-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Microbiology Research
p-ISSN: 2166-5885 e-ISSN: 2166-5931
2023; 13(1): 1-5
doi:10.5923/j.microbiology.20231301.01
Received: Mar. 31, 2023; Accepted: Apr. 12, 2023; Published: May 23, 2023

Prevalence of Hepatitis C Virus among Blood Donors in Brazzaville, Republic of Congo
Brunel M. Angounda1, 2, Serge O. Mokono1, 3, Oscar Akombo Itoua1, Geneviève B. Boukatou1, Boris S. Bakoua1, Edwige P. Lc. Nanitelamio1, Elira Dokekia A.3
1National Center of Blood Transfusion, Brazzaville, Congo
2Faculty of Sciences and Technology, Marien NGOUABI University, Brazzaville, Congo
3Faculty of Health Sciences, Marien NGOUABI University, Brazzaville, Congo
Correspondence to: Brunel M. Angounda, National Center of Blood Transfusion, Brazzaville, Congo.
| Email: |  |
Copyright © 2023 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Hepatitis C is a global health problem and transfusion of the contaminating blood products is one of the most important mechanisms for its transmission. The aim of this study is to determine the prevalence of the HCV infection among the potential blood donors in Brazzaville, Republic of Congo. A cross-sectional study was conducted from January 2019 to December 2020 among 594 blood donors in the National Blood Transfusion Center of Brazzaville. The socio-demographic characteristics and associated risk factors were collected using a standard questionnaire. Screening of HCV was done by using the ELISA tests and P-value of less than 0.05 was considered as statistically significant. The overall prevalence of the HCV was 4.18% (95% CI:2.47-5.89). The positive cases were more prevalent among males, replacement donors and those who were less than 30 years old (68.2%). The gender of donors (P=0.04) and those with a multiple sexual partners (p = 0.019) were found to be associated with the higher risk for the HCV infection. However, there was no significant association with the history of surgery and tattooing. The present study reveals that the HCV infection is more prevalent among the blood donors in Brazzaville.
Keywords: Hepatitis C virus, Blood donors, Prevalence, Brazzaville
Cite this paper: Brunel M. Angounda, Serge O. Mokono, Oscar Akombo Itoua, Geneviève B. Boukatou, Boris S. Bakoua, Edwige P. Lc. Nanitelamio, Elira Dokekia A., Prevalence of Hepatitis C Virus among Blood Donors in Brazzaville, Republic of Congo, Journal of Microbiology Research, Vol. 13 No. 1, 2023, pp. 1-5. doi: 10.5923/j.microbiology.20231301.01.
Article Outline
1. Introduction
- Hepatitis C virus (HCV) is a major cause of acute and chronic hepatitis, which can progress to liver cancer [1]. The main routes of HCV transmission are perinatal exposure, blood transfusion, different surgery and other routes of transmission such as, family contacts [2]. Chronic Hepatitis C Virus infection (CHC) is a world health problem, affecting more than 71 million people and causing about 500,000 deaths each year. Moreover, it is estimated that, there were 1.75 million new HCV cases [3,4]. Central Africa is considered as a high-prevalence region of anti-HCV antibodies, detected in about 2–20% of the population [5,6,7]. HCV is transmissible by blood transfusion and is known to be the major cause of post-transfusion HCV infections [8]. The risk of acquiring HCV from blood transfusion varies between 20–40% in countries where blood is not routinely screened for HCV [9]. In Africa, only 19% of blood is screened for HCV (anti HCV antibodies). The main reason for this low screen rate is the prohibitive cost of the laboratory tests. Also, inconsistent screening procedures for blood donors make blood transfusion a major means of acquisition of HCV infection [9]. The Republic of Congo is considered as a high prevalence area of the HCV infection, with an estimated seroprevalence of 5.6% [10]. In the previous study conducted in 2014 in Pointe Noire, the seroprevalence of anti-HCV antibodies in the blood donors has been reported to be at 4.7% [11]. Meager information regarding the prevalence of HCV infections among blood donors in Brazzaville. Such data are important to understand the burden of infection in different donor subgroups and to predict the future prevalence for public health purposes. So, the present study is designed for the detection of the sero-prevalence of HCV infection among blood donors in Brazzaville, Republic of Congo.
2. Methods and Methods
2.1. Study Design, Data Collection and Processing
- This cross-sectional prospective study was carried on the blood donors who attended at the National Blood Transfusion Center in Brazzaville, republic of Congo, from January 2019 to December 2020. All subjects were interviewed by trained physicians using the post-donation questionnaire containing the demographics, socioeconomic status and other background characteristics. Risk factors such as sexual behaviors, injection risk, history of blood transfusion, history of surgery and dental procedures, were also included. Samples were collected on dry tubes from donors during blood donation, centrifuged at 4000 g for 5 minutes and collected serum were tested using the Enzyme-Linked Immunosorbent Assay (ELISA) (Monolisa® HCV Ag-Ab ULTRA kit, Bio-Rad, Marnes-la-Coquette-France) according to the manufacturer instruction.
2.2. Statistical Analysis
- Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS, Chicago, IL) version 21. Differences between categorical data were assessed with the Chi-Square test or the Fisher’s exact test. Logistic regression was used to determine the level of association by calculating the Odds Ratio (OR) and 95% confidence interval (95%CI). P-values <0.05 (two-tailed) were statistically significant.
3. Results
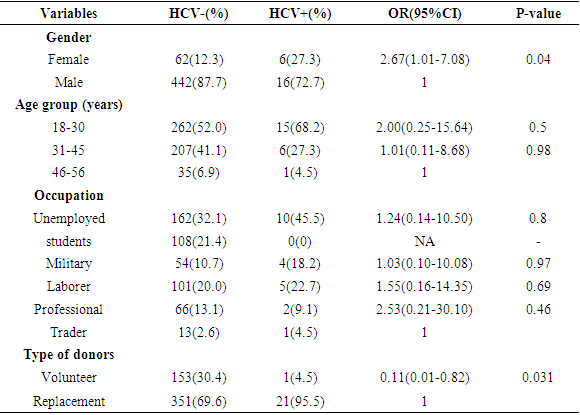
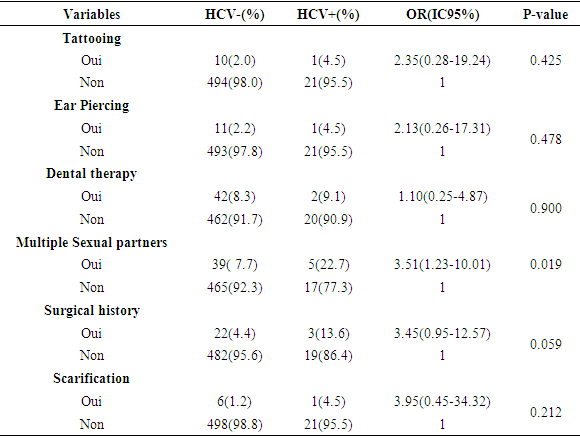
- A total of 526 blood donors were included in this study. The age of the blood donors varied between 18 and 56 years, with a mean of 34,92 ± 9,37 years. Most of the donors were the males (87.1%), and 68(12.9%) were females. Participants were primarily unemployed (172; 33.7%) and students (108; 20.5%) whereas the minority of the donors were trader (14; 2.7%). Moreover, the majority of the blood donors were replacements at 372 (70.7%), compared to 154 (29.3%) who were volunteers.Overall, the prevalence of HCV among the study population was found to be 4.2%. The males blood donors had the highest frequency with 16(72.7%) while only 6(27.3%) of the subjects was a female. There was a significant difference (P < 0.05) between the donors. The age group of 18-30 years had the highest prevalence of 15(68.2%). Regarding occupation, a high proportion was found among unemployed donors (45.5%), followed by laborer workers (22.7%), and military (18.2%), whereas the lowest proportion was observed among professional workers (9.1%) and trader (4.5%). The difference in the seroprevalence of HCV among donors in relation to their occupations was not statistically significant (P > 0.05) (Table 1). A high proportion was found among replacement donors (95.5%). However, the difference in the results of HCV among and replacement donors was not found to be statistically significant (OR=0.11) (Table 1). The relationship among possible risk factors and HCV infection in Table 2 revealed a significant (P < 0.05) association in multiple sexual partners (OR=3.51 and p = 0.019). There was no significant association with history of tattooing, history of dental therapy, history of ear piercing, history of scarification or history of surgical (Table 2).
|
|
4. Discussions
- Hepatitis C virus is emerging as an important transfusion transmissible infection that is associated with chronic liver disease such as the cirrhosis and hepatocellular carcinoma [1]. The blood transmission of the virus via blood and blood products have been the public health concern, particularly in developing countries where the issue of unsafe blood remains a major challenge [2].The seroprevalence of the HCV in the current study was 4.2% which was comparable with other studies done in other countries 4% in Ghana and 4.3% in Egypt [12,13]. The present study is slightly higher than studies conducted in Burundi which were 1.12%, 1,1% in Brazil and 1.58% in Morocco [14,15,16]. However, the prevalence was lower compared to the previous studies among the blood donors in other countries, 12.5% in Cameroon, 7.8% in Georgia, 8.7% in Burkina Faso and 12.3% in Nigeria [17,18,19,20]. These variations in the prevalence of HCV infection in the different parts of the world could be a result of a combination of several factors including, different risky behaviors at different geographical locations and the level of awareness in the different regions of the country. In addition, the quality of the primary screening test and the effectiveness of their blood donor screening program could account for these variations. The age group of 18-30 years old had the highest prevalence compared to other age groups. This showed that the HCV infection is seen more in the younger age groups. Similar study was done in Pakistan where the age highest prevalence of HCV was 18-26 years old followed by 27-32 years [21]. Another study in India showed the highest prevalence of HCV among replacement donors blood donors in age group 18-30 years [22]. However, this pattern of transmission where the infection rate declines in persons greater than 40 years old, suggests that the risk for HCV infection was greater in the distant past and reached a decreased risk of infection along generations as consequence of improving sanitary [15].In our study, the male blood donors were more likely to be infected with the HCV infection than female donors. This result agreed with studies done in other countries and suggests that males were more likely to be exposed to sources of infection (shared use of razors and shaving at barbershops) [23,24]. In addition, this may also be due to the fact that fewer women than men donate blood and are screened.HCV seropositivity was found to be lower in our voluntary donors as compared to replacement donors which is similar to other blood donors studies [25,26]. This is because voluntary donors donate without any pressure and can better understand the implication of donor questionnaire. On the other hand, replacement donors, feel it is necessary to donate out of their parents’ death and therefore may conceal answers about their health and sexual habits.Our results indicated that there was a significant association with the type of donors at the sexual risk regard to HCV infection. This agrees with a study carried out by Okafor et al., in Nigeria, which reported that the percentage prevalence of the multiple sex was at its peak among donors aged 40-49 years [27]. This may be explained with the fact that most of the HCV-positive donors are male and at this particular age group, they are sexually active and in a better position to keep as many sexual partners as possible. Our study demonstrates the insignificant risk of dental therapy and surgical history. On the other hand, studies carried out in Iran, Sudan, Pakistan and Thailand reported that the occupational status, history of surgery, history of blood transfusion, ever pricked by sharps, habit of injecting drugs, glass sharing and donors who had many sexual partners or had sex with a commercial sex worker were significantly associated with occurrence of the hepatitis C [28,29,30].
5. Conclusions
- The results of our study showed a high prevalence of HCV among blood donors in Brazzaville. The prevalence is high for blood donors under 30 and replacement donors. Therefore, strict selection of blood donors with an emphasis on getting voluntary donors and screening donor blood for HCV using standard methods are strongly recommended to ensure the safety of blood for HCV recipient. HCV prevalence needs to be studied on a larger scale to better understand the impact on the clinical status and treatment response.
ACKNOWLEDGEMENTS
- We are really thankful to all blood donors for acceptation to participate and National Blood Transfusion Center who assisted us in providing the resources for this project.
Conflict of Interest
- There is no conflict of interests regarding the publication of this paper.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML