-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Management
p-ISSN: 2162-9374 e-ISSN: 2162-8416
2024; 14(1): 14-26
doi:10.5923/j.mm.20241401.02
Received: Apr. 7, 2024; Accepted: May 5, 2024; Published: May 28, 2024

Quality Improvement and Financial Performance: An Endless Relationship
Marita Issa Ibrahim 1, Amal Abou Fayad 2
1PhD Candidate at Holy Spirit University of Kaslik, Kaslik Lebanon
2Lebanese University, École Doctorale de Droit et des Sciences Politiques Administratives et Économiques, Sin El Fil Beirut Lebanon
Correspondence to: Amal Abou Fayad , Lebanese University, École Doctorale de Droit et des Sciences Politiques Administratives et Économiques, Sin El Fil Beirut Lebanon.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Since 2019, Lebanon has been entangled in a political-economic crisis, which has significantly impacted the healthcare sector. This crisis has led to various challenges, notably a decline in patient care quality due to shortages in medications, medical supplies and human resources. Furthermore, inconsistent adherence to quality standards, outdated medical practices, and a lack of standardized protocols have further worsened variations in healthcare service quality. These challenges, alongside others, have undoubtedly influenced the financial performance and revenue generation of hospitals. The effectiveness of total quality management systems in hospitals in achieving financial performance remains a subject of investigation. Employing a quantitative methodology and distributing a questionnaire to executive management in Lebanese hospitals will offer insights into the following hypotheses: Healthcare team effectiveness is positively associated with financial performance, Patient satisfaction is positively associated with financial performance, Hospital reputation is positively associated to financial performance and Patient care quality is positively associated to financial performance. The findings reveal that a hospital's financial performance is influenced by factors such as patient satisfaction, quality of care, workforce performance, and hospital reputation.
Keywords: Patient care quality, Financial performance, Total quality management, Workforce performance, Healthcare reputation
Cite this paper: Marita Issa Ibrahim , Amal Abou Fayad , Quality Improvement and Financial Performance: An Endless Relationship, Management, Vol. 14 No. 1, 2024, pp. 14-26. doi: 10.5923/j.mm.20241401.02.
Article Outline
1. Introduction
- Nowadays and after the economic depression of 2019, Lebanese hospitals are facing many challenges; lacking human resources, material, regulatory requirements and big competition in market. What can differentiate a hospital from another is its quality-of-care standards and stakeholders’ satisfaction which emphasize the hospital’s reputation. Since 2019, Lebanon has encountered a series of crises, beginning with the economic and financial downturn in October 17, 2019, followed by the global COVID-19 pandemic caused by the spread of SARS-CoV-2, and culminating in the devastating explosion at the Port of Beirut on August 4, 2020. Healthcare sector didn’t have time to breath normally since that black year 2019. Healthcare workforce has to keep, during this time and despite the economic, social, financial and political crisis, a high sense of professionalism and treat patients with high level of quality of care to save lives of many people from patients affected by the pandemic and/or saving life of injuries from Beirut blast. The economic and healthcare sectors are strictly connected to each other, therefore, the necessity of obtaining a high quality of standards is mandatory. According to [1], the population is split into three categories: the first category children and young under 15, second part, working-age population, between 15 and 64 years old and last part, for elderly population above 65. The second part is linked directly to the economic cycle as it requires to work and generate money to take care of the first and third part of the population. Consequently, adopting a healthy healthcare sector with a high quality of standards remains essential. Quality management in hospitals is mandatory to understand fundamental concepts in quality improvement, identify the environment and key steps for a successful quality improvement project, and become familiar with several quality improvement tools and their use. Improved quality delivers better patient care at lower costs with potentially higher reimbursements (pay-for-performance) and it can make our jobs more interesting, fun, and rewarding. Thus, healthcare performance, patient satisfaction, physician satisfaction and reputation may play a leading role in the development and reputation of a hospital. Quality management is considered to be long term investment for the hospital. Quality improvement and financial performance are two critical pillars for the growth of any healthcare institution. That’s why many hospitals in Lebanon and abroad go for more and more accreditation bodies like JCI (Joint Commission International) accreditation, Australian and so on. Does the healthcare workforce performance have any effect on the financial performance? How can patient satisfaction play crucial role? Are there any consequences from the hospital reputation on the hospital financial performance? What is the relationship between the quality of patient care and the hospital financial performance? To address our research question, we will undertake the following methodology: conducting a comprehensive literature review, performing quantitative analysis through surveys administered to hospital executives in Lebanon, analyzing the gathered data, and drawing conclusions based on our findings.
2. Literature Review
2.1. Total Quality Management Practices
- According to [2], nowadays the total quality management (TQM) system has become a priority to organizations and government. Thus, [3] has affirmed what it has been stated by [2] and added that the philosophy of administration has positive effect on the quality of services or goods provided to customers, the organizational success, and the rapid work environmental changes. TQM is mandatory for management success [4]. Continuous improvement of internal and external operations of services is the basis of the total quality management that ends up meeting the clients’ needs [2]. As we are in a globalized world with extreme competition in internal and external markets, quality improvement becomes mandatory to provide high-quality products or services [5]. According to [6], patients’ or consumers’ satisfaction is the principal tool used in total quality management to measure quality of service provided in healthcare institutions. To enhance patients’ satisfaction, we rely on perceived service quality (PSQ). Not only private health institutions are committed to a quality improvement system, but public institutions are committed to understanding patients’ needs and elements affecting their satisfaction [7]. However, using patients’ satisfaction survey is one of the best and most reliable tools that truly reflects the performance of the health institutions in measuring the quality of healthcare services [8]. Total quality management has been introduced recently in healthcare; TQM effects on PSQ, patient satisfaction and behavior intentions have been concerned with focusing on manufacturing industry and forgetting healthcare [7]. Additionally, TQM & PSQ have been measured in developed countries rather than Arab countries, especially in Palestine, according to previous empirical studies [9]. TQM aims to achieve customers’ and consumers’ needs by focusing on continuous quality improvement of all processes and functions; thus, this is considered as a way of successful organization management [10].The objective of continuous quality improvement is to establish efficient mechanisms and protocols that ensure the delivery of high-quality products and services to customers. By implementing these measures, customers will receive satisfactory service, leading to increased satisfaction and overall happiness [11]. Quality process, service quality, product quality, and strong operating system led to clients’ satisfaction, according to the ISO 9001:2015 standards. Healthcare loyalty patient is identified by the following four factors from service quality perspective: quality, interaction quality, environmental quality, and outcome, as defined by literature.
2.1.1. Perceived Service Quality (PSQ)
- According to [12] the perception of the service quality is obtained by an assessment form to test the quality of offered services and meet clients’ expectations. For customers retention and loyalty, customer satisfaction assessments are mandatory. PSQ is how patients in the healthcare industry judge the health service they receive from the hospital, or their opinion of the health service quality they get [13]. The hospital’s medical service is not something you can own or touch, but it uses various tools, devices and equipment to serve the patient and then take them back. It can last for a short or long time. PSQ is composed of five factors: Tangibles, Reliability, Responsiveness, Assurance and Empathy [14,15].
2.1.2. Patient Satisfaction
- Customer, consumer or patient satisfaction is evaluated after the use of the product or service in healthcare [16,17]. In the healthcare sector, assessing the quality of services provided to patients involves determining the extent to which those services have fulfilled the needs and expectations of patients [18]. By questioning patients, we may assess their evaluation regarding the offered service and to which extent they are satisfied or unsatisfied from the quality of the offered service. In other words, perceived service quality and customer expectations are the key components in the satisfaction survey [19].
2.2. Role of Management in Implementing Total Quality Management
- TQM is implemented and maintained by the management and leadership engagement and commitment [20,21]. Effective leadership is an essential key in TQM [22]. By creating vision and promoting change in a TQM context are essential roles for top management to implement and improve the TQM successfully [23]. Throwing out old mentalities for quality managers and defining new strategies for new quality managers must be implemented by defining leaders who set new goals and quality initiative on the good track [24]. TQM is a strategy used by all the leaders in executing and implementing those strategies. (Quality planning, human resource management, learning and customer focus) [25]. Again, to implement all of the cited strategies, effective and strong leadership is the primary key [26]. Services are offered by employees. Thus, employees must be motivated and persuaded while working in hospitals to deliver a quality of service. Consequently, those employees are persuaded with leadership skills of managers that affect the operational and financial performance. So, TQM practices are influenced by effective top management leadership skills leading to achieve sustainable set goals [27,28].
2.3. Patient-Centric Care Quality and Satisfaction
- The highest standards of medical care offered to patients determine the patient care quality (PCQ) [29,30]. Four dimensions constitute the patient care quality: interpersonal, technical, environmental and administrative quality [31,32].1. Interpersonal: it aims at the relationship and healthy communication between healthcare team and patient from respect, personalized attention and confidentiality [31,32]. 2. Technical: healthcare workforce performance, expertise, professionalism and competencies are essential components in delivering the highest medical quality of care quality to patients. For instance (X-rays and lab tests) results are considered critical results and requires competent team [31,33].3. Environmental quality: being hospital patient friendly, the following concepts must be taken into consideration: hospital hygiene and cleanliness, lighting, normal temperature, good quality of tangible assets like bed and all the requirement needs of every patient [31,34].4. Administrative: administrative work is not least important than medical care. It coordinates with internal hospital services, decrease waiting time at the hospital, support new services, control billing records and documentation to be free from mistakes [31,35]. In addition to the key factors discussed regarding perceived quality care, it is essential to pay attention to the matter of medical treatment expenses. In the U.S. healthcare, most patients are covered with health insurance that is an intermediate link between patient and hospital to cover hospital/physicians’ expenses. Research has found that patient and physicians must adhere to the medication schedule because this adherence will determine the medical expenses especially to chronic patients such as diabetes and hypertension [36], anxiety and depression [37] and asthma [38]. Cost efficiency and practical quality of care are interrelated [39].Consequently, patient satisfaction measures the level of satisfaction from offered services with the healthcare. Evaluation of patient satisfaction is a key performance indicator that spotlight marketing work [30,31]. This indicator is affected directly by computerized and electronic clinical orders by physicians [40].
2.4. Hospital Outcomes
- According to healthcare literature made by [41], it has presented the positive effect of patient satisfaction on the hospital’s reputation and consequently, its financial performance. Reporting positive ratings to public is mandatory to improve hospital reputations [42]. Moreover, to patient safety and quality perceptions strong relationship affect it [43]. Hospitals abiding by serious and strong quality improvement plan their financial performance will be affected positively [44]. Physicians’ engagement and involvement in the hospital governance improves financial performance [45] in addition to the importance of relationship between hospital strategic planning processes and financial performance [46]. Integrating physicians in hospital interests is mandatory, as his/ her individual reputation is strongly correlated to the hospital reputations [47].
3. Research Methodology
3.1. Research Methods
- Despite the various research methods discussed above, it is imperative to delve into detailed descriptions of the following methods: qualitative and quantitative.
3.1.1. Qualitative Method
- This method relies on collecting deep details on a specific topic. It allows us to represent feelings, thoughts and emotions of the person while explaining any subject. Researchers observe and interpret an action in order to get out by a conclusive theory [48].
3.1.2. Quantitative Method
- This method relies on a scientific method as the positivist paradigm [49]. This method ignores all feelings and subjective reasoning. It relies only on analyzing statistically fresh data collected. Similarly, researchers adopt data description rather than data interpretation. They work objectively and opinions are measured numerically.
3.2. Types of Variables
- “Variables” are the most used word in any research. While conducting quantitative research, it is obvious to define and clarify each variable. Variables are welcomed more than constants in research. As an example, we may list the following types: Independent & dependent variables, Active and attribute variables, Continuous, discrete, and categorical variable, Extraneous variables and Demographic variables. Independent variables are considered to be as antecedent variables. However, dependent variables are consequent. Thus, when independent variables are active, they do manipulate and affect the other variable. Usually, dependent variables are affected by the independent one. In this research, we used both dependent (financial performance) and independent variables (healthcare team performance, hospital reputation, patient satisfaction, quality of care) [50].
3.3. Measurement Scale
- Likert-type scales are the most used measurement scales in theses [51]. They usually rely on five or seven responses categories. Commonly used are the 5-point Likert scale which increases the quality of responses and reduce the respondent frustration level.
3.4. Sampling Data Collection
- According to the Syndicate of Hospitals (site visited on 14/01/2024), there are 27 private hospitals in Beirut and 9 between Jbeil and Kesrwan district. Main hospitals are located in the biggest districts in Beirut, Jbeil and Kesrwan. Mentioned districts are considered the heart of Lebanon as they are the engine of the economic and tourism activity due to the population density, historical significance and well-structured infrastructure. The whole number of private hospitals in Lebanon is 134 hospitals (21 hospitals in Bekka, 12 hospitals in Chouf/Aley, 27 hospitals Metn/Baabda, 21 hospitals in North and 17 hospitals in South, In additionto 29 government hospitals [52]. Therefore, the total number of hospitals in Lebanon is 163 hospitals including both private and public sectors. Thus, the required sample size is 115. However, since this sample size exceeds 5% of the population (163*.05=8.15), Cochran’s correction formula should be used to calculate the final sample size [53]. These calculations are as follows:
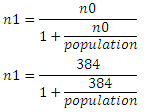 n1= 114.42 (115)Where population size = 163Where n0 = required return sample size according to Cochran’s formula= 384Where n1 = required return sample size because sample > 5% of populationThese procedures result in a minimum returned sample size of 115.
n1= 114.42 (115)Where population size = 163Where n0 = required return sample size according to Cochran’s formula= 384Where n1 = required return sample size because sample > 5% of populationThese procedures result in a minimum returned sample size of 115. 3.5. Data Treatment
- SPSS (Statistical Package for the Social Sciences) is an advanced statistical software used to analyze quantitative data; it combines machine learning algorithms, string analysis and big data analysis. To navigate in this program, researchers must have the know-how of this program. Its latest version is updated in 2019 and considered the 25th [54]. Every scientific research relies on statistical tests that influence the remarks on the research outcomes. In 1993, Black pointed out that a change may occur in the research and change the analysis of the data. Therefore, data selection and decision process are not included in the statistical analysis [55].
3.6. Reliability Measurement & Validity
- For reliability measurement, we referred to Cronbach’s alpha method. This method is used to test the consistency and interrelation of tested questions [56]. A common interpretation of the coefficient is as follows:• α < 0.5 for low reliability • 0.5 < α < 0.8 for moderate (acceptable) reliability • α > 0.8 for high (good) reliability. Small tested questions and lot of heterogeneity of measured items that are poorly interrelated results for a low reliability with an α < 0.5.
3.7. Correlation Coefficient Test
- The direction of the relationship between variables and the strength of the linear relationship is found by the correlation coefficient test called Cramer’s V or Phi. Positive correlation is indicated by a unidirectional relationship of two variables. So, when the variable X is high, the variable Y will be high. However, negative correlation shows inverse relationship between variables. Consequently, variable X is high, variable Y will be low, and vice versa [54]. The following criteria are used to identify the strength of the correlation between two variables:• 0 means There is no correlation between two variables • > 0.00 – 0.25 means the correlation is very weak• > 0.25 – 0.50 means enough correlation• > 0.50 – 0.75 means strong correlation• > 0.75 – 0.99 means the correlation is very strong • 1.00 means perfect correlation
3.8. Research Hypothesis
3.8.1. Healthcare Team Effectiveness and Financial Performance
- The variety and scope of clinical knowledge within teams significantly impact both patient care and organizational performance [57]. Factors such as collaboration, conflict resolution, participation and cohesion play crucial role in enhancing staff satisfaction. Cross-functional teams are mandatory in hospitals to implement and follow-up quality practices due to their commitment [58,59]. Teamwork is crucial in the quality management philosophy [60] as this kind of cooperation will let healthcare team perform their routine tasks in other ways and learn from each other. For instance, small surgical team members learn from each other during workload and complex operations [61]. Physician empathy [62] and nurse emotional involvement [63] are the essential components in influencing interpersonal relationships. For better interpersonal quality of patient care, communicating clearly result to the patient and or his/her kin, quicker his/ her cure and being active towards his pain are done by effective healthcare ream [64].Electronic health records (EHR) and up-to-date information increase patient’s health as all the information are adequate, accessible and readily available to physicians for decision making and nurses support [65,66,67].Besides that, good environmental quality must be in place. Hospital hygiene from staff hand hygiene and hospital beds, clothes and equipment must be in an extremely high level of cleanliness [68,69]. That’s why workforce must follow hospital hygiene procedures very carefully to prevent infection among patient by cleaning and disinfecting beds and other medical and surgical equipment [70].Hospital administration departments like billing and reception tend to think that they are working separately in isolation than nursing departments. In fact, that’s not the reality at all, as they are supporting other healthcare teams in providing the best of quality in patient care [71,72]. By healthcare team, information must be disclosed to patient and or his/her kin on a timely basis especially on their administrative steps such as scheduling hospital visit appointments, providing food and dietary information related to the sickness to the patient or to their kin, explaining healthcare decision making processes to patients, and when required, interacting with the hospital’s administrative departments on behalf of patients [73]. Drawing from the preceding discussions, it is recommended that for optimal effectiveness, healthcare team members should collaborate seamlessly. This entails preemptively verifying schedules and ensuring room/equipment availability ahead of patients' medical procedures, implementing measures to prevent hospital-acquired infections, and consistently prioritizing patient care in their decision-making processes [73].Therefore, drawing from tenets of QM philosophy we propose the following hypothesis:H1: Healthcare team effectiveness is positively associated with financial performance.
3.8.2. Patient Satisfaction and Financial Performance
- Patient satisfaction must be improved in healthcare what improves directly the treatment outcomes [74]. It is considered to be the defining core of all medical treatment philosophy. Empirically speaking, by having high levels of nurse-staffing in hospitals, high quality of care and good patient experience will be provided [75]. Several articles have noted that patient satisfaction might not necessarily correlate directly with the quality of medical treatment [76,77]. Hospitals and physicians may prioritize satisfying patients without necessarily ensuring the precise medical treatment required for curing their ailments [78]. However, empirical research in healthcare and marketing literature presents evidence supporting a positive association between patient care quality and patient satisfaction [29,31]. We therefore posit: H2: Patient satisfaction is positively associated with financial performance.
3.8.3. Hospital Reputation and Financial Performance
- Hospital reputation is correlated to individual physicians’ reputation [79]. In other words, building and sustaining a safety culture in medicine is extremely important. Establishing and maintaining a safety culture within hospitals faces distinctive hurdles due to the professional norms in medicine. The prevalent emphasis on holding individuals accountable for errors frequently leads to a culture of "blaming and shaming," where individuals are held responsible for mistakes occurring under their supervision [80]. Due to fear of losing their nursing, doctors and administrative staff they remain silent in unsafe conditions or errors [81]. Besides that, we do not forget the importance of quality control of suppliers and medical equipment that may affect patient harm, quality of care offered and by that loss of reputation and image [82,83].On one hand, dissatisfied patients may spread negative experience, bad word of mouth and express their anger on social media [84] which could harm both individual physicians’ reputation and hospital reputation. On the other hand, positive experience and satisfied patient may spread good word of mouth bout physicians and hospitals facilities and quality of care. Nurses play major role in ensuring patient safety, quality of care and consequently hospital’s financial performance by adopting preventive action [85].A recent study from the Deloitte Center for Health Solutions—The Value of Patient Experience—reports that enhancing customer loyalty, building reputation and brand and boosting new services will improve hospitals’ financial performance [86].For an extended period, the Centers for Medicare and Medicaid Services (CMS) have integrated patient-reported experience scores into their assessment criteria. These scores, which influence a hospital's reputation, are utilized to determine reimbursements and incentives or penalties for hospitals participating in Medicare's Value-Based Purchasing program.Therefore, based on the above discussions, we propose: H3: Hospital reputation is positively associated to financial performance.
3.8.4. Patient Care Quality and Financial Performance
- To be integrated in quality initiatives, teams need to be directed by leaders. According to the quality management philosophy, senior management plays a crucial role in educating and training people to make the environment conducive for teams to work [60]. When the hospital financial performance is healthy, its aim is not only to deliver the good quality of service to all stakeholders but to put quality improvement efforts on physicians, nurses and staff by improving resource allocations to the departments as necessary, e.g., hospital facilities expansion, internal technology infrastructure upgrades. Hospitals with good reputation are managed by reputed doctors [87] that consequently facilitate the born of new well reputed doctors [88] and certainly will lead to improve patient experience at the hospital [89]. Hospitals always aim to abide by high perceived quality of care standards in order to be ranked publicly the first and attracting higher rate of good patients [90]. Therefore, based on the above long-term phenomena our final hypothesis is: H4: Patient care quality is positively associated to financial performance. In relevance to the above four hypotheses, below a conceptual model to be tested. Figure 1: Conceptual framework.
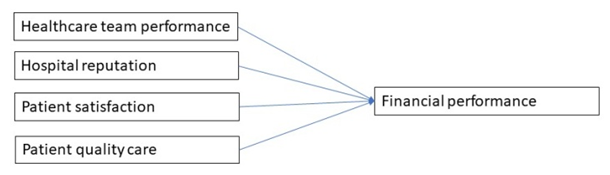 | Figure 1. Conceptual framework. (Source: Elaborated by author.) |
4. Results of the Quantitative Analysis
4.1. Reliability Measurement & Validity
- For reliability measurement, we referred to Cronbach’s alpha method. This method is used to test the consistency and interrelation of tested questions [56].A common interpretation of the coefficient is as follows:• α < 0.5 for low reliability • 0.5 < α < 0.8 for moderate (acceptable) reliability • α > 0.8 for high (good) reliability. Small tested questions and lot of heterogeneity of measured items that are poorly interrelated results for a low reliability with an α < 0.5.
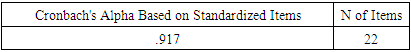 This means that for the 22 questions testing all the hypotheses have an α = 0.917 > 0.8 indicating a high reliability.
This means that for the 22 questions testing all the hypotheses have an α = 0.917 > 0.8 indicating a high reliability. 4.2. Correlation Coefficient Test
- The direction of the relationship between variables and the strength of the linear relationship is found by the correlation coefficient test called Cramer’s V or Phi. Positive correlation is indicated by a unidirectional relationship of two variables. So, when the variable X is high, the variable Y will be high. However, negative correlation shows inverse relationship between variables. Consequently, variable X is high, variable Y will be low, and vice versa [54]. The following criteria are used to identify the strength of the correlation between two variables:• 0 means There is no correlation between two variables • > 0.00 – 0.25 means the correlation is very weak• > 0.25 – 0.50 means enough correlation• > 0.50 – 0.75 means strong correlation• > 0.75 – 0.99 means the correlation is very strong • 1.00 means perfect correlation
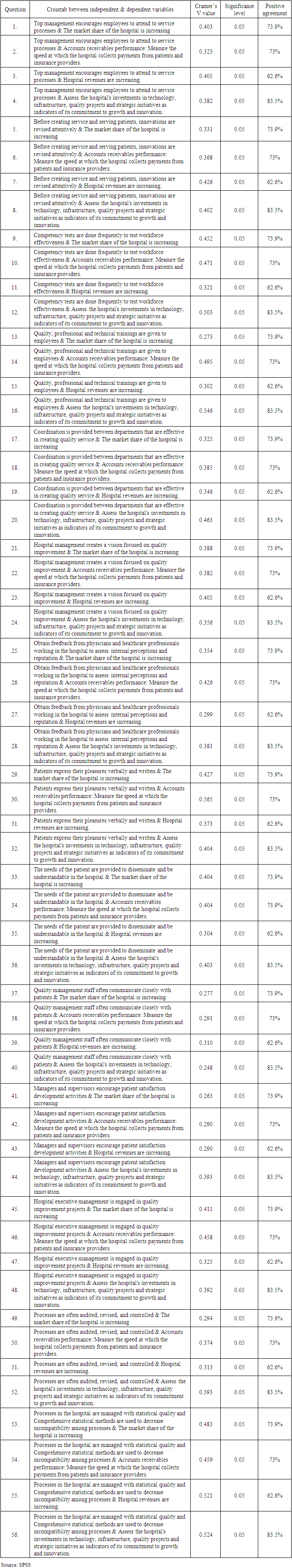
4.3. Results Discussion & Analysis
- According to SPSS results for the survey conducted, 27.83% of respondents were males and 72.17% were females. However, 55.65% from respondents were occupying Chief quality officer position, 8.7% from respondents were occupying Chief nursing officer position, 7.83% from respondents were occupying Chief operating officer position, 6.96% from respondents were occupying director of patient services position, 6.09% from respondents were occupying Chief financial officer position, 5.22% from respondents were occupying Chief executive officer position, 5.22% from respondents were occupying Chief medical officer position and 2.61% from respondents were occupying Chief human resources officer position. The participating hospitals in this study were: 16.52% from Notre Dame de secours University Hospital- Jbeil, 3.48% from Saint Georges Hospital Ajaltoun, 3.48% from Child and Mother Welfare hospital, 1.74% from Hopital Notre Dame de Liban, 1.74% Hotel Dieu de France, 1.74% Dar Al Ajaza Al-Islamia Hospital, 0.87% Al Rassoul Al Aazem Hospital and 70.43% to other hospitals. First, the results (from Q1 à Q16) using of table 1 SPSS software show a significant level less than 0.05, meaning that there is a correlation between dependent and independent variables. And a correlation coefficient value Cramer's V indicating that there is correlation. In accordance to all crossmatch functions, having a positive percentage of full agreement (combination between strongly agree and agree) higher than 50% with a verified correlation between dependent and independent variables, this approves that H1: Healthcare team effectiveness is positively associated with financial performance is verified.
|
5. Conclusions
- In conclusion, the fundamental practices to deliver high-quality healthcare are in assessing clinical guidelines, protocols and standards of care to be followed by healthcare workers. In addition to good clinical practices, healthcare policies and regulations need to be examined in order to identify areas for improvement and ensure compliance with standards. Infrastructure and resources need to be reviewed adequately in terms of quality and availability to support patient safety and the delivery of quality care. The evaluation of Health information system (HIS) is mandatory to deal with patients’ information management, facilitate communication among healthcare providers in order to enhance the efficiency of care. Patient safety and quality improvement aims to minimize risk of errors, increase patient and elaborate a quality improvement culture. Briefly, due to the economic crisis, the current state of healthcare in Lebanon is suffering from many challenges in terms of quality of care and financial pressures. The healthcare sector across Beirut and various regions of Lebanon is confronted with multiple shortages, including those of human resources, medical supplies, and equipment, leading to a decline in the quality of care provided. Furthermore, accessibility to healthcare services is becoming increasingly difficult for individuals seeking treatment in reputable hospitals, primarily due to the escalating costs of medical services coupled with high unemployment rates and inflation nationwide. The ongoing financial crisis in Lebanon is exacerbating the challenges faced by hospitals, as they grapple with difficulties in compensating their staff, procuring essential medical supplies, and upkeeping their facilities, primarily attributable to the liquidity constraints within the country's banking system. All the efforts are already addressed to overcome these challenges but the situation remains always difficult for both healthcare providers and patients in the city. Despite what some executive directors think that quality is less important and cost the hospital, that’s why they prefer to invest in rapid direct return instead of costs, quality management practices in all its areas remain mandatory to the continuity and progressive reputation of hospital. Investing in buying a new machine and getting a quick return on investment is not always the best decision for the development of the hospital. Investing in quality management practices, adherence to policies, procedures, protocols, national and/or international accreditation standards, stakeholder satisfaction, etc. is favorable sometimes. Good reputation will increase hospital’s shares certainly by those employees, and physicians will be rewarded. Patient satisfaction plays a crucial role in affecting the hospital’s reputation and consequently, the financial performance. Workforce performance, engagement, discipline, enthusiasm, and productivity are extremely important in satisfying our consumers. Thus, patient care quality associated with stakeholder satisfaction affects the financial performance from revenue, shares and investments of any hospital. Finally, is good quality management system the only engine for the healthcare growth?
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML