-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Basic Sciences of Medicine
p-ISSN: 2167-7344 e-ISSN: 2167-7352
2015; 4(2): 28-30
doi:10.5923/j.medicine.20150402.02
Effect of Obesity on the Pulmonary Functions of the Adolescents
Mohamed Hanea Mohamed Rezk1, Ahmed Sayed Khashaba2
1Demonstrator, Riyadh Colleges of Dentistry and Pharmacy, B.Sc in Pharmaceutical Sciences
2Assistant Professor- Physiology Medicine, Riyadh Colleges of Dentistry and Pharmacy
Correspondence to: Ahmed Sayed Khashaba, Assistant Professor- Physiology Medicine, Riyadh Colleges of Dentistry and Pharmacy.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
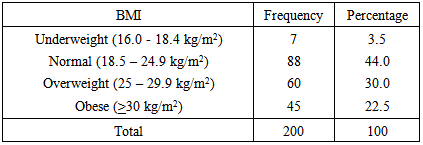
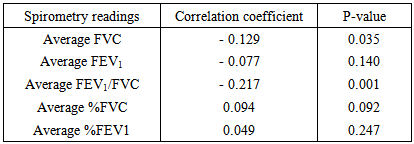
Objective:To explore the effect of obesity on the pulmonary function of adolescents. Methodology: This study was conducted at Riyadh Colleges of Dentistry and Pharmacy (RCsDP), Saudi Arabia, during the period from January 2013 till April 2014. A simple random sample of 200 adolescent students were assessed. Three study questionnaires were used for data collection, i.e., personal characteristics questionnaire; case-finding questionnaire and the Medical Research Council (MRC) Dyspnea Scale. Spirometry was performed onto the participants, using Spirolab III machine. Results:Age of participants ranged from 17 to 19 years. Prevalence of overweight and obesity were high among adolescent students (30% and 22.5%, respectively). Body mass index correlated negatively and significantly with average FVC and average FEV1/FVC (-0.129, p=0.035 and p=-0.217, p=0.001, respectively). Conclusions: Obesity may have a negative effect on pulmonary function of male adolescents. Weight loss is recommended to prevent the possible negative impact of obesity on pulmonary function of adolescent males.
Keywords: Obesity, Pulmonary Functions, Adolescents
Cite this paper: Mohamed Hanea Mohamed Rezk, Ahmed Sayed Khashaba, Effect of Obesity on the Pulmonary Functions of the Adolescents, Basic Sciences of Medicine , Vol. 4 No. 2, 2015, pp. 28-30. doi: 10.5923/j.medicine.20150402.02.
1. Introduction
- Obesity is one of the risk factors that are responsible for many diseases and disorders that include myocardial infarction, congestive heart failure and metabolic disorders. It has been reported that in the United States, the prevalence for obesity from 1976 to 1980 and from 1988 to 1994, has significantly increased [1]. In addition, results collected over a period of 46 years, from 1960 to 2006, have shown that the percentage of men and women affected by obesity ranged from 10-34% and from 15-36% respectively [2]. The National Heart, Lung and Blood Institute in 1998 reported that overweight and obesity have been shown to cause sleep apnea and other abnormal respiratory conditions. A significant decrease in functional residual capacity (FRC) and expiratory reserve volume (ERV) has been reported in obese patients. Increased body mass index (BMI) has been reported to raise pulmonary arterial pressure [3]. Childhood obesity has been shown to be a predictor of adulthood obesity, and obesity-related complications, such as cardiovascular diseases and metabolic disorders [4]. A high BMI in a child could significantly contribute to obesity, which might augment as the child keeps on growing up. The incidence of obesity among adolescents has moved toward the higher side over the last three decades [5].The increasing prevalence of childhood obesity is due to social changes. Unlike most adults, children and adolescents cannot choose the environment in which the food they eat and live. They also have a limited ability to understand the long term consequences of their behavior. Therefore, they need special attention in the fight against the obesity epidemic [6, 7].In Saudi Arabia, several studies explored complications of obesity. Mosli et al. [8] reported that obesity is associated with metabolic disorders, while Habib [6] found that prevalence of obesity was also accompanied by poor fitness, whereas Al-Rethaiaa et al. [7] noted that 18-24 year old male college students were shown to have high BMI levels between the classes of overweight and obesity. However, the impact of obesity on pulmonary function of adolescents remains to be explored. Therefore, this study aimed to explore the effect of obesity on the pulmonary function of adolescents.
2. Methodology
- A cross-sectional study design has been followed. The study was conducted during the period from January 2013 till April 2014. The study was carried out at the Riyadh Colleges of Dentistry and Pharmacy (RCsDP), Riyadh City, Saudi Arabia. Thre data collction tool comprised three parts, i.e., a "personal characteristics" questionnaire; and a "case-finding" questionnaire (which were constructed by the researchers), in addition to the "Medical Research Council dyspnea scale" [9]. The sample size for the present study was determined using "GPower" software to be 200 subjects. A simple random sample was followed to include 200 students (aged 17-19 years) in this study. Subjects with associated chronic diseases co-morbidities (e.g., diabetes, hypertension, renal or heart disease) were excluded.Weight and height of each participant student were measured. Each student's BMI was calculated as his weight (in kg) divided by his squared height (in m2) [10]. BMI values were correlated with FEV1, FVC and FEV1/FVC to test any significant correlation between obesity and pulmonary function parameters. Spirometry was applied to all participants using the Spirolab III machine. Common measurements included:• Forced Expiratory Volume for the 1st second (FEV1): volume of air forced out in one second [11]. • Forced Vital Capacity (FVC): volume of air forced out after maximum inhalation. • The ratio between FEV1 and FVC (FEV1/FVC) [11].Spirometry was performed three times for each participant student. FEV1 and FVC readings were also compared as a percentage of their predicted values (%FVC and %FEV1, respectively). The mean values of the three readings for FEV1, FVC, FEV1/FVC, %FVC and %FEV1for each student were calculated.The statistical analysis for collected data was carried out using the Statistical Package of Social Sciences (SPSS) version 21. Descriptive statistics (i.e., frequency and percentage) were calculated. Pearson's correlation coefficients between BMI and variables of pulmonary function tests were calculated. P-values less than 0.05 were considered as statistically significant.
3. Results and Discussion
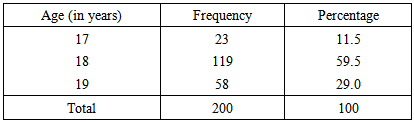
- Age groups of participant students are shown in Table (1). All participants belonged to the late adolescence age period (i.e., 17-19 years).
|
|
|
4. Conclusions
- Obesity may have a negative effect on pulmonary function of male adolescents. Weight loss is recommended to prevent the possible negative impact of obesity on pulmonary function of adolescent males.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML