-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Basic Sciences of Medicine
p-ISSN: 2167-7344 e-ISSN: 2167-7352
2018; 7(2): 27-31
doi:10.5923/j.medicine.20180702.02

Effect of Auricular Acupuncture in Sympathetic Point on Heart Rate Variability in Healthy Young Adults under Active Standing Test
José F. Rivas-Vilchis, Tania R. Banderas-Dorantes, José Pablo Akel
Especialización en Acupuntura y Fitoterapia, Universidad Autónoma Metropolitana, Ciudad de México, México
Correspondence to: José F. Rivas-Vilchis, Especialización en Acupuntura y Fitoterapia, Universidad Autónoma Metropolitana, Ciudad de México, México.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Auriculomedicine is applied for acute and chronic pain relief, insomnia, depression, and ailments related to the autonomic nervous system (ANS), among others. Its techniques would modulate the ANS functioning. The heart rate variability (HRV) makes it possible to assess the sympathovagal balance of the ANS under normal conditions or stimulation. The objective of this study was to compare the changes in HRV due to the active standing, before and after the application of acupuncture in the auricular Sympathetic point. Methods. Twenty subjects underwent two consecutive test of active standing (AST) moving from lying supine to standing position. Two consecutive electrocardiographic records of 5 min were made during the active standing test, the first in the supine position and the second in the standing position; before and after the treatment with auricular acupuncture at the Sympathetic point. Results. The HRV parameters in both time and frequency domains underwent significant changes during the standing phases of the AST. When comparing the HRV in the supine position and those after the standing posture maneuver, subjects showed an increase in the LF and LF/HF ratio, and a reduction in HF, PNN50, RMSSD parameters regarding the values in the supine position. These changes were significantly increased by auricular acupuncture. Conclusion. A significant change in sympathovagal equilibrium towards the sympathetic domain presented in the immediate stage after the standing. Moreover, auricular acupuncture enhanced this shift toward the sympathetic dominance.
Keywords: Sympathetic point, Heart rate variability, Active standing test, Autonomic nervous system
Cite this paper: José F. Rivas-Vilchis, Tania R. Banderas-Dorantes, José Pablo Akel, Effect of Auricular Acupuncture in Sympathetic Point on Heart Rate Variability in Healthy Young Adults under Active Standing Test, Basic Sciences of Medicine , Vol. 7 No. 2, 2018, pp. 27-31. doi: 10.5923/j.medicine.20180702.02.
Article Outline
1. Introduction
- Auricular acupuncture has been utilized to treat a wide range of conditions mainly, pain [1, 2], insomnia [3], neurorehabilitation [4]. Some studies have suggested that auriculotherapy would modulate the reticular formation and the autonomic nervous system [5].The evaluation of the function of the autonomic nervous system (ANS) through the heart rate variability has clinical and experimental relevance. One of the main aspects of the method of heart rate variability is the analysis of the frequency domain, based on the knowledge that the heart rate evaluated through the duration of the RR intervals varies significantly even under resting conditions [6]. The sympathetic nerve activity is related with low frequency (LF), and the parasympathetic nerve activity with high frequency (HF), corresponding with frequency fluctuations in the range of 0.04–0.15 Hz and 0.15–0.4 Hz, respectively [6-8]. The LF/HF ratio could either mean the sympathetic modulation or shows sympathovagal balance [7, 8]. Under various conditions such as aging, ANS pathologies, physical or mental stress, these parameters change.Active standing is more suited than a head-up tilt test to assess responses during the initial phase of the orthostatic challenge. It is the best test to diagnose idiopathic orthostatic hypotension and other disorders of the autonomic nervous system [9]. Sympathetic insufficiency or sympathetic withdrawal upon assuming an upright posture (standing), as observed in orthostasis, is abnormal and can present as occasional or frequent dizziness or lightheadedness upon standing [10]. Orthostatic hypotension is an independent risk factor for all-cause mortality and cardiovascular morbidity [11].Recent studies have supported the efficacy of auricular points stimulation to change activity in the sympathetic and parasympathetic nervous system [12, 13]. Also, the relationship between the auricular acupuncture and the vagal regulation has been reviewed [14]. The stimulation of the sympathetic point significantly decreased the stimulus-evoked electrodermal response compared with an auricular stimulation to a non-specific point of the helix [14].We hypothesized that auricular acupuncture at the Sympathetic point would modulate the response to active standing in healthy subjects, thereby changing autonomic nervous. Therefore, this study aimed to evaluate the effect of auricular acupuncture in Sympathetic point on HRV changes during active standing test in healthy volunteers.
2. Participants and Methods
2.1. Participants
- Twenty healthy, adults (12 female), 20 – 40 years of age, (26.5 ± 5.5 in women and 24.5 ± 6.1 in men, age in year ± SD) belonging to the student community of the Universidad Autónoma Metropolitana participated in the study. The subjects had no history of hypertension, diabetes mellitus, renal disease, or other diseases; nor were they taking any medication that could affect the autonomic nervous function. University’s Ethics Committee approved the experimental procedures performed by following the ethical standards laid down in the 2013 Helsinki Declaration. Each subject received detailed information about the nature of the experiment and gave their informed written consent.
2.2. Experimental Protocol
- Testing consisted of four phases as follows:a) Pre-treatment orthostatic test. After 5–10 minutes of rest, subjects in a supine position lying on a bed receive a continuous ECG monitoring for 5 minutes; then subjects were gently assisted into the standing position for a second 5 minutes of ECG monitoring.b) Twenty minutes of sitting rest (recovery).c) Auricular acupuncture treatment.d) Post-treatment orthostatic test, same as a).Medical personnel and an open bed nearby were available should a subject become syncopal. All investigations were performed between 9:00 and 12:00 AM inside a quiet room maintained at 23 to 24°C.
2.3. Assessment of HRV and Data Analysis
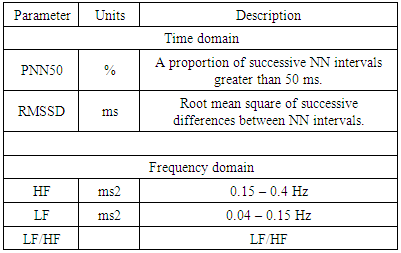
- After a rest period of 10 minutes, segments of the 5-min electrocardiogram were recorded; then amplified, digitized and stored in a computer, using the SphygmoCor device (AtCor Medical, Model EM3, Sydney, Australia). The filtered signals were then analyzed. The device considers only normal heartbeats, ignoring ectopic beats, to derive the statistical parameters from the regular RR intervals (NN intervals) of the electrocardiogram. A standard linear HRV analysis was performed according to the guidelines of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology [15].Parameters of time-domain analysis include the RMSDD that describes short-term variation and thus reflects parasympathetic activity and the PNN50 which significance is similar to RMSDD [16, 17], Table 1. Besides, the following frequency domain parameters: the low frequency (LF, 0.04 to 0.15 Hz); the high frequency (HF, 0.15 to 0.40 Hz); and the LF/HF ratio were analyzed [16, 17], Table 1.
|
2.4. Ear Acupuncture Stimulation and Procedure
- Auricular acupoint Sympathetic on the right ear was selected for acupuncture stimulation. The Sympathetic ear point is on the inside of the helix following the path of the lower part of the antihelix crus (see Figure 1). Auricular acupuncture was performed inserting a stainless steel 0.22 mm diameter, 40 mm long acupuncture needle (HBW Supply Inc., San Jacinto Hemet, CA, USA) into a depth of approximately 0.2 mm, with no additional stimulation, and the needle remained inserted for one minute.
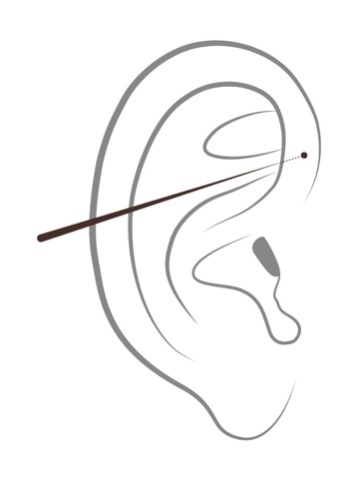 | Figure 1. Sympathetic auricular point |
2.5. Statistical Analysis
- The data are expressed as mean ± standard derivation (SD). Statistical software SPSS version 13.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. Comparisons of heart rate variability before and after active standing were performed using two-tailed, paired Student’s t-tests. P-values of < 0.05 were considered statistically significant.
3. Results
3.1. Pre and Post-treatment HRV in the Active Standing Test
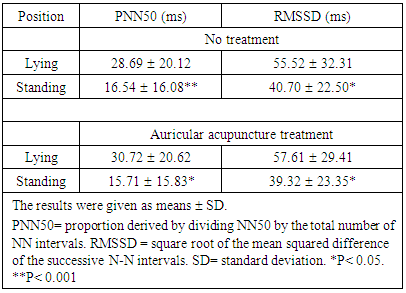
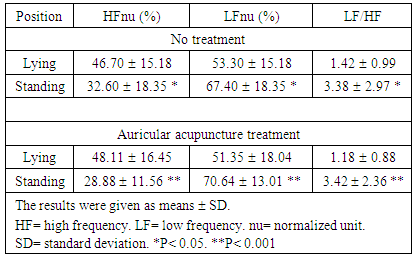
- Regard to time domain parameters, subjects both without treatment and those with the auricular acupuncture treatment had in a significant decrease in PNN50, and RMSSD values after standing as compared with the supine, Table 2.
|
|
3.2. Comparison of HRV Differences Related to Standing in the Phases non treated or treated with Auricular Acupuncture
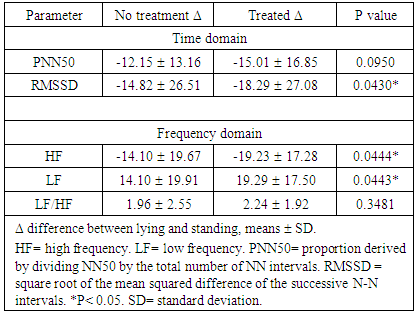
- The HRV components in both time and frequency domains changed in the standing phases. Auricular acupuncture elicited a significant decrease in RMSSD, and HF; besides an increase in LF (p< 0.05) compared with no treatment variables. Otherwise, there was no significant difference in PNN50 or LF/HF, Table 4.
|
4. Discussion
- Orthostatic hypotension is defined as a reduction in systolic or diastolic blood pressure upon standing [18] and generally results from dysfunction of the ANS, medications, or non-neurologic conditions such as cardiovascular disorders causing cardiac failure or hypovolemia [19]. Orthostatic hypotension is one a striking disabling condition, and the treatment must be managed as a process of hierarchical steps that include both non-pharmacological and pharmacological approaches [19, 20]. However, conventional therapies often do not give entirely satisfactory results, there is limited evidence to guide orthostatic hypotension treatment, and recommendations are often based on small cross-sectional trials with acute interventions in neurogenic cases [21].Power spectral analysis of the beat-to-beat variations of heart rate or the heart period (R–R interval) has become widely used to evaluate cardiac autonomic regulation [17, 22-24]. Studies of HRV employed the periodogram or fast Fourier transform (FFT) for power spectral density (PSD). This technique typically identifies two main peaks: low frequency (LF), 0.04–0.15 Hz, and high frequency (HF) 0.15–0.4 Hz. The HF peak is widely believed to reflect cardiac parasympathetic nerve activity while the LF, although more complicated, is often assumed to have a dominant sympathetic component [24]. Despite serious and largely under-appreciated limitations [25], the LF/HF ratio has gained wide acceptance as a tool to assess cardiovascular autonomic regulation, where increases in LF/HF are assumed to reflect a shift to sympathetic dominance and decreases in this index correspond to a parasympathetic dominance [26-29].Our findings regarding the changes in HF and LF/HF as a result of orthostatic challenge coincide with those of previous studies which compared HRV in the supine position and after the tilting postural maneuver or standing [30], this report showed a reduction in the HF and an increase in the LF and LF/HF ratio in healthy individuals. Other study showed that the HRV components in the frequency domain similarly changed during the tilting phases in patients in experimental conditions [31, 32].Studies on the effect of auriculotherapy on sympathovagal balance have shown controversial results. Acupuncture in specific acupoints has been found to significantly increase HRV total by manual ear acupressure in Shenmen [33]. Other study shows that electrical stimulation in the concha seems to be a suitable method for the stimulation of the vagal nerve through auricular electrical stimulation in humans [34]. Otherwise, volunteers showed sympathomimetic effects when underwent a randomized clinical trial with ear acupuncture stimulation in the treatment of obesity [35].The findings of the present study showed that the stimulation of Sympathetic auricular point could enhance the sympathetic activity. These results are in line with the previous hypothesis that the evoked sudomotor response by Sympathetic point stimulation could be related with an enhanced sympathetic activity [36].Orthostatic stress in humans causes changes in the ANS that involve suppression of vagal function and enhanced sympathetic function [37]. The failure of these adaptive mechanisms can cause orthostatic hypotension and other deleterious effects for the patient [38]. Hence, the response observed in this study related to with the application of auricular acupuncture that enhanced a pattern of sympathetic activation and vagal withdrawal during the realization of the active standing test may be useful in patients with an insufficient adaptive response of the ANS.
5. Conclusions
- In summary, we founded a significant shift in sympathovagal balance toward sympathetic dominance in the early stage after standing. Moreover, this shift in sympathetic dominance increased with the auricular acupuncture treatment. The increase in HF and the decrease in LF/HF were considerably more remarkable when the group was treated with auricular acupuncture. Further evaluation of auricular acupuncture in points with cardiovascular effects could provide more insight into its mechanisms of neuromodulation and potentially lead to alternative approaches for treating orthostatic hypotension.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML