-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Microbiology Research
p-ISSN: 2166-5885 e-ISSN: 2166-5931
2016; 6(3): 65-67
doi:10.5923/j.microbiology.20160603.03

Comparative Study of Modified Acid Fast Stain and Rapid Saffranin Method for the Better Detection of Cryptosporidium, Isospora and Cyclospora Oocysts in HIV Diarrhoeal Samples
Chanu ON1, Srikanth NS2, Muralidharan S2
1Dept. of Microbiology Sikkim Manipal Institute of Health Science, Gangtok, India
2Dept. of Microbiology, St. John Medical College, Koromangala, India
Correspondence to: Chanu ON, Dept. of Microbiology Sikkim Manipal Institute of Health Science, Gangtok, India.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Intestinal coccidian infection is a major health problem in a developing country like India, having the largest number of people living with HIV in the world. Objectives: 1. To detect opportunistic parasites in HIV/AIDS positive patients with diarrhoea. 2. To compare the performances of modified acid fast and rapid saffranin method for the detection of Cryptosporidium species, Isospora species and Cyclospora species in HIV/ AIDS patients with diarrhoea. Intestinal coccidian infection is a major health problem in a developing country like India, having the largest number of people living with HIV in the world. This study includes 80 stool samples from AIDS patients with diarrhoea attending St.John medical college and hospital, Bangalore. Cryptosporidium species and Isospora speciesoocysts were detected using modified acid fast stain and rapid saffranin method. This was done in stool samples before and after concentration. Cryptosporidium species oocyst (2.5%) was detected in the stool samples stain with modified acid fast stain before stool concentration. An additional Cryptosporidium speciesoocyst (18.75%) was detected following stool concentration. Isospora species oocyst (11.25%) was detected following formalin ether concentration technique. Of the Cryptosporidium oocyst (3.7%) detected by the modified acid fast stain was also seen using the rapid saffranin method following stool concentration method. Cyclospora oocysts were not detected. Both modified acid fast stain and rapid saffranin method are useful in demonstrating oocysts of Cryptosporidium species and Isospora species. Stool concentration improved detection of oocysts.
Keywords: HIV and AIDS patients, Diarrhoea, Modified acid fast stain, Rapid saffranin method
Cite this paper: Chanu ON, Srikanth NS, Muralidharan S, Comparative Study of Modified Acid Fast Stain and Rapid Saffranin Method for the Better Detection of Cryptosporidium, Isospora and Cyclospora Oocysts in HIV Diarrhoeal Samples, Journal of Microbiology Research, Vol. 6 No. 3, 2016, pp. 65-67. doi: 10.5923/j.microbiology.20160603.03.
1. Introduction
- India has the distinction of having the largest number of people living with HIV in the world and the adult prevalence rate of 0.91%, is increasing [1]. Intestinal coccidian infections including Cryptosporidium, Cyclospora and Microsporidia are increasingly becoming prevalent in acquired immunodeficiency syndrome (AIDS) patients [2]. In immunocompromised patients, the intestinal opportunistic parasites probably play a major role in causing chronic diarrhoea accompanied by weight loss [3]. Cryptosporidiosis remains an important cause of diarrhoea in the immunocompromised due to the lack of effective therapy. Cryptosporidiosis in HIV infected patients has been widely reported in India [4]. A conventional method for identification includes wet mount, trichrome stain, merifluor stain & auramine –rhodamine stains. [12] These methods are time consuming and trichome stains results cannot give the confirmation for Cryptosporidium, as all oocysts will appear unstained [12]. There is also a lack of appreciation of the importance of this opportunistic parasite in immunocompromised host because of the low prevalence. Therefore failure to diagnose and difficulty in testing of these infections early may interfere with therapeutical procedures, leading to high morbidity and mortality. [5]Because many patients with AIDS are being seen in India, the accurate identification of these opportunistic enteric parasites will become more important for diagnosis and management of these patients [6]. It is necessary to document the public health significance of this infection in immunocompromised hosts in order to formulate more rational approaches to the control of these diseases, especially in the developing countries like India [7]. The present study was under taken to study the prevalence of opportunistic parasites which causes diarrhoea and their association with their status in HIV/AIDS patients in St.John Hospital, Bangalore, India.
2. Materials and Methods
- This study was undertaken for the detection of Cryptosporidium species, Isospora species and Cyclospora species among HIV/AIDS positive patients with diarrhoea who attended St. John Medical College and Hospital, Bangalore, India. The samples from 80 HIV positive cases with diarrhoea were collected from December 2011 to January 2013. These patients had already been tested for HIV at an ICTC centre as per strategy 3 of the National AIDS Control Organisation to establish the diagnosis of HIV. Stool examination: Stool specimen were collected after taking an oral consent from the patients according to the standard procedure of the WHO and they were examined microscopically by following the direct and the formalin-ether concentration method. The stool samples were collected in labelled, leak proof, clean and sterile plastic container and they were then transported to the laboratory within 3 hours of their collection. All specimens were collected prior to radiological studies using barium or the administration of bismuth, minerals oil and anti-diarrhoeal medication that could interfere with the detection and identification of intestinal parasites. The faecal specimens were properly labelled with the patient name, hospital number, date and the time of collection. The stool specimens were not kept at room temperature for longer time. The specimen should never be incubated at 37°C or frozen at 0°C. These specimens can be kept in refrigerator at 4°C. An episode of diarrhoea was classified as acute if it lasted for less than a month and provided the patient is diarrhoea free in the preceding months. Episode was defined as chronic when chronic when diarrhoea lasted more than a month, or was intermitted and recurrent over a period of at least 2 months with diarrhoeal symptoms for at least half this time. Then the stool samples were examined through a direct observation in saline (0.85% NaCl). Lugol’s iodine was used for the demonstration of the intestinal nuclear structure of the parasites. The smears of the direct and the concentrated specimens were examined by modified acid fast and rapin saffranin method for C. parvum, I. belli and Cyclospora.
3. Results
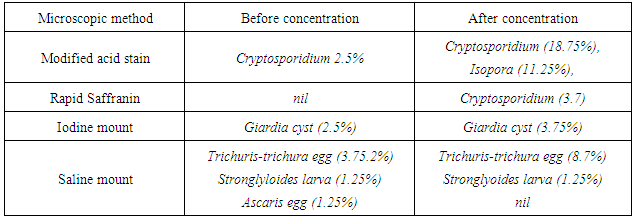
- The present study showed that out of 80 AIDS diarrhoeal stool sample, the prevalence of Cryptosporidium species (21.2%) oocyst was the commonest parasite, followed by Isospora species oocyst (11.2%). Other intestinal parasite found were Tricuris trichura egg (12.5%), Giardia cyst (6.2%) and Strongyloides larva (2.5%).
|
|
4. Discussion
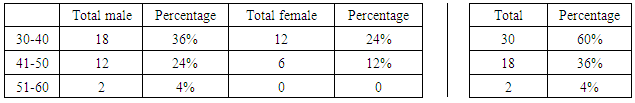
- In the present study, there is a male predominance as similar in studies conducted by S.V. Kulkari, S. Gupta as well in other studies [8, 9]. Weight loss (70%), fever (48%) was the most common complained. In the similar studies done by S.V Kulkarani & A. Singh also reported the same whereas in studies done by S. Satheesh, vomiting & abdominal pain was predominant complaint [8]. Most of the symptomatic cases presented with chronic diarrhoea, which is similar to the study by S. Satheesh [10]. However cases presented with acute diarrhoea in the study conducted by S.Gupta and S.S Rao Ajjampur [7].In our study, Cryptosporidium (18.7%) and Isospora (11.25%) were detected. No Cyclospora was detected in the present study similar with some other studies done by S.Satheesh et al & SS Rao [8, 7]. However, in the study conducted by Kumar et al & S.V Kulkarni et al, they detected Cyclospora. [11].Out of the 80 stool samples, 2.5% of Cryptosporidium oocyst was detected before concentration and 18.7% after concentration and staining by modified acid fast. Isospora oocyst (11.25%) was detected only after concentration followed by modified acid fast stain. Using rapid saffranin method, 3 (3.7%) of the above Cryptosporidium oocyst was detected. This result has agreements with other similar studies done by S.H Talib, S.Gupta where most of the organism yields better results in Modified acid fast stain. Modified acid fast stain may a better method to detect Cryptosporidium compared to rapid saffranin method. Stool concentration evidently improves detection of Cryptosporidium species and Isospora species as evidenced by other studies [13, 9].Other intestinal parasites present in this study were Giardia, Trichuris trichura, Strongyloides larva and Ascaris egg. Ascaris egg was identified before concentration. In other studies, they have reported Giardia, Ascaris lumbricoides, E. histolytica. [13, 14]. Trichuris trichura egg was also detected in one Cryptosporidium species positive stool sample.The study was limited as only single stool samples were examined and lack of molecular method which could increase the detection of coccidian parasites more, also larger number of samples need to be studied to determine if this observation is true.
5. Conclusions
- Cryptosporidium species and Isospora species are associated in AIDS patients. The oocysts can be detected using modified acid fast and rapid saffranin method. Stool concentration enhances detection of Cryptosporidium and Isospora oocysts. Detection of Cryptosporidium and Isospora species will help in proper management of patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML