-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Basic Sciences of Medicine
p-ISSN: 2167-7344 e-ISSN: 2167-7352
2014; 3(1): 1-7
doi:10.5923/j.medicine.20140301.01
Is Variant Anatomy of Atlas Clinically Important? A Review
Singh Rajani
Department of Anatomy, All India Institute of Medical Sciences, Rishikesh, 249201, India
Correspondence to: Singh Rajani, Department of Anatomy, All India Institute of Medical Sciences, Rishikesh, 249201, India.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Atlas occupies the most important and vital position interfacing skull cranially and axis caudally constituting atlanto-occipital and atlanto-axial joints. So it helps in complex biomechanical movements of skull and neck along with weight transmission of skull to spine. Besides this it paves the way for spinomedullary junction through vertebral foramen, vertebral artery and first cervical nerve over superior surface of posterior arch making it more vulnerable. Above mentioned reasons may make atlas most favorable for anatomical variations of all the vertebrae. Thus any of these anatomical variations of atlas causing pathology thereby clinical complication will be of paramount importance for health scientist and medical professionals. It is therefore necessary to make the health caring scientists and doctors to update the knowledge of the morphological variants consisting of occipitalization, cleft, hypoplasia and aplasia of anterior and posterior arches, bridging of vertebral groove and foramen transversarium of atlas. These morphological variations in atlas vertebra are related to bundle of clinical complications. This systematic review analyses available information on the clinical anatomy of the atlas vertebra. A literature search using electronic databases and standard anatomy references text books was conducted. The search was restricted to English language only. The study will be of paramount importance to Anatomists, clinicians and radiologists for updating their knowledge of current developments in this field.
Keywords: Atlas, First cervical vertebra, Atlanto-occipital joint, Axis, Atlanto-axial joint
Cite this paper: Singh Rajani, Is Variant Anatomy of Atlas Clinically Important? A Review, Basic Sciences of Medicine , Vol. 3 No. 1, 2014, pp. 1-7. doi: 10.5923/j.medicine.20140301.01.
Article Outline
1. Introduction
- Atlas vertebra was named after Atlas, the great titan of Greek mythology, who was supposed to hold the globe of universe on his head as first cervical vertebra supports the globe of the head. Atlas is the most superior cervical vertebra of the spine. Atlas vertebra (Fig.1) is ring like structure, consisting of anterior and posterior arches including two lateral masses along with transverse processes. Two lateral masses bear a kidney shaped superior articular facets which articulate with occipital condyles to form atlanto-occipital joint. Inferior articular facets of these lateral masses are almost circular and flat. It is oriented more obliquely to the transverse plane than the superior articular facet and faces more medially. Inferior articular facets of atlas form lateral atlanto-axial plane joint. On medial surface of each lateral mass is a rough area which bears vascular foramina and a tubercle for the attachment of transverse ligaments[1]. In adults the distance between these tubercles is shorter than length of the transverse ligament with a mean of 16 mm.The anterior arch which forms anterior 2/5 of ring is slightly convex anteriorly and bears anterior tubercle. The anterior longitudinal ligament and longus colli muscles are attached to anterior tubercle. Its upper border provides attachment to the anterior atlanto-occipital membrane which often gets ossified. The posterior surface of the anterior arch bears concave circular facet for dens[1].
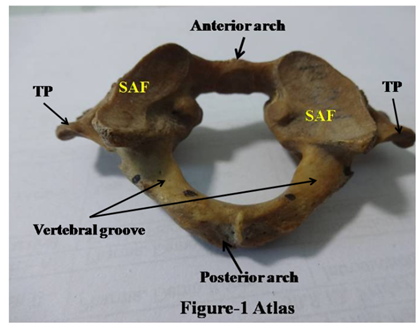 | Figure 1. Atlas, SAF stands for superior articular facet TP for Transverse process |
2. Material and Methods
- Literature search was conducted using the following databases as appended below:Scielo, Scopmed, medline, PubMed and Wiley online library. Papers containing original data were selected and secondary references retrieved from bibliographies. The search was restricted to English language articles and selected anatomy reference text books. Search terms used for surfing the literature were-1. Atlas- the first cervical vertebra2. Morphometry of atlas3. Occipitalisation or assimilation of atlas vertebra4. Bridging of vertebral groove5. Morphometry of vertebral groove6. Anatomy of atlas vertebra7. Atlanto-occipital joint8. Variant anatomy of atlas vertebra 9. Variant anatomy of anterior arch of atlas vertebra10. Variant anatomy of posterior arch of atlas vertebra
3. Results
- The following account of atlas vertebra is based on the analysis of the retrieved literature under headings- description of anomalies of atlas vertebra, etiology and clinical significance related to these anomalies.
3.1. Anomalies Associated with Atlas Vertebra
- Occipitalization of atlas is congenital bony fusion of the atlas vertebra with the base of the occipital bone of the skull. This involves superior articular facets, anterior and posterior arches or complete atlas vertebra[2]. The incidence of atlanto-occipital fusion (assimilation or occipitalization) ranges from 0.14% to 0.75% of the population, both sexes being equally affected[3,4,5]. Partial fusion is more common. Occipitalization was first described by Rokitansky in 1844. This was later demonstrated roentgenographically by Schüller in 1911. The authors[6, 7, 3, 8, 9, 10, 11, 5] also reported this bony abnormality involving neurovascular complications due to occipitalization. The assimilation of atlas vertebra creates difficulty in mobility of skull with respect to spine. But absolute immobility of an occipitalized atlanto-occipital joint results in compensatory hypermobility between the atlas and axis. This hypermobility in atlanto-axial junction may create abnormalities in atlas and axis vertebrae at their interface due to over use of this junction. Approximately 50% of patients with atlanto-occipital fusion develop atlanto-axial instability[12] and concurrent subluxation[13]. Vertebral artery anomalies with atlanto-occipital fusion were observed by Bernini et al. (1969)[14].
3.2. Anomalies of Anterior and Posterior Arches of Atlas Vertebra
- Congenital anomalies in arches of the atlas are rare and usually discovered incidentally. Anomalies of anterior and posterior arches include cleft (Fig-2A, 2B), partial aplasia, hypoplasia (Fig.3A) and complete agenesis (Fig.3B).
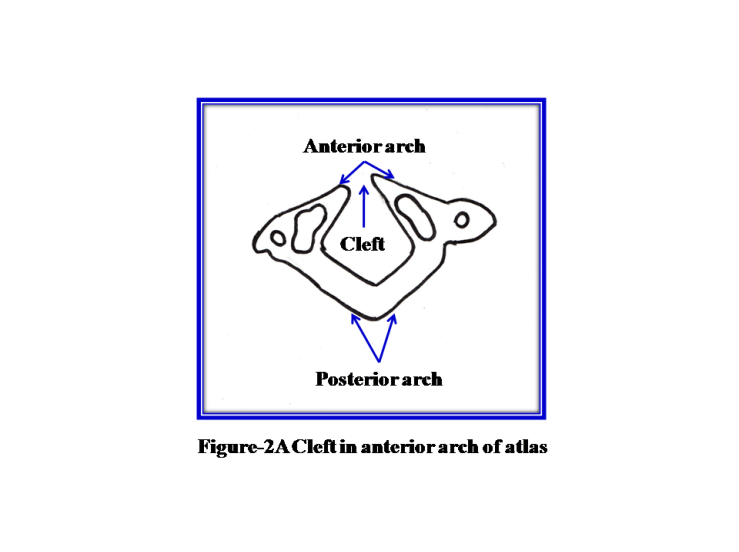 | Figure 2A. Cleft in anterior arch of atlas |
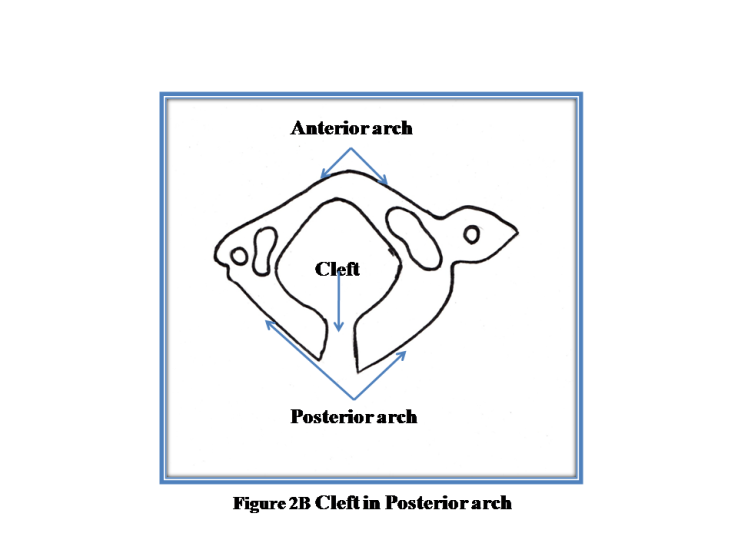 | Figure 2B. Cleft in Posterior arch |
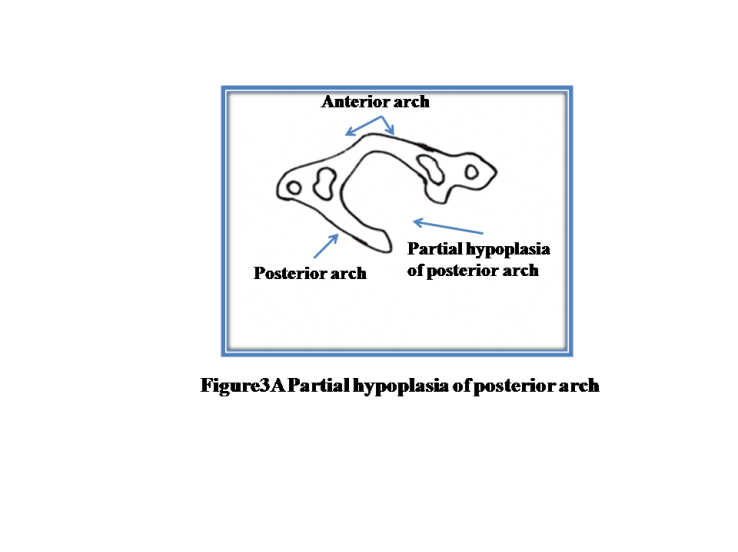 | Figure 3A. Partial hypoplasia of Posterior arch |
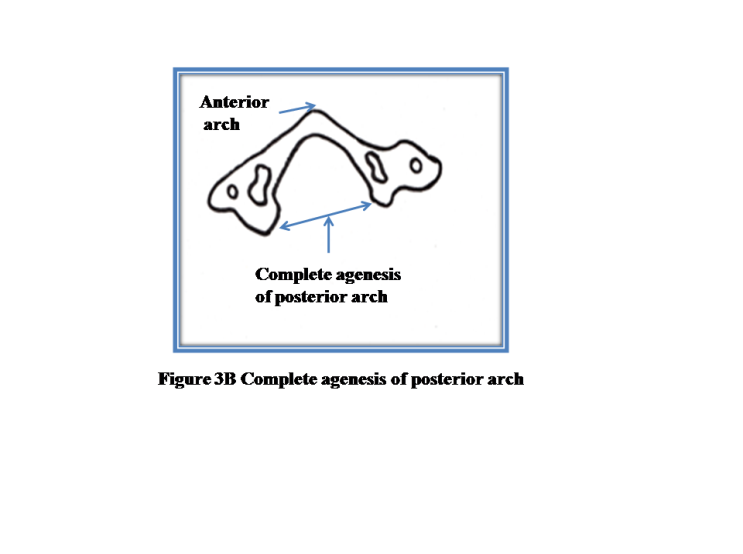 | Figure 3B. Complete agenesis of Posterior arch |
3.3. Anomalies of Vertebral Groove
- The Vertebral groove has been seen bridged by ossification named as ponticulus posticus which extends from the lateral mass to posterior arch of atlas. The existence of the ponticulus posticus has been demonstrated in a study in which lateral cephalometric x-ray films have been examined in 1963. This foramen thus formed has been classified as complete or incomplete foramen depending upon the complete or partial ossification. The complete foramen (Fig.4) is called “Kimmerle anomaly”.
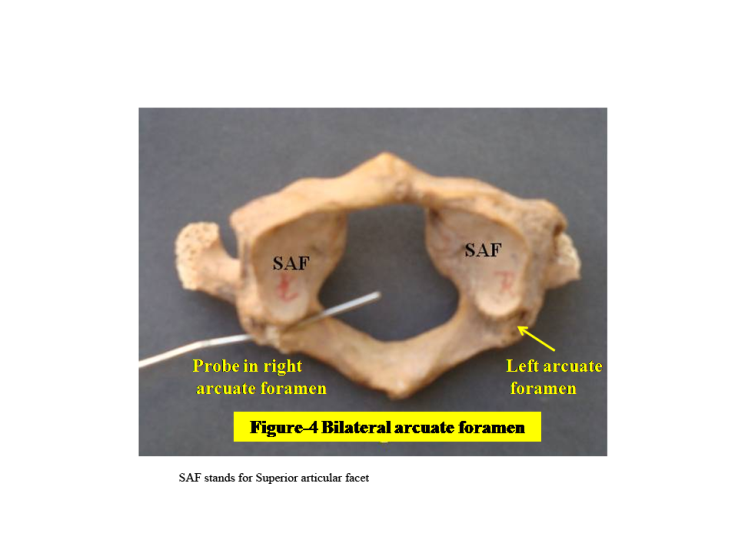 | Figure 4. Bilateral Arcuate Foramen |
3.4. Foramen Transversarium
- The costal elements sometimes remain deficient leaving the foramen transversarium open anteriorly. Double foramen transversarium has also been reported[29, 30]. According to them one foramen transmitted vertebral artery and second vein. Foramen transversarium was also described to be divided by a fibrous or bony bridge separating the artery and vein. An accessory foramen transversarium on the posterior arch of atlas vertebra was reported altering the course of vertebral artery and even led to its compression[31].
4. Etiology of Variant Anomalies of Atlas
4.1. Occipitalization
- Barge demonstrated that the atlanto-occipital joint was intersegmental and not segmental[8]. Tachdjian (1990)[32] mentioned that the dense caudal part of the fourth occipital somite apparently united with the cephalic part of the subjacent somite resulting in atlanto-occipital fusion. According to Chandraraj and Briggs (1992)[33], occipitalization was due to an interruption in the differentiation of the occipito-cervical somites early in the embryonic period. The caudal portion of the first cervical sclerotome mainly gave rise to the neural arch (posterior arch) of the atlas and the hypochordal bow becomes the anterior arch.
4.2. Anterior and Posterior Arches
- Congenital hypoplasia of the posterior arch of the atlas vertebra, a developmental failure of chondrogenesis was a rare anomaly and may range from partial clefts to total agenesis of the posterior arch. Ossification of the posterior arch usually occurred between the 3rd and 5th years of life. Pax9 was expressed in cells fated to form posterior arch (neural arch) which was responsible for proliferation of cells in this region. Further, an increased apoptosis was observed in Pax1/ Pax9 deficient mice[34]. Partial hypoplasia/ complete agenesis might be either due to decreased cell proliferation or increased cell death as Pax1/Pax9 genes are required to maintain high rate of cell proliferation during sclerotome development. Thus there might be under expression/complete deletion of Pax9 gene in this region. Similarly various defects of anterior arch might be caused by deletion/mutation of Pax1 in varying degree.
4.3. Causes of Formation of Arcuate Foramen
5. Clinical Significance
- (1) Occipitalization of the atlas is commonly associated with concomitant neurovascular and skeletal anomalies at the craniovertebral junction. Occipitalization of the atlas is an important congenital malformation of the craniovertebral region because of its proximity to the spinomedullary region with the possibility of a neurological compression syndrome.Occipitalization of the atlas can produce a wide range of neurological signs and symptoms which vary from transitory headache to a full blown neurological syndrome. Cervical cord compression is due to the soft tissue and bony abnormalities associated with occipitalization of the atlas. This leads to weakness, ataxia of the lower extremities and nystagmus. Numbness and pain in the upper extremities is a prominent complaint[2]. Objective findings chiefly comprise hyperreflexia, positive Babinski and Hoffmann reflexes, weakness and other long-tract signs in both the upper and lower extremities. Sensory findings are less frequent. Occipitalization may result in vertebral artery compression or even total occlusion leading to dizziness, seizure etc. The assimilation of the atlas with the occipital bone is generally associated with bony torticollis[7, 36, 32] due to constraints of mobility.For diagnosis of assimilation/occipitalization of atlas, some degree of bony union between the skull and the atlas is necessary to be demonstrated[8]. Probable criteria for differentiating occipitalization of the atlas from manifestations of an occipital vertebra (third occipital condyles, a paracondyler process, a transverse basioccipital fissure, basilar process and bipartite atlantal facets) is based on the position of the hypoglossal, suboccipital nerves and the vertebral artery (2).(2) Cleft, hypoplasia and aplasia of anterior and posterior arches may be mistaken for fractures. Therefore when upper cervical anomalies are found in a young patient, the patient should be evaluated in detail with advanced radiological studies to avoid misinterpretation of cleft, hypoplasia and aplasia for fractures, subluxation, osteolysis or instability. Klimo et al[16] described a case of congenital partial aplasia of the posterior arch of the atlas causing myelopathy. Patient came with complaint of Lhermitte sign, only with extension of his neck and an episode of temporary quadriparesis with a minor fall. Currarino et al.[17] described seven cases having defects of posterior arch. In three patients the anomaly was discovered as an incidental asymptomatic finding; three other patients presented with transient neck pain or transient neurologic symptoms after head and neck trauma and one patient (an adult woman) described neck symptoms of 1-year duration. Garg et al[37] described a case of bipartite atlas with os odontoideum in patient with weakness and numbness of all four limbs after sustaining a minor head trauma. Radiographs of cervical spine revealed aplasia of anterior arch of atlas, ventral displacement of C1 over C2 on flexion which reduced on extension. CT scan showed anterior arch aplasia, posterior arch midline defect, and os odontoideum which had a small projection on the anterior surface at the level of anterior arch. The clinical symptoms due to variant defects of posterior arch of atlas are caused due to involvement of first cervical nerve and part of cervical spinal cord passing through vertebral foramen of atlas vertebra. The complaints of tremor, hyperesthesia of lower limbs followed by quadreparesis after experiencing minor head trauma were observed by Choi et al.,[15] in patients with congenital cleft of anterior arch and partial aplasia of the posterior arch of the atlas vertebra.
5.1. Arcuate Foramen
- The vertebral artery is vulnerable to compression during external rotation of head and neck as in the manipulation of cervical spine. This situation may be aggravated by presence of posterior or lateral bridge of the atlas and result in compromised blood flow.Some spine surgeons reported that during lateral mass screw fixation/ insertion severe complications like vertebral artery injury occurred. The possible cause may be presence of posticus ponticle or arcuate foramen. Therefore proper identification of this anomaly on preoperative lateral radiographs should alert surgeons to avoid using ponticulus ponticus as a starting point for lateral mass screw fixation. As it vary in size and shape, 3D CT scanning should be considered before planning lateral mass screw placement into the posterior arch[38]. Some patients with this anomaly have complained neck pain, headache, dizziness etc. If patient comes with above symptoms, presence of ponticulus ponticus should also be kept in mind. Vertebral artery may be injured during posterior approaches to the cranio-vertebral junction especially during lateral dissection and decompressive C-1 laminectomy. The arches of C-1 and C-2 are widely exposed during some procedures and injury to the vertebral artery as it passes above the C-1 arch through the suboccipital triangle should be avoided. Various suggestions have been made as to how far exposure should be made laterally during dissection to avoid vertebral artery injury. Exposure of the posterior arch of the atlas is an important step in surgical procedures for treatment of diverse conditions of the upper spinal cord and foramen region. According to Tulika[39] a minimum of 1.5 cm of the posterior arch could be safely exposed at both outer and inner cortices. In addition with mobilization of the vertebral artery from its groove on both the sides, an additional 1 cm of posterior arch could be exposed on either side.Stayffer[40] has recommended that the soft tissue attachment on the posterior ring of the atlas be separated approximately 1 cm from the midline bilaterally to prevent vertebral artery injury during a deeper dissection. Various authors have quoted the safe zone for surgical manipulations on the posterior arch of the atlas to avoid iatrogenic injury to the vertebral artery. According to Simpson et al[41], the surgical exposure of the posterior arch should not exceed 15 mm from the midline in adults and 10 mm in children. Max franco de carvalho[42] suggested that the posterior dissection of the posterior arch should be limited to a distance of 11.2 mm from the midline. Stauffer[40] recommends a safe zone of 10 mm from the posterior midline. Ebraheim et al[43] noted the safe zone as 10 mm for males and 9 mm for females from the posterior midline. All these data belong to the Western literature. However, the standard textbooks on posterior exposure suggest a safe distance of 15 mm from the midline[44].Lateral mass screw for the fixation of the atlas has become common for the treatment of atlantoaxial instability. Some surgeons have recommended that in the presence of a broad posterior arch of the atlas, the insertion of the screw be started in the dorsal aspect of the posterior arch instead of at the base of the lateral mass or at the junction of the posterior arch and the lateral mass[45]. A broad dorsal arch of the atlas is the best indication for this modified screw trajectory. The ponticulus posticus/arcuate foramen carrying vertebral artery can be mistaken for a broad dorsal arch and the surgeon may insert the screw into the ponticulus posticus[45]. This may result in injury to the vertebral artery and lead to stroke or even death by thrombosis, embolism or arterial dissection [45]. Therefore the presence of this anomaly should be carefully checked before screw placement in the lateral mass of the atlas to avoid vertebral artery injury. Bridges and ponticulus normally occur in monkeys and lower animals. In quadrupeds, the superior margin of posterior bridge provides greater surface area for the attachment of posterior atlanto- occipital membrane helping to support the weight of head. In human beings the weight is received by the superior articular facets of the atlas, thus the bridge has disappeared.
5.2. Foramen Transversarium
- (4) The presence of double foramen transvesarium may be correlated with duplicate vertebral artery. This may create confusion to surgeons during surgery around this region and misinterpretation of radiographs. An accessory foramen transversarium on the posterior arch of atlas vertebra can lead to symptoms like headache, migraine and fainting attacks[31]. Open foramen transversarium anetriorly may expose the vertebral vessels which are at risk of being damaged.Thus normal and variant anatomy of atlas is of paramount importance to clinicians for various types of pathologies associated with atlas, for surgeons for carrying out surgical procedures around this region, radiologists for avoiding misinterpretation of radiographs and anatomists for the source of database.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML