of patients. Anxiety was experienced by most of the patients, 73.3%, during PIVC. This is supported by Burke and colleagues, [16] who reported that discomfort associated with intravenous cannulation can cause patient anxiety and dissatisfaction. Healthcare personnel should acknowledge anxiety during PIVC, and they should design comfort measures to reduce anxiety and make patients more comfortable.The results show that only 19 patients (15.8%) were offered the option to choose a preferred site for needle insertion. A total of 118 patients (98.3%) felt their comfort level would increase if they were given the option to choose a preferred site. The majority of patients wanted to be allowed to choose the preferred site for cannula insertion. This finding implies that healthcare personnel should involve patients in deciding the site for intravenous cannulation if there are no medical contraindications as it directly affects the movement and function of the limb. These findings are further supported by Polak and colleagues, [3] who found that patient willingness to undergo future cannulation was strongly related to cannula location and interference with activities of living. Cannulating over joints should be avoided as it causes discomfort, reduces patient mobility and interferes with activities of living. The effectiveness of communication by healthcare personnel in relieving pain and anxiety was evidenced by 116 patients (96.7%), who reported effectiveness of communication in relieving pain and anxiety. This finding is supported by Simonsen-Rehn and colleagues, [17] who found that participants emphasised the importance of communication and kindness in addition to a proactive approach in patient care. This implies that the majority of patients are more comfortable with their care if they feel that they are actively involved by being told about the procedure being performed. The importance of providing adequate information relating to the procedure was supported by 74 patients (88.1%) in this study, who stated that the information given to them has helped to reduce their anxiety. Lücker and Stahlheber-Dilg [18] stated that the provision of clear and comprehensive information relating to the procedure should reduce patient anxiety. Healthcare personnel should provide adequate explanations to alleviate fear and anxiety.There were 110 patients (91.7%) who preferred topical anaesthesia before cannulation. However, only 14 (11.7%) were offered topical anaesthesia prior to PIVC. This implies that topical anaesthesia may act as optimistic pain management in order to increase patient comfort and reduce the fear of cannulation. Experience of anxiety during intravenous cannulation may result in vasoconstriction, it then cause the procedure more difficult for patient and healthcare personnel and more painful for the patient [19]. Hence, in settings where topical anaesthesia is not accessible, it is important to reassure the patient with effective communication (including smiling, friendliness and kindness) to ease pain and anxiety. Patient care should continue to be holistic – effective communication with patient during PIVC must be established in order to ensure continuous rapport between healthcare personnel and patients. One limitation of the study is that it may not be possible to generalise the findings for other demographic areas in view of the use of the convenience sampling method. Future study on culture and ethnicity in pain perception could be considered. Perceptions and experiences of pain and anxiety might vary between those first experiencing PIVC and those who have had the procedure before. The research was specific to adults and cannot be generalised for children. Future studies in a larger population and different settings would be required to refine the questionnaire and test-retest correlations.
5. Conclusions
- Patients who undergo PIVC may experience pain, anxiety and discomfort throughout the procedure. The importance of meeting the need for comfort, relieving pain and anxiety during cannulation, should be emphasised as it may contribute to a more efficient treatment process. Since there was a positive response on the need for topical anaesthesia prior to PIVC, pre-treatment with topical anaesthesia should be suggested as an option for pain relief for adult patients. The study could provide information that facilitates the improvement in quality of care during the procedure, as it shows that the majority of patients’ comfort levels are affected during PIVC. The use of topical anaesthesia, effective communication and patient empowerment should be acknowledged to produce better care outcomes.
ACKNOWLEDGEMENTS
- The authors would like to thank the Director of Health Malaysia for his permission to publish this paper. This study was supported by a grant from the International Medical University, Malaysia.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML