-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Nursing Science
p-ISSN: 2167-7441 e-ISSN: 2167-745X
2015; 5(1): 35-40
doi:10.5923/j.nursing.20150501.05
Postnatal Care by Student Nurses
Jezreen C. Ambales, Lawrence C. Caranto, Juan Jose T. David
College of Nursing, Benguet State University, La Trinidad, Benguet, Philippines
Correspondence to: Jezreen C. Ambales, College of Nursing, Benguet State University, La Trinidad, Benguet, Philippines.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
This article is a report of a study conducted to explore the postnatal care by student nurses. A woman has come through a tremendous psychological experience during pregnancy and birth of child. In this light, the study primarily aimed to determine the clinical practice protocol for postnatal care rendered by student nurses. Specifically, it sought to determine the nursing practices that are frequently utilized when the following clinical practice protocols are considered: assessment, plan, implementation and evaluation. Furthermore, it sought to determine if there is a difference of postnatal care rendered by student nurses when grouped according to sex. Questionnaires were administered to sixty-seven (67) third year student nurses. Results revealed that student nurses gave the most emphasis on breastfeeding practices specifically highlighting the following: assessment- ‘I monitored vital signs hourly for the next 3 hour’; plan-‘I planned that the patient will be able to verbalize understanding regarding breastfeeding’; implementation- ‘I emphasized to breastfeed per demand’; and evaluation- ‘verbalized understanding on the health teachings about breastfeeding’. Moreover, the results showed that student nurses always render postnatal care following the clinical practice protocol as to assessment, plan, implementation and evaluation. The study yielded two different results when grouped according to sex; that of having significant effect in the areas of implementation and evaluation, and no significance when dealing with assessment and planning.
Keywords: Assessment, Clinical practice protocols, Evaluation, Implementation, Plan, Postnatal care
Cite this paper: Jezreen C. Ambales, Lawrence C. Caranto, Juan Jose T. David, Postnatal Care by Student Nurses, International Journal of Nursing Science, Vol. 5 No. 1, 2015, pp. 35-40. doi: 10.5923/j.nursing.20150501.05.
Article Outline
1. Introduction
- Health is defined as “an experience that is often expressed in terms of wellness and illness, and may occur in the presence or absence of injury” (ANA, 2010) [1]. Maternal health refers to the health of women during pregnancy, childbirth and the postpartum period. Although the number of maternal deaths has been declining, they are still far from the targets set by the Millenium Development Goals in most countries (WHO, 2010) [2].Every year, four million infants die within their first month of life, representing nearly 40 percent of all deaths of children under age 5 (WHO, 2010) [2]. Given the exceptional extent to which the deaths of mothers and babies occur in the first days after birth, the early postnatal period is the ideal time to deliver interventions to improve the health and survival of both the newborn and the mother (WHO, 2010) [2]. Hence, appropriate care in the period following birth is critical not only for survival but also for the future of mothers and newborn babies.Yelland et al. [3] (1998), states that postpartum period is an opportunity for women to rest and recuperate following delivery, to receive guidance, support, and information on baby care. It is a time of reflection, of relieving the birth experiences and a time of adjustment to the new roles. The basic knowledge that nurses use to make decisions and solve problems provides the foundation for developing and improving skills (Given, et al. 2009) [4]. As stated in Butcher [5] (2006), “A unique body of knowledge is a foundation for attaining the respect, recognition, and power granted by society to a fully developed profession and scientific discipline”.The study primarily aimed to determine the clinical practice protocol on postnatal care rendered by student nurses. Specifically, it sought to determine the nursing practices that are frequently utilized when the following clinical practice protocols are considered: assessment, plan, implementation and evaluation. Furthermore, it sought to determine if there is a significant difference of postnatal care rendered by student nurses when grouped according to sex. Nurses will never know the quality of care they offer until it is being assessed with the fact that they will be dealing with various patients (Given, et al. 2009) [4]. This study measured the quality of care provided by student nurses.The study is designed to gather and provide relevant information concerning the postnatal care. This is an exercise to other student nurses in the practice of their roles in finding problems and developing solutions to better improve the practice of the nursing profession. The study will add up to their current knowledge on postnatal care. Moreover, they will be equipped with the necessary skills for a more effective, reliable and comforting assessment for postpartum patients.To the clinical instructors, they will be able to see the area wherein student nurses need more skills, support and encouragement in rendering postnatal care. They can be given idea thoughts on what to discuss with them in relation to postnatal patients and postnatal care.The study will help the researcher not only to gain knowledge on the postnatal care rendered by student nurses but also to enhance and improve the care and health promotion teachings rendered in the community and clinical visits. Moreover, they will be able to differentiate the care rendered to mothers if sex is involved. Finally, this study serves as a reference for future studies in dealing with postnatal patients.
2. Background
- The immediate response most nurses give centers on the activities they carry out to ensure a safe outcome for both the mother and baby. They know that life and death may hang in the balance if accurate and thorough judgment in observing the client is not properly executed. Nurses use critical thinking as they apply knowledge, evidence, and caring to the nursing process. The challenge is now therefore to define interventions that might improve nurses’ knowledge and practice to improve their performance (Mike, et al. 2009) [6].In Kenya, correct care during the postnatal period for mother and baby is outlined in the National Guidelines for Quality Obstetrics and Perinatal Care (2004). However, these guidelines lack specific recommendations on postnatal care for both mother and infant from the first six hours postpartum to six weeks after delivery A study conducted highlight the low priority of nursing interventions accorded to postnatal clients thus, collaborative approaches and continuum of care were suggested (Yelland et al., 1998) [3]. Another observational study done by Department of Health (DOH) with WHO in 2009 stated that clinical practice in 51 hospitals that represent approximately 10% of deliveries nationwide lack appropriate attention focusing on postnatal care (Sobel et al., 2012) [7].Clients are not all the same. Caring is a universal phenomenon that influences the ways in which people think, feel and behave in relation to one another. It is always specific for each nurse-client encounter. This facilitates a nurse’s ability to know a client, allowing the nurse to recognize a client’s problem and to find and implement individualized solutions (Potter and Perry, 2008) [8]. In nursing, this goal is to facilitate and enhance patients’ ability to do and decide for themselves (Scotto, 2003) [9]. Jean Watson’s theory of Human Caring and Imogene King’s Goal Attainment Theory will guide this study. Watson [10] (2003), believes that caring is the essence of nursing and the most central and unifying focus of nursing practice. She noted that throughout it’s history, nursing has been involved in caring and has actually evolved out of caring. Nursing is a human science of person and human nursing care is something measured from the clients experience and is provided to it’s optimum by the performance of the nurse.According to Henderson as cited by Kozier [11] (2004), individual care is stressed on assisting in essential activities to maintain health, to prevent illness and recover from illness. The knowledge, skills, and attitude of nurses enable them to serve as substitute for whatever the client lacks in order to make the client “competent, whole or independent”. Likewise, she saw nursing as concerned with both healthy and ill individuals, acknowledged that nurses interact with clients even when recovery may be feasible and mentioned the teaching of the nurse. As a nurse begins clinical practice, it is important to consider how clients perceive caring and what are the best approaches in providing care. (Potter and Perry, 2008) [8].
3. Methods
3.1. Design
- The study utilized quantitative-descriptive design with survey questionnaire. Surveys are efficient in that many variables can be measured without substantially increasing the time or cost (Weiss, et al 2001) [12].
3.2. Sampling
- The respondents of this study are third year student nurses who finished the course Maternal and Child Nursing at Benguet State University. The inclusion criterion guarantees that the respondents have experienced assessing postnatal mothers in the clinical setting. Sixty-seven (67) student nurses were chosen as respondents through total enumeration.
3.3. Instrument
- The questionnaire was based from Joint Commission on Accreditation of Healthcare Organizations (JCAHO) standards of nursing practice and Hanan Maternal Child Health and Nutrition (MCHN) Project checklist. Furthermore, closed ended questions were included where in the respondents selected an answer from a list of responses provided by the researcher.The instrument was composed of two (2) parts. The first part includes the respondents’ demographic profile, which consists of their name (optional) and sex while the second part are questions presented in a checklist form, composed of twenty (20) clinical practice protocol divided into four subsets. The four subsets are assessment, plan, implementation and evaluation with three (3), three (3), eleven (11), and three (3) evaluation statements respectively. A four point likert scale ranging from 1 (never) to 4 (always) was used to assess the respondents’ compliance to clinical practice protocols.The researchers personally administered the questionnaires to the respondents who gave consent to conduct the study. About 10-15 minutes was allotted for the respondent to answer the questionnaires. They were collected making sure that the respondents were given sufficient time to answer the questionnaires. After that, the data were tallied, analyzed and statistically tested.
3.4. Ethical Considerations
- Respondents were treated as autonomous agents, who were allowed to make their own decisions regarding their participation in the study. According to Babbie [13] (2008), informed consent in research was based on respondents’ participation, provided they fully understand all possible risks involved. Therefore, the respondents were informed about the purpose and procedures of the study and allowed to ask questions to clarify any uncertainties. Likewise, total confidentiality of the obtained information and respect of the subject’s privacy were ensured.
3.5. Statistical Treatment
- The data were statistically analyzed using the statistical program of Statistical Package for the Social Sciences (SPSS) version-20 (IBM Inc., 2011) [14]. Descriptive statistics including mean and standard deviation was utilized. Mean scores were calculated for each category. Higher scores implied that postnatal care was always practice and lower scores implied that postnatal care was sometimes practice. On the other hand, t-test was used to determine if there is a difference of postnatal care delivered by student nurses when grouped according to sex.
4. Results and Discussion
4.1. Compliance on Postnatal Care when Assessment and Plan are Considered
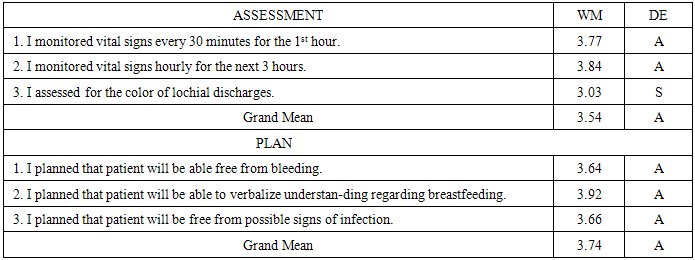
- Table 1 depicts the compliance of student nurses when the following clinical practice protocol of assessment and plan on postnatal care are considered.
|
4.2. Compliance on Postnatal Care When Implementation and Evaluation are Considered
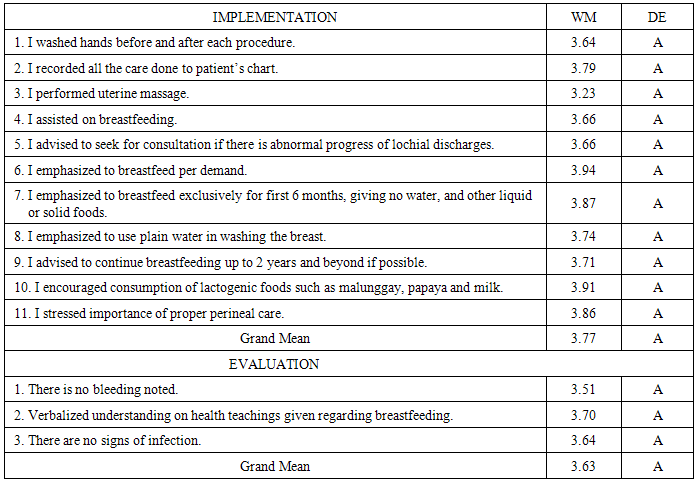
- Table 2 depicts that all the statements presented under the category of implementation were on the level of always where the practice “I emphasized breastfeed per demand” got the highest mean rating of 3.94. On the other hand, the lowest mean of 3.23 was obtained from the statement “I stressed importance of proper perineal care.”
|
4.3. Difference of Postnatal Care by Male and Female Student Nurses
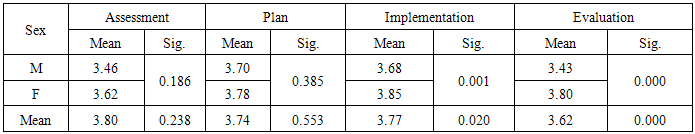
- Table 3 shows that both male and female students always render care during assessment. The T-test shows that the assessment of the male students is not significantly different from that of the female.
|
5. Conclusions and Recommendations
- The following conclusions are drawn:Student nurses generally, always render postnatal care following the clinical practice protocol as to assessment, plan, implementation and evaluation. Results revealed that there is a significant difference among students’ implementation and evaluation practice of postnatal care when grouped according to sex. Meanwhile, it was inferred that there is no significant difference on assessment and plan of care by student nurses. Moreover, the protocol that is most performed by the student nurses in assessment, plan, implementation and evaluation are as follows: ‘I monitored vital signs hourly for the next 3 hours’, ‘I planned that patient will be able to verbalize understanding regarding breastfeeding’, ‘I emphasized to breastfeed per demand’ and ‘verbalized understanding on health teachings given regarding breastfeeding.’Student nurses should further study and understand the clinical practice protocols in rendering postnatal care giving more emphasis on the most common overlooked postnatal problem such as bleeding. It may be important for future studies to include years of exposure to clinical area as one of the considerations in identifying its impact towards the care rendered. Also, having larger sample to ensure generalization of results was suggested. Furthermore, the results of this study may be utilized to nursing practice for emphasis on the standards of postnatal care. To nursing institutions, instructors should be reminded to place emphasis on assessment regarding bleeding.
ACKNOWLEDGEMENTS
- The authors extend their deepest gratitude to faculty members of Benguet State University-College of Nursing for their comments, suggestions, and recommendations of this endeavour. We are thankful to all students who participated in the study, without their wholehearted input this study could not have been possible. This was a non-funded study and there is no conflict of interest.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML