-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Basic Sciences of Medicine
p-ISSN: 2167-7344 e-ISSN: 2167-7352
2020; 9(2): 24-31
doi:10.5923/j.medicine.20200902.02
Received: Aug. 22, 2020; Accepted: Sep. 10, 2020; Published: Sep. 15, 2020

The Relation Between Spirometry Parameters and Tissue Doppler Echocardiography Findings in Children with Asthma
Sameh Abdel-Aziz Ahmed Mansour1, Abd ElMohsen Mostafa Abdou AbouAalia2, Fathi Khalil Hassen Nowar1, Sherif Mostafa Kamal Reda1, Hesham Ahmed Mohammed Ali1
1Department of Pediatrics, Faculty of Medicine, Al-Azhar University, Egypt
2Cardiology Department, Faculty of Medicine, Al-Azhar University, Egypt
Correspondence to: Abd ElMohsen Mostafa Abdou AbouAalia, Cardiology Department, Faculty of Medicine, Al-Azhar University, Egypt.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Despite advanced understanding of the asthma pathophysiology as it a complex immune-mediated multi-factorial disease, some of asthma systemic effects of are still not well defined. Objectives: To find out the relation between spirometry parameters and heart function assessed by tissue Doppler echocardiography in children with Asthma. Methods: One hundred and five child were enrolled in this study (35 Child with mild persistent asthma (13.66 ± 0.49 years), 35 child with intermittent asthma (13. 76 ± 0.39 years) and 35 child as a control (13.54 ± 0.36 years)). Spirometry parameters [forced vital capacity (FVC), forced expiratory volume in the first second of FVC (FEV1), the ratio between FVC1 and FVC (FVC1/FVC) and peak expiratory flow (PEF)] were done for all individuals. Echocardiography parameters were evaluated using conventional and tissue Doppler imaging (TDI). Results: In children there is significant difference of pulmonary function tests according to severity of disease. Echocardiography revealed no significant difference by conventional echo but there is difference in diastolic function of both ventricles and systolic functions of RV by TDI. There is some correlations between spirometry measurements and TDI parameters especially right ventricular diastolic dysfunction parameters ( in mild persistent asthma FVC1 is positively correlated with Tricuspid E` and negatively with E/E` and FVC is positive correlated with tricuspid A` and tricuspid S`, while FVC1/FVC positively correlated with tricuspid E`/A` and S`, while in Children with intermittent asthma maximal expiratory flow brought to 25-75% of the vital capacity (MEF 25-75%) is positively correlated with TDE (S`) & (E`) peak velocities of tricuspid valve and PEF is positively correlated with IVRT). We also found that a negative correlation between tricuspid E/E` and duration of illness while a positive correlation with mitral E/E` and duration of illness in asthmatic children. Conclusion: Changes in echocardiographic parameters, evaluated by TDI, were observed in mild and intermittent asthma patients even with normal conventional echocardiography and also asthma severity can be predicted using TDI.
Keywords: Spirometry Parameters, Asthma pathophysiology
Cite this paper: Sameh Abdel-Aziz Ahmed Mansour, Abd ElMohsen Mostafa Abdou AbouAalia, Fathi Khalil Hassen Nowar, Sherif Mostafa Kamal Reda, Hesham Ahmed Mohammed Ali, The Relation Between Spirometry Parameters and Tissue Doppler Echocardiography Findings in Children with Asthma, Basic Sciences of Medicine , Vol. 9 No. 2, 2020, pp. 24-31. doi: 10.5923/j.medicine.20200902.02.
Article Outline
1. Introduction
- Asthma is a common chronic disease of respiratory system affecting up to 18% of population. There is a complex interaction between respiratory diseases and cardiovascular function. In asthma there were attacks of recurrent hypoxemia, and hypercarbia that with various released mediators and cytokines lead to pulmonary vasoconstriction and development of pulmonary hypertension [1].Pulmonary hypertension developed due to multiple factors beside pulmonary vasoconstriction, including the distortion of pulmonary vessels by parenchymal changes, increased cardiac output, and blood viscosity from polycythemia secondary to hypoxia. Asthmatic patient develop pulmonary hypertension as a sequale of chronic inflammation and recurrent hypoxia. Severe asthma can lead to cor pulmonale later in life [2].Cor pulmonale starts with RV diastolic dysfunction of the right ventricle that depends on RV hypertrophy and total pulmonary resistanc[3]. The interaction between both ventricles with increased LV afterload can lead also to LV) diastolic dysfunction [4].Tissue Doppler imaging (TDI) by echocardiography through its quantitative measurement of regional myocardial velocities can detect subclinical RV abnormalities when conventional echocardiography fail [5]. The relation between spirometry parameters reflecting severity of asthma and TDI is not well understood.
2. Aim of the Work
- To find out the relation between spirometry parameters and heart function assessed by tissue Doppler echocardiography in children with Asthma.
3. Patients and Methods
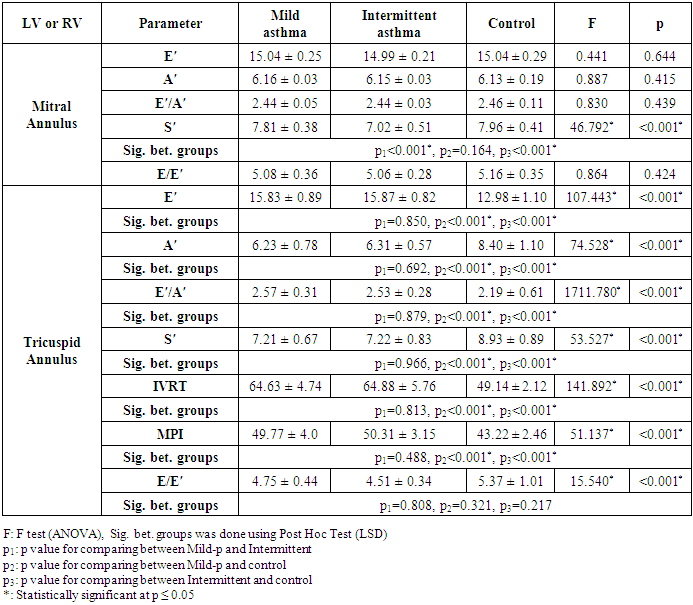
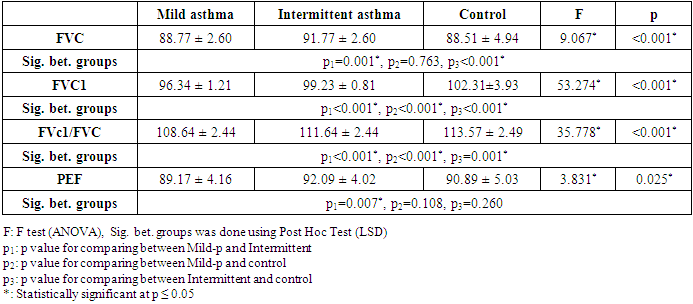
- Study population:This is a Cross sectional study carried out on 105 child (35 of them with mild persistent asthma, 35 with intermittent asthma according to Global Initiative for Asthma (GINA) report 2006 in remission for at least 4 weeks and 35 matched healthy children) on regular follow up at the Pediatric Allergy & Pulmonology Outpatient Clinics, Al-Azhar university Hospitals (Al-Hussien & Bab EL-Shairia) during the period from January 2013- May 2015. The patients were excluded if moderate or severe persistent asthma, other co-morbid diseases (upper or lower respiratory infection, allergic rhinitis, gastroesophageal reflux, obesity; chronic cardiovascular disease or renal impairment), acute attack of asthma during the last 4 weeks and use of oral steroids in the last 4 weeks or refusal of parents of patients to participate in the study.Methods The following was done For all subjects:1. Informed written consent from the parents or persons responsible for the children to participate in the study.2. Detailed history was taken from parents especially of pulmonary symptoms and family history of allergy.3. Thorough physical examination were performed including the height, body weight, body mass index, heart rate, respiratory rate, and blood pressure for all children. 4. Routine laboratory investigations including CBC, CRP & ESR.5. Plain chest X- Ray.6. Pulmonary function tests using spirometry [forced vital capacity (FVC), forced expiratory volume in the first second of FVC (FEV1), the ratio of FEV1 to FVC, and peak expiratory flow (PEF)]. For each patient three technically acceptable measurements were performed and the highest value was taken [6].7. 12 lead electrocardiogram was done for each patient.8. ECG-gated transthoracic echocardiography was done by Single experienced observer who was blinded to the patient’s respiratory status using Philips iE33 echo machine with S5-1 probe (in adult echo unit, Cardiology department). The patients were studied without sedation while they were lying quietly in the supine and left lateral decubitus positions. According to standard techniques by the American Society of Echocardiography the standard views (parasternal long and short axises, apical 4 chamber, 2 chamber and 3 chambers and subcostal views) and modes (2D, M-mode, pulsed wave, continuous wave, color Doppler and TDI) were obtained [7].The following measurements were taken:1) LV End-diastolic and end-systolic dimensions, RV anterior wall thickness, and end-diastolic dimension [7].2) Trans-mitral and tricuspid pulse-wave peak velocities during early diastole (E), peak velocity during late diastole (A) and deceleration time (DT) of the early diastolic velocity.3) Tissue Doppler imaging (TDI) of peak systolic (S′) and early (E′) and late diastolic velocities and from the apical four-chamber view. Sample volume was placed in apical 4 chamber view at the lateral tricuspid annulus and the average medial and lateral mitral annulus. The ratio of early to late diastolic annular velocities was calculated. Cardiac time intervals, comprising right ventricle including isovolumetric contraction and relaxation time (IVCT), (IVRT), and ejection time (ET) from the beginning to the end of the pulmonary flow, was measured. Doppler-derived myocardial performance index (MPI) was calculated as the IVCT and IVRT divided by the ejection time (ET) [7].Statistical analysis:Data were collected and analyzed using IBM SPSS software package version 22.0 (IBM corporation and others, USA). Qualitative data were described using number and percent. Quantitative data were described using range (minimum and maximum), mean± standard deviation and median. Significance of the obtained results was judged at the 5% level. The used tests were: Chi-square for categorical variables (to compare between different groups), Fisher’s Exact or Monte Carlo correction when more than 20% of the cells have expected count less than 5, F-test (ANOVA) For normally quantitative variables, to compare between more than two studied groups, and Post Hoc test (LSD) for pair wise comparisons, Mann Whitney test for abnormally quantitative variables, to compare between two studied groups, Kruskal Wallis test for abnormally quantitative variables, to compare between more than two studied groups and Pearson coefficient to correlate between two normally quantitative variables.
4. Results
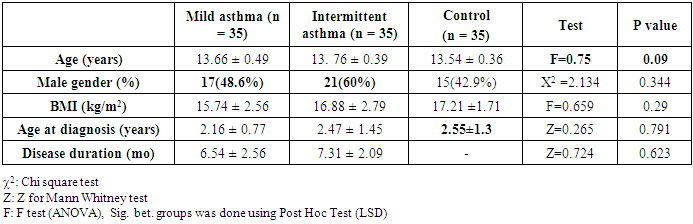
- This case control study was designed to assess the left and right ventricular function in children with bronchial asthma and to detect the correlation between spirometry parameters and tissue Doppler echocardiography. Both asthmatic cases and controls were properly matched regarding age, sex, BMI, age at diagnosis and bronchial asthma disease duration., birth order, family size, parental education and parental occupation. The differences between the two asthma groups (mild and intermittent) and control were statistically insignificant (P >0.05). (Table 1).
|
|
|
|
|
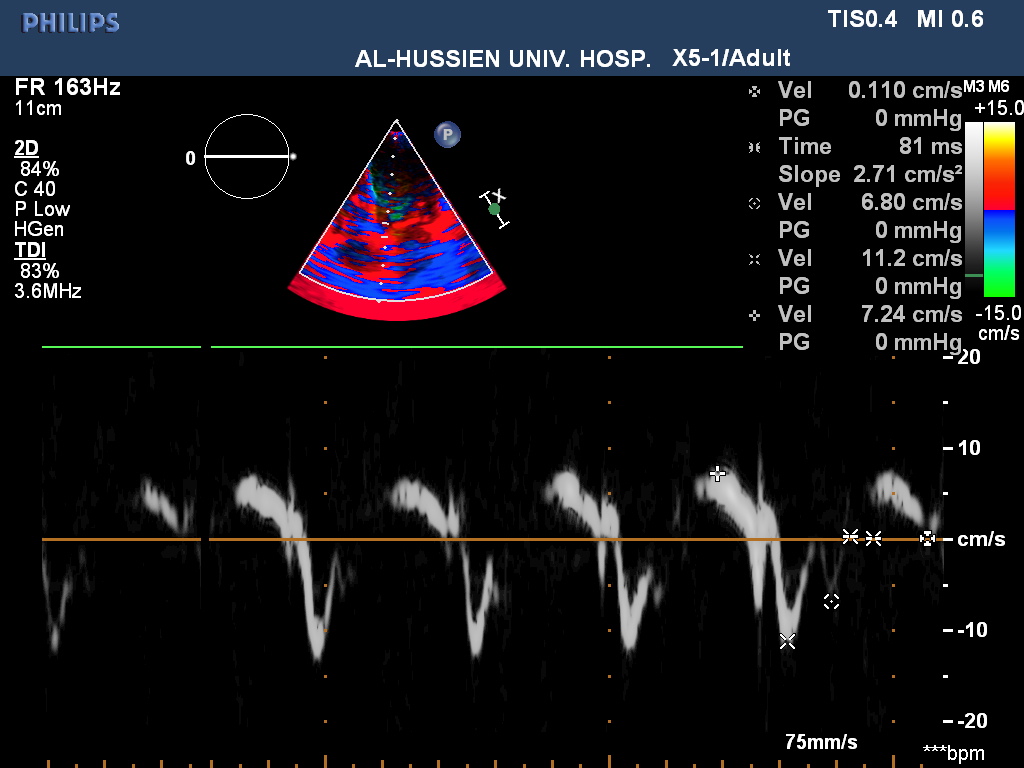 | Figure (1). TDI mitral valve septal annulus (Em: 11.2 cm/sec), Am (6.5cm/sec), Sm (7.2cm/sec), E/E'(7.7) Normal tissue Doppler image parameters. Patient No. (19) with mild asthma |
|
5. Discussion
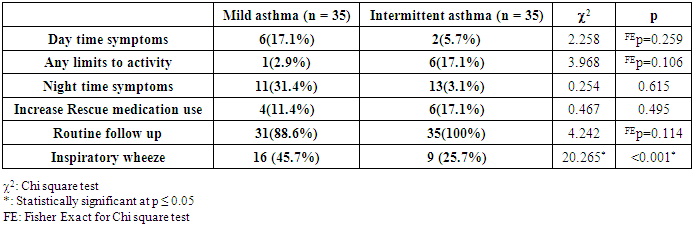
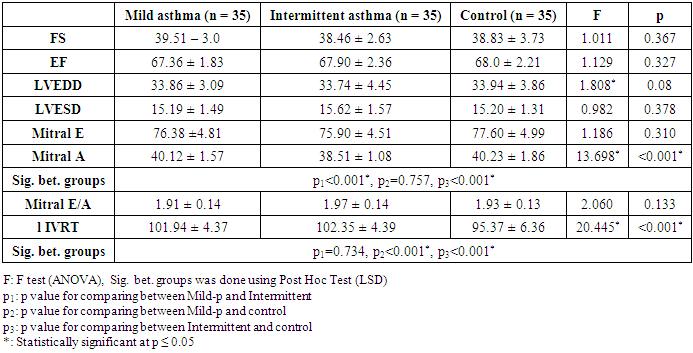
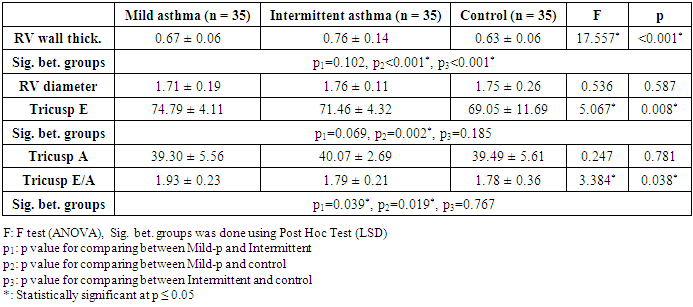
- Asthma is a complex immune-mediated multifactorial disease in which there are recurrent episodes of airway narrowing, resulting in difficulty breathing and coughing, and in which the airway narrowing is variable. Sustained pulmonary vasoconstriction and narrowing of the pulmonary vasculature which may develop pulmonary hypertension in asthmatic patients is believed to result from recurrent exposure to hypoxemia besides chronic and sustained inflammation in the airway of those patients which lead to right heart enlargement with ventricular hypertrophy, and impaired cardiac function, known as cor pulmonale [2].Little is known about the function of the right ventricle early in the disease. Spirometry is the easiest and most commonly performed measurement of lung function. It uses forced ventilatory manoeuvres to assess maximal flow rates and dynamic lung volumes.As the patient performs forced inspiratory and expiratory manoeuvres through the mouthpiece of the spirometer, flow rates and time are measured. Volumes are calculated from these parameters. Older school children and adolescents may be able to perform satisfactory flow–volume loops on most electronic spirometers.Chronic chest disease resulted in early RV diastolic dysfunction followed by LV diastolic dysfunction from interplay between ventricles. The degree of RV diastolic dysfunction is proposed to depend on RV hypertrophy and total pulmonary resistance. TDI enables the detection of right ventricular dysfunction in the early stages of respiratory disease [3].In this study both groups (Asthmatic children and controls) were properly matched together regarding age, sex and socioeconomic standard. Regarding demographic data 55% of asthmatic children were males and rest of them are females these agree with Elmasry, et al. [8] who reported that bronchial asthma is more common in male compared to female patients.In the present study it was found that all the left ventricular dimensions and functions by conventional echocardiography among asthmatic children were insignificantly differ from controls.A study done in by Elmasry et al. [8] to assess the left ventricular function among asthmatic children both during and after resolution of acute severe asthma found that patients had significant higher trans-mitral peak A velocity and lower E/A ratio (i.e. impaired LV diastolic function) during acute asthma exacerbation but disappeared after its resolution and concluded that trans-mitral inflow velocity patterns during acute severe asthma in children are suggestive of altered LV preload due to an acute transient elevation in pulmonary artery pressure secondary to the altered lung mechanics and not reflection of intrinsic LV diastolic dysfunction.In the current study, significant differences between groups were found regarding E' and A' evaluated in the tricuspid and mitral annuli. In addition, the MPI of the right ventricle was significantly higher in the group with intermittent asthma. Interestingly, symptoms and signs of respiratory stress were similar in both groups. Taken together, these findings suggest that echocardiographic parameters, especially TDI parameters, can be useful as a complementary evaluation for patients with asthma, allowing the early detection of repercussions on the heart. The relation and interaction between lung and cardiovascular function is complex (cardio-pulmonary axis). Right ventricular hypertrophy was present in asthmatic patients as Shedeed et al. [3], Ozdemir et al. [2], Han et al. [9] and Zedan et al. [10], but not De-Paula et al. [11], that found no RV hypertrophy unlike these studies but De-Paula studied only 20 asthmatic patients. Right ventricular hypertrophy begins very early in the course of the disease, they explained this process as The RV is a thin-walled, compliant, low pressure chamber that pumps the same stroke volume as the left ventricle (LV) with 25% of the stroke work because of the normally low resistance of the pulmonary vasculature [3].Moreover, in the current study the conventional Doppler echocardiogram revealed statistically significant difference between the controls and the group with asthma regarding peak velocities during the early diastole and atrial contraction (E, A and E/A) evaluated in the annulus of the tricuspid valves and only A wave when evaluated at the mitral valve. This finding agree with De-Paula et al. [11], and Zeybek et al. [5] who found that tricuspid E velocity, E/A ratio and isovolumetric relaxation time (IVRT) were significantly different in mild asthmatics and control subjects compared to those among moderate and severe cases. In contrary, Shedeed et al. [3] found no significant differences in these variables among controls and a group with asthma or in between the different degrees of asthma severity.A number of studies have demonstrated that patients with asthma exhibit diastolic dysfunction [3], [5], [10]. Indeed, in this study significant differences between both asthma groups and the control group regarding myocardial diastolic velocities E', A' and E'/A' ratio evaluated in the tricuspid annulus. Similar finding were appear in the mitral valve annulus, with myocardial velocity reduction in early diastole and an increase in atrial contraction. A significant increase in IVRT was also found in the two groups of asthma, resulting in significant increase in the MPI. Myocarial Performance Index (MPI) is a simple and useful clinical index of global ventricular function, and it is reported to be independent of heart rate and ventricular geometry. For this reason, MPI is used to evaluate the cardiac effects of multiple systemic diseases. In patients with chronic obstructive lung diseases, the longer IVRT and MPI of the right ventricle the subclinical RV dysfunction [12].Vitarelli et al. [13] stated that the parameters of TDI-determined RV dysfunction were complementary to indices of conventional echocardiography and were correlated with respiratory function tests in patients with chronic obstructive pulmonary disease. In these patients, subclinical pulmonary hypertensionand chronic inflammatory mediators lead to RV dysfunction and TDI was found to be useful in showing RV functions.The TDE parameters of children included in the study were all normal according to patient age. However, a significant difference of TDI parameters in asthmatic patients may support the presence of subclinical RV dysfunction. Regarding the selected paramters of spirometry ( FEV1, FEV1/FVC, and PEF), are the best predictors of disease severity in children with asthma [14]. In previous studies, different correlations were reported between respiratory function tests and TDE findings in asthmatic children like Zeybek et al. [5]. In the current study, we found that in children with mild persistentasthmaFVC1 is positively correlated with Tricuspid E` and negatively with E/E` and FVC is positive correlated with tricuspid A` and tricuspid S` in mild persistent asthma while FVC1/FVC positively correlated with tricuspid E`/A` and S`.Children with intermittent asthma MEF 25-75% is positively correlated with TDI (S`) & (E`) of tricuspid valve.PEF is positively correlated with IVRT while Ozdemir et al. [2] stated that PEF was negatively correlatedWith the E`/A` myocardialdiastolic velocities of the tricuspid annulus.We also found that a negative correlation btween tricuspid E/E`and duration of illness while a positive correlation with mitral E/E` and duration of illness in asthmatic children.This means patients with bronchial asthma have right ventricular dysfunction and the severity of the functional impairment is parallel with the severity of the disease and right Ventricular subclinical diastolic dysfunction than left ventricle especially with long duration of illness.Massoud, et al. [15] stated that there is an evidence for the role of inflammation in patient with bronchial asthma particularly among severely asthmatics on myocardial functions where such patients have chronic and sustained inflammation, which increases at the time of an exacerbation of respiratory symptoms. Various mediators and cytokines are produced during the early and late phases, including interleukinssuch as IL-1 beta, IL-2, IL-6, IL-8, IL-10, as well as tumor necrosis factor-alpha (TNF-a). These mediators are potent depressants of cardiac contractility and long term exposure resulting in cumulative effect on cardiac function.This means that disease severity can be predicted using TDI. Identifying patients with increased risk of ventricular dysfunction may have important implications for treatment.
6. Conclusions
- Although the clinical and conventional echocardiographic findings of asthmatic children were apparently normal, tissue Doppler echocardiographic study revealed subclinical right ventricular dysfunction, which is positively correlated with the severity of asthma. This signify the diagnostic value of tissue Doppler imaging in the early detection and monitoring of such deleterious effects among asthmatic patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML