-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Basic Sciences of Medicine
p-ISSN: 2167-7344 e-ISSN: 2167-7352
2020; 9(3): 39-43
doi:10.5923/j.medicine.20200903.01
Received: Oct. 11, 2020; Accepted: Nov. 9, 2020; Published: Nov. 28, 2020

Trigeminal Neuralgia- Review of Literature
Rajani Singh
Department of Anatomy, UPUMS Saifai Etawah, India
Correspondence to: Rajani Singh, Department of Anatomy, UPUMS Saifai Etawah, India.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Trigeminal Neuralgia is a syndrome consisting of excruciating and lancinating facial pain. It is dreaded diseases and cripples a person so much that it is given a name “suicide disease.” This condition may lead to anxiety and depression in patients due to apprehension. Literature search has been carried out between September-December 2019 using various data bases and terms related to trigeminal neuralgia in the Department of Anatomy UPUMS Saifai Etawah India. It is said that focal demyelination at the trigeminal root entry zone is the underlying cause of this condition. According to many authors vascular compression of the nerve root causes this demyelination in most patients. To alleviate severe pain associated with this disorder, non-steroidal anti-inflammatory agents, narcotics or oral steroids may be administered. In refractory cases surgical manipulations like microvascular decompression of the trigeminal nerve or Gamma knife therapy may ameliorate symptoms. Considering severity of the condition and its immense clinical implications, review has been carried out to consolidate and update the existing knowledge and to elucidate common pitfalls in management of this disorder.
Keywords: Trigeminal neuralgia, Demyelination, Vascular compression
Cite this paper: Rajani Singh, Trigeminal Neuralgia- Review of Literature, Basic Sciences of Medicine , Vol. 9 No. 3, 2020, pp. 39-43. doi: 10.5923/j.medicine.20200903.01.
Article Outline
1. Introduction
- Trigeminal Neuralgia (TN) also known as tic doloureux is an important illness. Its significance increases as it cripples a person so much and causes suffering to such an extent that it is sometimes referred to as the “suicide disease.” It is one of the most painful conditions and can result in depression. Incidence of TN is approximately 4.5 cases per 100,000. Its frequency increases with advancing age and is more prevalent in women than in men in the ratio of 2:1 [1]. The TN can be treated effectively with medications but in refractory cases, invasive procedures are adopted. Here, a review of its history, clinical complications, causatives and common pitfalls in the diagnosis and management of TN has been performed. Considering the severity of diseases, updating and consolidating the related knowledge is essential. Therefore review study has been carried out. The study will be of paramount importance to neurologists and neurosurgeons in diagnosis and treatment of this neurological disorder.
2. Material and Methods
- Literature was explored in the department of Anatomy, UPUMS saifai during September 2019- Dec. 2019 using the following data bases: Medline, pubmed, Willy online library, research Gate, Scielo, Scopmed, Web of Science and Amed. Papers containing original data were selected and secondary references retrieved from bibliographies.Only English language articles and selected reference text books were taken into account for search. Terms used for literature search were as appended below: anatomy of trigeminal nerve, trigeminal neuralgia, trigeminal neuralgia and its clinical significance.
3. Clinical Features
- Trigeminal neuralgia is of two main types: typical and atypical trigeminal neuralgia. Both forms may occur in the same person.It was John Fothergill who firstly elucidated trigeminal neuralgia in 1773 and presented his work entitled “On a Painful Affliction of the Face.” in the Medical Society of London [2,3] and these patients of John Fothergill with trigeminal neuralgia were treated surgically by John Murray Carnochan. Both these stalwarts were graduates of the University of Edinburgh Medical School [4]. Fothergill described trigeminal neuralgia in 14 patients. According to him pain of trigeminal neuralgia was sudden, sharp, excruciating, of short duration and triggered by light touch or eating. Some authors report the pain of trigeminal neuralgia as electric, lancinating with an abrupt onset and termination, remaining for few seconds and can be so intense that the patient often winces in a tic-like fashion [4]. The pain of trigeminal neuralgia is confined to the area of distribution of the trigeminal nerve. Cutaneous stimuli within specific“trigger zones” may induce pain. Pain is so severe that patients unable to chew, drink, shave or brush their teeth. Rarely the site of pain is remote to the site of stimulation. Some patients will have a brief refractory period following an attack, during which subsequent cutaneous stimuli will not trigger an episode [5]. So, some patients may invoke an attack so that they can carry out essential activities like brushing the teeth, shaving etc.Sometimes, cross-modal stimuli such as a bright light or loud noise elicit an attack. Occasionally the pain starts spontaneously without any stimulation. It disturbs the lifestyle as tasks like eating, shaving and brushing may set off the pain of TN. The pain may be exasperated by wind, chewing and talking. The pain occurs in cycles with remissions lasting months or even years [6].Pain of TN varies during day and may be aggravated in morning which may be due to waning effect of medicine or increased facial stimulation associated with increased morning activities. Pain attacks are characteristically absent during sleep. Pain usually occurs in spells and may remain for weeks to months. Pain of TN is so severe and disabling that during the period of remission the patient is worried as to when the patient will get the next attack and how severe it will be and may lead to depression and anxiety [7,8]. Between attacks, there is often anxiety regarding the subsequent attack [7]. During attack free period, there is no symptom except hypoesthesia [7]. Both sides of face are reported to be affected in 1-6% cases. But both sides of face are less likely to be affected at the same time [6]. If both sides of face are involved at the same time it suggests that pathology lies in both trigeminal nerves since each side of face is innervated by only one trigeminal nerve. Pain attacks may increase in frequency and severity with passage of time. Slowly other branches of TN may be afflicted.If both sides of face are involved or other cranial nerves are affected simultaneously like V and VII nerve or V and IX nerve, it suggest systemic cause which may include multiple sclerosis or spanning cranial tumors [8]. Above mentioned features are suggestive of Type I TN. There is another type of TN in some patients described as A typical trigeminal neuralgia which is briefed below.
4. Atypical Trigeminal Neuralgia
- The atypical form of the disorder known as Trigeminal Neuralgia Type 2 (TN-2), is characterized by a constant aching, burning and stabbing pain of somewhat lower intensity when compared to Type 1. Pain of this type of TN is constant in 50% of patients whereas that of Type I is sharp and fleeting in nature. Both forms of pain may occur in the same person, sometimes at the same time [9].TN-2 is supposed to be caused by a compression affecting delayed pain carrying nerve fibers rather fast pain fibers or have long-term, chronic injury anywhere along the nerve’s course [9].
5. Anatomy of Trigeminal Nerve
- The trigeminal nerve is a paired Vth cranial nerve which emerges on the anterior surface of the pons (Fig. 1). The trigeminal nerve arises from one motor nucleus and three sensory nuclei in the brainstem. It consists of sensory and motor roots. The roots pass anteriorly through the prepontine cistern and Meckel’s cave to the trigeminal ganglion in the middle fossa. The three branches, the ophthalmic nerve (V1), the maxillary nerve (V2), and the mandibular nerve (V3) emanate from the trigeminal ganglion [Fig. 1].
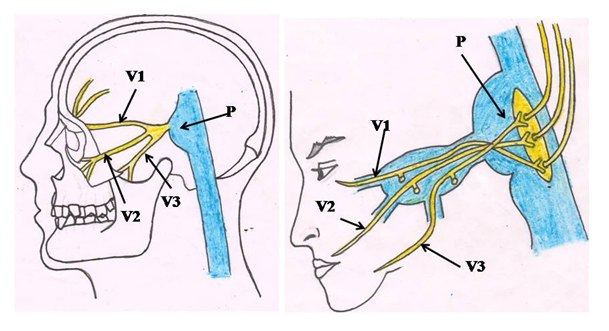 | Figure 1. Attachment of trigeminal nerve to pons and its three branches Ophthalmic (V1), Maxillary (V2) and Mandibular (V3) nerves. P= pons |
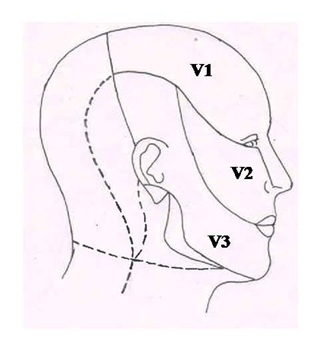 | Figure 2. Showing area of face innervated by three branches of trigeminal nerve, Ophthalmic (V1), Maxillary (V2) and Mandibular (V3) nerves |
6. Pathogenesis
- In 1829, Charles Bell studied the functions of the trigeminal and facial nerves and advocated that paroxysmal pain in trigeminal neuralgia is due to dysfunction of the trigeminal nerve [12].The etiology of TN is unclear but may be due to loss of myelin sheath surrounding the trigeminal nerve [13]. According to Hamlyn in 80-90% cases, TN is caused by compression of trigeminal nerve by overlying vessel [14]. Certain authors suggest demylination may be due to compression and throbbing effect of enlarged or an aberrant branch of superior cerebellar artery against the microvasculature of the trigeminal nerve as it exits from the pons [15]. Compression is caused by superior cerebellar artery in 75% and anterior inferior cerebellar artery in 10% cases of TN [16]. Besides, a vein is found to compress the nerve in about 68% of cases [10].Continuous compression of trigeminal nerve may damage the myelin sheath resulting in erratic, aberrant and hyperactive functioning of the nerve causing pain at the slightest stimulation in the area innervated by the nerve as after demyelination the pain signals do not stop after the stimulation is over. Mechanical displacement caused by compressing vessel generates aberrant impulses in demyelinated axons [17] and ectopic spontaneous nerve and abnormal nonsynapticephaptic impulses [18]. Demyelination may also be caused by aneurysm, by an arteriovenous malformation [19], by a tumor such as an arachnoid cyst or meningioma in the cerebellopontine angle [20] or by a traumatic event, multiple sclerosis and stroke. TN is observed in 3-4% of patients with multiple sclerosis [20]. A tumor may compress against the trigeminal nerve causing TN. This is a rare cause. Physical damage to the nerve may be due to injury like facial trauma, a dental or surgical procedure, or infection. There may be family history leading to TN.If peripheral compression of nerve occurs for brief period, it usually does not cause pain. Continuous compression culminates in local demyelination with no loss of axon potential continuity but subsequently may lead to axonal degeneration. According to some authors trigeminal neuralgia is caused by demyelination of axons in the Gasserian ganglion, the dorsal root or both [20]. Few authors believe that idiopathic trigeminal neuralgia is due to demyelination of trigeminal sensory fibers within the proximal nerve root [17].Since the fibers are arranged in multiple layers in Trigeminal nerve root , its medial compression may lead to V2 symptoms, lateral V3 symptoms and cranial compression V1 symptoms. Focal demyelination in Trigeminal nerve has been demonstrated histologically near vascular indentation in patients with TN due to vascular compression [21].
7. Diagnosis
- Trigeminal neuralgia is diagnosed based to symptoms typical of this disorder after excluding other causes of pain such as postherpetic neuralgia. Other factors such as age and sex should also be taken into consideration for it is observed more after the age of 50 years though no age is spared. Moreover women are more commonly affected than men. MRI scan may help eliminate other conditions with similar symptoms such as tooth decay, a tumor, or sinusitis. However, an MRI is unlikely to show the exact cause of nerve irritation.Trigeminal neuralgia patients should be adviced MRI to rule out tumour, other mass lesion, demylenation and stroke [22]. Refractory cases of TN may be advised advanced MRI and MR angiography to rule out Trigeminal nerve demyelination caused by compressing vessel [16].
8. Treatment
- Considering the severity of pain and disabling caused by TN, immediate relief of pain is very important.Nonsteroidal anti-inflammatory agents, narcotics or a short course of oral steroids may provide symptomatic relief. But in all cases, daily prophylactic therapy is recommended.Treatment of TN can be done by medications but in some cases surgery may be indicated.
9. Medical Treatment
- Carbamazepine is first-line of treatment and is effective in nearly 90% of cases [23]. Morning painful exacerbations can be prevented by advising extended release formulation at night. Gabapentin is second line treatment for trigeminal neuralgia with rare serious adverse effects [24]. Moreover it is neither metabolized nor bound to serum protein. So it can be used safely in the elderly patients [24].In a most recent study Oxcarbamazepine has shown equivalent efficacy to carbamazepine with lower incidence of adverse side effects [23]. Hence it can used to treat TN.In some patients, spontaneous remissions occur, so when the patients are asymptomatic weaning of medications can be considered. If symptoms recur doses should be increased to therapeutic level. But it is not always acceptable since some patients are anxious over next attack of pain [4].
10. Surgical Treatment
- In patients with intractable pain or intolerable side effects of medicines, invasive procedures may give relief. In 1967, Peter Jannetta was first to perform microvascular decompression of the nerve in patients with TN [25].A retrospective study of microvascular decompression of the nerve in patients with TN by Barker showed complete immediate postoperative relief in 82% of patients and partial in 16%. After one year 75% patients were asymptomatic while after 10 years 64% were pain free [10]. Major complications were rare but included death (0.2%), brainstem infarction (0.1%), severe facial numbness (1.6%), severe ipsilateral hearing loss (1.1%), and cerebrospinal fluid leak (1.5%). Intraoperative brainstem evoked responses can reduce the rate of complications [10].Less invasive percutaneous procedures for the treatment of trigeminal neuralgia include radiofrequency thermo coagulation, retro-gasserian glycerol injections and trigeminal ganglion balloon compression specially in elderly patients and those with comorbidities [26].All of these procedures permanently lesion the trigeminal ganglion and there is high incidences of facial numbness, dysesthesia and corneal keratitis. Observational studies suggest that thermocoagulation may provide greater pain relief but may cause permanent dysesthesia than glycerol rhizolysis [27]. However, glycerol rhizolysis is effective for 3 or more years and the procedure has to be repeated when symptoms recur [27].Stereotactic gamma knife radiosurgery is an non invasive, nondestructive therapy for treating the trigeminal root entry zone with a targeted beam of gamma radiation. It was introduced in 1951 by Lars Leksell to treat trigeminal neuralgia. Because of lack of high-quality neuroimaging for targeting, the procedure was not used for several years [28]. However due to advances in MR imaging and limitations of use of destructive treatments has lead to increased interest in this technology. In a study this technique causes dampening of pain in 94% of pateints with TN. In addition to this, Gamma knife radiosurgery cause very low rate of trigeminal dysfunction and more suitable for elderly patients or those with comorbid disease. Finally, repetitive transcranial magnetic stimulation of the contralateral motor cortex is ultra new therapy under consideration for the treatment of several pain disorders, including trigeminal neuralgia. The technique is still under trial. Further studies are recommended for best treatment regimen and long term tolerability of the procedure [29].The most modern technique to alleviate pain of TN is Pain Stimulator Placement. Here the surgeon places tiny electrodes underneath the skin at the site of the trigeminal nerve. Small impulses are used to disrupt the misfiring signals via these electrodes, preventing the nerve from sending false messages to the brain [9].
11. Conclusions
- Trigeminal neuralgia is one of the most painful and disabling condition. The pain is so severe that it is known as suicidal diseases. So proper management of this condition is very essential. In most of patients, cause of this diseases is vascular compression of trigeminal nerve. In majority of patients, pain is relieved by anticonvulsants. In refractory patients newer methods such as microvascular decompression, gamma knife therapy, and percutaneous treatments can alleviate the pain.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML