-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Basic Sciences of Medicine
p-ISSN: 2167-7344 e-ISSN: 2167-7352
2022; 11(1): 1-4
doi:10.5923/j.medicine.20221101.01
Received: Jul. 5, 2022; Accepted: Jul. 18, 2022; Published: Jul. 20, 2022

Study of Thyroidea Ima Artery: Narrative Review of Its Prevalence and Clinical Significance
Rajani Singh
Department of Anatomy, UP University of Medical Sciences, Saifai, Etawah, India
Correspondence to: Rajani Singh, Department of Anatomy, UP University of Medical Sciences, Saifai, Etawah, India.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Thyroidea ima artery shows variability in origin and course with infrequent occurrence. Most frequently it originates from the brachiocephalic, followed by the aortic arch, common carotid, internal thoracic, inferior thyroid, transverse scapular, and suprascapular arteries. Clinically Thyroidea ima artery is very important for vascular surgeons. Hence the study was carried out. Aim of the study is to describe incidence, origin, course and clinical significance of this artery. Literature was explored using various databases. Only English language articles were selected for the study. Various terms related to thyroid ima artery were used for searching the literature. The detailed knowledge of origin and course of this artery is very essential to clinicians and vascular surgeons as it may be injured during surgery in the superior mediastinum or lower neck as in a low tracheostomy as during these procedures the artery may be damaged causing fatal haemorrhage. Its presence may be misinterpreted in neck angiography.
Keywords: Thyroidea ima artery, Arch of aorta, Neck, Superior mediastinum
Cite this paper: Rajani Singh, Study of Thyroidea Ima Artery: Narrative Review of Its Prevalence and Clinical Significance, Basic Sciences of Medicine , Vol. 11 No. 1, 2022, pp. 1-4. doi: 10.5923/j.medicine.20221101.01.
1. Introduction
- Thyroid gland consists of right and left lobes connected by isthmus. Mostly these lobes including isthmus are irrigated by superior and inferior thyroid arteries (Figure 1), originating from the external carotid artery and thyrocervical trunk, respectively [1]. During head and neck surgeries such as hemi-/total thyroidectomies and parathyroidectomies, these arteries serve as landmarks for recurrent laryngeal nerve (Figure 1), hence their recognition is very important [2]. Moreover, these arteries are ligated during aforementioned procedures to ameliorate patient outcome [3]. Existence of additional third artery, Thyroidea ima artery may creat complications due to its unforeseeable origin, course, morphology and rarity [4,5].
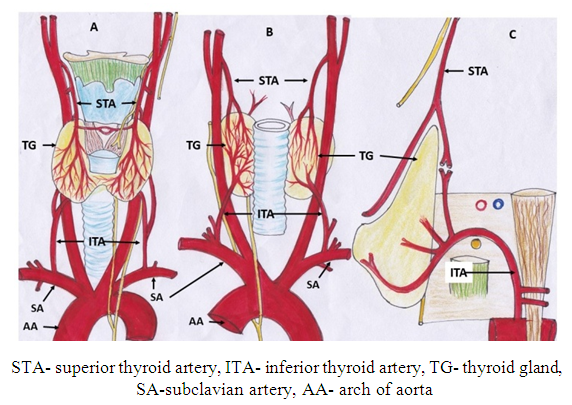 | Figure 1. Showing normal arterial supply of thyroid gland (A) anterior view (B) posterior view (C) Lateral view |
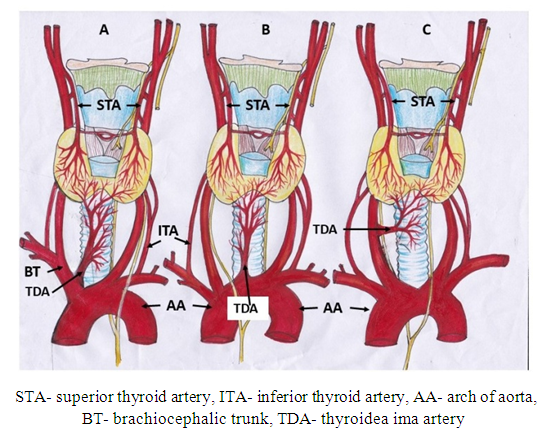 | Figure 2. Showing most common variant origin of thyroidea ima artery from (A) Brachiocephalic trunk (B) Arch of aorta (C) Right common carotid artery |
2. Material and Methods
- Literature was explored using different data bases like scielo, pubmed, medline, wilyonline library, medline, google scholar and terms such as thyroidea ima artery, prevalence of thyroroidea ima artery, variations of thyroidea ima artery, significance of thyroidea ima artery etc, related to thyroidea ima artery and its clinical significance were used during literature survey. Thyroidea ima artery in literature is not differentiated from accessory thyroid artery irrigating lobes of thyroid gland. In this study we classify this artery into two groups: I- Accessory thyroid artery supplying thyroid gland, II- thyroidea ima artery supplying isthmus of thyroid gland and other viscera of neck. English language articles and standard text books of Anatomy were selected for this study.
3. Results and Discussion
- Thyroidea ima artery has diverse variation of origin such as arch of aorta, brachiocephalic trunk, common carotid arteries etc. The artery ascends anterior to trachea and traverses the superior mediastinum and neck to reach the thyroid [10]. Review of literature shows marked degree of variability in the frequency, site of origin and the size of thyroidea ima artery. The commonest site of origin of the thyroid ima artery is from the brachiocephalic trunk in 1.9 to 6% cases followed by right common carotid artery [8] in 1.4% to 1.7% and from the arch of aorta on left side [11] in 0.36%. Bilateral thyroidea ima arteries have been reported by Gruber. Incidence of occurrence of this artery has been reported ranging between 4%-10% in reference book describing anatomic variations [9]. But Adachi detected in only 0.4% of the population [12]. Some investigators have described its frequency [13] as 6% or ranging [14] from 1.5% to 12.2%. The calibre of thyroid ima artery may be as large as the inferior thyroid artery or merely a minor branch. Thyroidea ima artery has mean diameter of 3-5 mm.Clinical Significance related to thyroidea ima artery: If this artery originating from high pressure large artery like arch of aorta, brachiocephalic trunk or common carotid artery, is injured, there may be fatal hemorrage if immediately hemostatis is not carried out [15]. This can be avoided if surgeon is aware of variant origin and course of Thyroidea ima artery. Moreover, if this artery is torned, its caudal separated part may retract into the superior mediastinum causing collection of blood clots in the thoracic cavity which are difficult to remove [16,17]. The artery is closely related to trachea, it may be damaged during cricoidectomies and tracheostomies [18,19]. Prompt hemostatis and vascular repair can improve the outcome of patient [20] which is possible only if surgeon is aware of variations in origin and course of thyroidea ima artery.Abnormal ramification of artery can cause intraoperative bleeding and /or post operative hematoma by damaging the thyroid ima artery [21].Thus, knowledge of the course of the thyroid ima artery is important for surgeons while performing neck surgeries or during tracheostomy procedures [22]. The knowledge of this artery is necessary in angiography done as a preoperative requisite in the thyroid and parathyroid surgeries, which could be missed if this artery is not selectively injected. Though the Thyoidea Ima artery, if present, is identifiable on radiological studies, its iatrogenic damage associated with emergent or surgical procedures can have acute and long-term complications [23] if unaware of variant course of the artery. With its course and relation to the thyroid, the information about Thyroidea ima artery is an important for various medical specialties, such as emergency medicine, endocrinology, otolaryngology, and radiology [18,23]. Occasionally thymic branches from thyroidea ima artery to supply thymus gland and oesophageal branches to supply cervical part of the esophagus [13]. The thyroidea ima is also reported to irrigate the inferior part of the thyroid gland [24], the isthmus [25], or the gland in general [26]. If thyroidea ima artery is only source of supply to thymus and oesophagus then damage to this artery may cause ischemia to these organs causing helm of complication if unaware of this variation related to thyroidea ima artery.Three cases have been reported in literature; in one case the thyroidea ima artery was the only arterial supply to thyroid and parathyroid glands, and in two instances it was part of a dual arterial supply. If Thyroidea Ima artery is only supply to thyroid and parathyroid glands and if it is damaged inadvertently in absence of knowledge of variant origin and course of this artery, it may cause preoperative fatal haemorrhage and postoperative thyroid and parathyroid related diseases. It can also supply enlarged parathyroid glands, as illustrated in three cases. During treatment of enlarged parathyroid glands, again the artery may be damaged if unknown of this variation. If thyroidea ima artery originates from large vessel specially arch of aorta, a high pressure vessel, high pressure will be generated in thyroidea ima artery making it prone for aneurysm and dissection. Moreover, hemodynamic changes and high endothelial shear stress/pressure will modulate endothelial gene expression through complex mechanotransduction processes, leading to the formation of early atherosclerotic plaques [27,28] in thyroidea ima artery. This is because the levels of endothelial vasoactive agents such as nitric oxide synthase, endothelin-1, and angiotensin-converting enzyme are significantly increased due to alteration in endothelial shear stress and hemodynamics [29]. These factors promote the deposition of atherosclerosis in thyroidea ima artery. This is life threatening when the artery is only supply to thyroid, parathyroid, thymus, trachea or oesophagus. Carotid artery stent is very common now a days. Thyroidea ima artery if originating from carotid artery may be injured if endovascular interventionist is unaware of this variant origin leading to complications during the procedure [30].The presence of thyroidea ima artery should be confirmed if routine arteriography is negative, especially if the inferior thyroid arteries are small or absent, or if a portion of the expected thyroid stain is missing [31] or the thyroid gland may suffer from ischemia if this artery is injured during neck surgery.
4. Conclusions
- Due to high variability in origin and course of thyroidea ima artery, it may be damaged in neck surgeries, tracheostomy procedures, endovascular interventions causing intraoperative and postoperative haemorrhage. In addition to this it may be misinterpreted in neck angiography. Thus, detailed knowledge of this artery is of paramount importance to neck surgeons, endocrinologists, otolaryngologists, diagnostic radiologists, endovascular interventionists, vascular surgeons and anatomists.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML