-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Basic Sciences of Medicine
p-ISSN: 2167-7344 e-ISSN: 2167-7352
2019; 8(2): 23-28
doi:10.5923/j.medicine.20190802.01

Antimicrobial Activity of Root Bark Extracts of Rhus natalensisa and Rhus ruspolii
Peter W. Njoroge, Sylvia A. Opiyo
Department of Physical and Biological Sciences, Murang’a University, Murang’a, Kenya
Correspondence to: Sylvia A. Opiyo, Department of Physical and Biological Sciences, Murang’a University, Murang’a, Kenya.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Bacteria and fungi are frequent causes of serious opportunistic infections worldwide. Several effective antibiotic drugs are in the market. However, drug-resistance, side effects and cost of such antibiotics limits their usefulness in disease management. About 80% of the world’s inhabitants still rely on traditional medicines based on herbal plants for their primary healthcare. Anti-infective agents from plant origin are preferred because they have no side effects and are readily available. Rhus species have several applications both in traditional and contemporary medicine yet scientific data to support such uses is scanty. The aim of this study was to determine the efficacy of Rhus natalensis Krauss and Rhus ruspolii Engl in management of microbial infections. Plant extracts were subjected to cytotoxicity, antibacterial and antifungal assays using standard methods. LC50 values n-hexane, dichloromethane, ethyl acetate and methanol extracts were 7.15, 13.35, 4.80, 16.70 and 42.53, 22.3, 19.70, 25.70 μg/ml for R. natalensis and R. ruspolii, respectively. The plant extracts showed moderate activities (P ≤ 0.05) against the tested bacteria (Gram-positive and Gram-negative) and fungi. In all the tests, bioactivities of the extracts were lower compared to activity of standard drugs which were used as controls. These findings support the use R. natalensis and R. ruspolii in treating bacterial and fungal infections. Further studies aimed at isolation and characterization of the bioactive principles is necessary with the hope of getting better antimicrobial agents. It is also necessary to determine the mechanism of action of the extracts.
Keywords: Rhus natalensis, Rhus ruspolii, Cytotoxicity, Antibacterial, Antifungal, LC50
Cite this paper: Peter W. Njoroge, Sylvia A. Opiyo, Antimicrobial Activity of Root Bark Extracts of Rhus natalensisa and Rhus ruspolii, Basic Sciences of Medicine , Vol. 8 No. 2, 2019, pp. 23-28. doi: 10.5923/j.medicine.20190802.01.
Article Outline
1. Introduction
- Bacteria and fungi are frequent causes of serious opportunistic infections [1]. This is more so with a wide range of hosts with weakened immunity such as cancer patients, premature infants and human immunodeficiency virus (HIV) victims [2]. Many opportunistic bacteria and fungi are resistant to the antibiotics currently available in the market [3]. Antimicrobial resistance has worsened in the last decade. The increase in the number of drug-resistance cannot be matched by parallel expansion in the anti-infective agents used to treat infections [4]. In addition, side effects and cost of antibiotics limits their usefulness in disease management [4]. About 80% of the world’s inhabitants still rely on traditional medicines based on herbal plants for their primary healthcare [5-7]. Previous studies have shown that in plants there are bioactive compounds that have gained increasing interest as potential therapeutic agents [8-10]. Anti-infective agents from plant origin are preferred since they have no side effects, have better patient tolerance and are relatively inexpensive [11,12].The genus Rhus (sumac) which belongs to the family Anacardiaceae, consists of approximately 250 species which occur mainly in the tropics, subtropics and temperate areas of the world, especially in North America and Africa [13]. In traditional medicine, extracts of Rhus species are used to manage several ailments including influenza, wounds, diarrhea, abdominal pain, indigestion [14], diabetes, malaria, rheumatism [15], aching gums, toothaches, swollen legs [16], dog bites, peptic ulcer, kidney stones, skin eruptions, bruises and boils [17]. Root extracts of R. natalensis are used to manage venereal diseases, heartburn, cold, cough, diarrhea [18], hernia and stomach ache [19], influenza, abdominal pain and gonorrhea [14]. The leaves are used treatment of syphilis [20], cough and colds [14].Previously studied showed that the species posses a wide range of bioactivities including antimicrobial [21,22], antiviral [14,23], inflammation [24], anticancer [25,26], antiplasmodial [27-29], and antioxidant [22,24,29,30-32]. Phytochemical studies revealed that the plants are rich in flavonoids [22,24,26,27,30], biflavonoids [28,33], anthocyanins, quinones [27], triterpenes [34], sterols, coumarin [35], and urushiol [22,33]. We report the cytotoxic, antibacterial and fungal activities of R. natalensis and R. ruspoli. This is the first report on biological activity of R. ruspoli.
2. Materials and Methods
2.1. Plant Material
- The root bark of R. natalensis and R. ruspolii were collected from Kapkonga, Iten, 40 km northeast of Eldoret Town in Kenya. The plant materials were identified and the voucher specimen, reference numbers PKT/R1 and PKT/R2 for R. natalensis and R. ruspolii respectively, were deposited at the National Museums of Kenya. The plant materials were dried under the shade at room temperature for one month then ground into coarse using a mill (Christy and Norris Ltd., Chelmsford, England).
2.2. Solvent Extraction
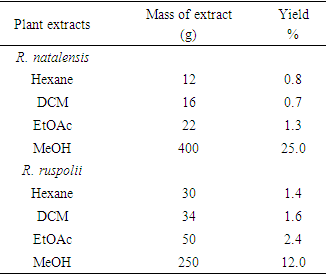
- Powdered root bark of Rhus natalensis (1.6 kg) and R. ruspolii (2.1 kg), were sequentially extracted using n-hexane, dichloromethane (DCM), ethyl acetate and methanol. The plant materials were soaked in cold solvent and left to stand for five days with occasional shaking. The macerates were filtered and concentrated at reduced pressure (temperature of 45°C) using rotary evaporator. The extracts (Table 1) were weighed and stored at 4°C in brown glass bottles.
|
2.3. Brine Shrimp Lethality Test
- Brine shrimp lethality bioassay is considered a useful tool for preliminary assessment of toxicity. The method is attractive, because it is simple, inexpensive and sensitive [36]. Brine shrimp eggs (Artemia salina) were hatched in artificial sea water prepared by dissolving sea salt (38 g/l) in distilled water. After incubation for 48 h at room temperature, the brine shrimp nauplii were attracted to one side of the vessel with a light source and collected using a pipette. The larvae were separated from eggs and placed in small beakers containing sea water [37]. Each crude extract (10 mg) was dissolved in dimethyl sulphoxide (DMSO, 50µl) and then diluted with 9.95 ml of sea water. Test solutions (100 µl) of varying concentrations (0.78 - 200 µg/ml) were obtained by the serial dilution using simulated seawater in 96-well microplates. DMSO (5 µl) in sea water (95 µl) and vincristine sulfate were used as negative and positive controls respectively [37]. A suspension of larvae (100 µl) containing 20 live nauplii was added to each well and the covered plate incubated at 29°C. After 24 h, the plates were inspected using a magnifying glass against a black background and the number of survived nauplii were counted. Percentage lethality of the nauplii was calculated for each concentration. The effectiveness of plant product is usually expressed as a median lethal concentration (LC50). This represents the concentration of drug that cause death in half of the test subjects after a certain exposure time. An approximate linear correlation was observed when logarithm of concentration versus percentage of mortality was and the values of LC50 were calculated using Microsoft Excel [37].
2.4. Antibacterial Activity Test
- Antibacterial activity of the plant extracts was tested by paper disc diffusion method [38]. The test organisms used were Staphylococcus aureus (ATCC no. 25923), Bacillus subtilis (local isolate), Escherichia coli (ATCC no. 25922) and Pseudomonas aeruginosa (ATCC no. 10622) which were obtained from Botany Department, Kenyatta University in Kenya. Test bacteria were cultured in nutrient broth medium from stock cultures and later transferred to the nutrient agar in the petri dishes [39]. Nutrients agar (28 g/l) in distilled water was sterilized at 121°C and 15 psi pressure for 20 minutes. Sterilized nutrient agar (15 ml) was dispensed in 90 mm diameter sterile petri dishes to yield a uniform depth of 4 mm. The petri dishes were allowed to cool at room temperature until the culture medium hardened. Using a sterile wire loop, bacteria cultures from stock cultures were scooped and spread on the nutrient agar surface and incubated at 37°C for 24 h. One loop-full of the bacterial strain from the 24 h culture was added to the sterile nutrient broth medium and incubated at 37°C for 24 hours in a rotary shaker [39]. The 24 h broth bacteria culture (0.1 ml) was pipetted into the nutrient agar media in the petri dishes and spread evenly using a sterilized glass rod.Plant extracts (10 µl) of concentration of 200 mg/ml in DMSO were dispensed on 6 mm sterile paper disc [38]. The oven dried (50°C, 1h) discs were firmly placed on the seed agar in the petri dishes using sterile forceps and incubated at 37°C in inverted position. The zones of inhibition were measured after 48 h [40]. Standard antibiotic drugs were used as control.
2.5. Antifungal Activity Test
- Agar-well plate diffusion method was used [41]. Three fungal species, Candida albicans, Penicillium notatum and Aspergillus Niger were obtained from Botany Department, Kenyatta University in Kenya. Portions of sterile potato dextrose agar (15 ml) were dispensed in sterile petri dishes under sterile conditions and left to solidify. Pure cultures of test fungi were introduced in the petri dishes from stock cultures and incubated at 30°C for seven days to produce a good crop of spores. The fungal inoculums were prepared by harvesting the spores from the crop of spores using a sterile spores-harvesting needle and transferred in to a sterile tube containing sterile distilled water. The spore suspension (0.5 ml) was pipetted onto the PDA surface in the petri dishes. The plates were tilted several times to spread the inoculum then left undisturbed for 10 minutes. Using a sterile cork-borer (6 mm), four agar wells were cut out from the inoculated PDA medium. Plant extracts (1 mg) were dissolved in DMSO (50 μl) then made to 1 ml using methanol. The resulting solutions (0.1 ml) were pipetted into the wells in triplicates. The petri dishes were covered, sealed and incubated at 30°C for 72 h after which diameter of zones of inhibition was measured [41].
3. Results and Discussion
3.1. Brine Shrimp Lethality
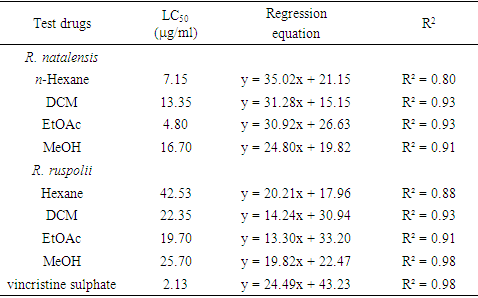
- Root extracts of R. natalensis and R. ruspolii (n-hexane, dichloromethane, ethyl acetate and methanol) were subjected to brine shrimp lethality bioassay for possible cytotoxic action. All the crude extracts exhibited brine shrimp larvicidal activity good (Table 2). Ethyl acetate and n-hexane extracts of R. natalensis were the most lethal, having LC50 values of 4.80 and 7.15 μg/ml, respectively. DCM and methanol extracts of R. natalensis had LC50 values of 13.35 and 16.70 μg/ml respectively. Brine shrimp larvicidal activity displayed by the extracts of R. ruspolii was lower than that of R. natalensis extracts. Ethyl acetate, DCM, methanol and n-hexane extracts of R. ruspolii had LD50 values of 19.70, 22.35, 25.70 and 42.53 μg/ml, respectively. Compared to positive control (vincristine sulphate, LC50 = 2.13 μg/ml), all the extracts tested showed good but lower brine shrimp larvicidal activity. Crude extracts resulting in LC50 values less than 240 μg/ml was considered significantly active and had the potential for further investigation [42]. The cytotoxic activity exhibited by the extracts was promising and this indicates the presence of potent bioactive compounds.
|
3.2. Antibacterial Activity of Extract
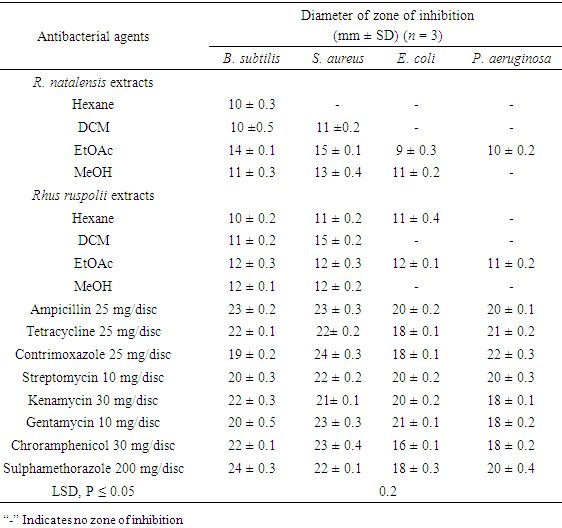
- Plant extracts were subjected to antibacterial test against selected Gram-positive and Gram-negative bacteria (Table 3). All extracts showed moderate activity against Gram-positive bacteria tested except n-hexane extract of R. natalensis which was not active against S. aureus. Ethyl acetate extract of R. natalensis exhibited the highest activity (P ≤ 0.05) against B. subtilis (inhibition zone of 14 ± 0.1mm) followed by ethyl acetate and methanol extracts of R. ruspolii which had 12 ± 0.3 and 12 ± 0.1mm inhibition zones respectively. Hexane extracts showed the least (P ≤ 0.05) antibacterial activity against B. subtilis. Rhus natalensis EtOAc and R. ruspolii DCM extract exhibited the highest against S. aureus (inhibition zone of 15 mm) followed by R. natalensis MeOH extract (inhibition zone of 13 mm) then R. ruspolii EtOAc and MeOH extracts (inhibition zone of 12 mm). Both R. natalensis and R. ruspolii showed antibacterial activity against the Gram-negative bacteria tested.
|
3.3. Antifungal Activity of Extracts
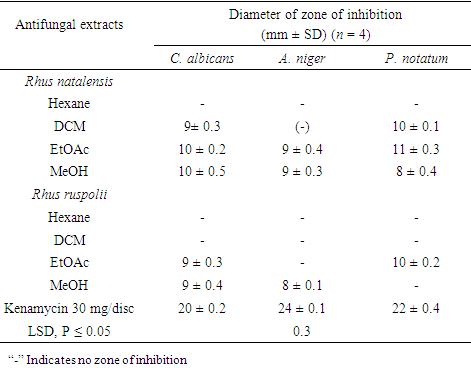
- Hexane, dichloromethane, ethyl acetate and methanol root extracts of R. natalensis and R. ruspolii were tested for antifungal activity against C. albicans, A. niger and P. notatum (Table 4). Five out of the eight extracts tested were active against one or more or the test fungi. Candida albicans and A. niger were most susceptible to EtOAc and MeOH extracts of R. natalensis with inhibition zones of 10 ± 0.2 and 10 ± 0.5 mm (C. albicans) 9 ± 0.4 and 9 ± 0.3 (A. niger) respectively. Rhus natalensis EtOAc extract was the most active against P. notatum (11 ± 0.3 mm) while R. natalensis MeOH extract was the least active (8 ± 0.4 mm) against the pathogen. R. natalensis hexane extract, R. ruspolii. Hexane and DCM extracts did not show any antifungal activity against the test pathogens. R. ruspolii EtOAc extracts inhibited the growth of C. albicans and P. notatum but was ineffective in controlling the growth of A. niger. Candida albicans and A. niger were susceptible to MeOH extract of R. ruspolii but P. notatum was not. The antifungal activity of R. natalensis concur with previous reports [28,43].
|
4. Conclusions
- The findings support the use R. natalensis and R. ruspolii, in treating bacterial and fungal infections. Further studies aimed at isolation and characterization of the bioactive principles is necessary with the hope of getting better antimicrobial agents. It is also necessary to determine the mechanism of action of the extracts.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML