-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Basic Sciences of Medicine
p-ISSN: 2167-7344 e-ISSN: 2167-7352
2013; 2(1): 21-23
doi:10.5923/j.medicine.20130201.04
Injury Risk of Vertebral Artery during Screw Placement through Atlas Posterior Arch
Gamal H. El-S. Hassanein
Department of Anatomy, faculty of Medicine, Zagazig University, Postcode 44519, Zagazig, Egypt
Correspondence to: Gamal H. El-S. Hassanein, Department of Anatomy, faculty of Medicine, Zagazig University, Postcode 44519, Zagazig, Egypt.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Screw placements into atlas lateral mass requires a detailed anatomy of the vertebral artery on the posterior arch of atlas (C1). This study was designed to determine the potential risk of injuring the vertebral artery during atlantoaxial fixation via the atlas posterior arch and assess the feasibility this site for screw insertion. Five parameters of the vertebral artery groove (VAG) were performed in thirty six adult dry atlas vertebrae of unknown sex using a Vernier sliding caliper. The distances, starting from the posterior midline, to the medial most edge of VAG on the inner and outer cortexes of posterior arch were 11.90 ± 2.97 mm and 17.58 ± 3.75 mm respectively, and to the lateral most edge of the VAG on the inner and outer cortexes were 16.30 ± 3.67 mm and 18.71 ± 3.64 mm respectively. The thickness of posterior arch at VAG was 3.99 ± 1.13 mm, with a total of 29 (80.6%) specimens were less than 5mm. In conclusion, the thickness of the lateral part of the posterior arch of atlas (C1) vertebra is not suitable for screw insertion in most cases and to avoid vertebral artery injury, the dissection should remain within 10 mm and 6mm lateral to the midline on the posterior and superior aspects respectively.
Keywords: Vertebral Artery Injury, Atlas Posterior Arch, Screw Fixation into C1 Posterior Arch, Vertebral Artery Groove
Cite this paper: Gamal H. El-S. Hassanein, Injury Risk of Vertebral Artery during Screw Placement through Atlas Posterior Arch, Basic Sciences of Medicine , Vol. 2 No. 1, 2013, pp. 21-23. doi: 10.5923/j.medicine.20130201.04.
1. Introduction
- The vertebral artery arises from a postero-superior position on the subclavian artery and the left side may arise from the arch of aorta (9%). Then it runs cephalad and posteriorly to enter the protective bony encasement of the vertebral column via the transverse foramen , usually at the level of the sixth cervical vertebra, but occasionally at a higher level[1]. It continues superiorly through the foramina of the fifth through the first cervical vertebra. At the superior border of the first cervical vertebra , the artery curves medially, crosses the posterior arch of the first cervical vertebra, and passes through the foramen magnum to enter the posterior cranial fossa[2]. The course of vertebral artery on C1 lamina complicates surgical procedures in this area[3]. The injury to the artery during surgery can lead to catastrophic intra-operative bleeding and compromise to the blood flow can lead to unpredictable neurological deficits, which will depend on the adequacy of blood flow from the contralateral vertebral artery[4]. Vertebral artery injury in posterior cervical surgery can occur with transarticular screw insertion and during lateral mass platting , as well as during exposure over the superior part of the posterior ring of atlas[5]. The increasing use of C1 (atlas) lateral mass screw placements for atlantoaxial fixation requires a detailed anatomy of the lateral mass and the relation of the entry zone to the vertebral artery[6]. This study was designed to determine the potential risk of injuring the vertebral artery during atlantoaxial fixation via the atlas posterior arch and assess the feasibility this site for screw insertion.
2. Material and Methods
 | Figure 2. The thickness (T) of the lateral part of the posterior arch of atlas vertebra at VAG (double-headed arrow) |
3. Results
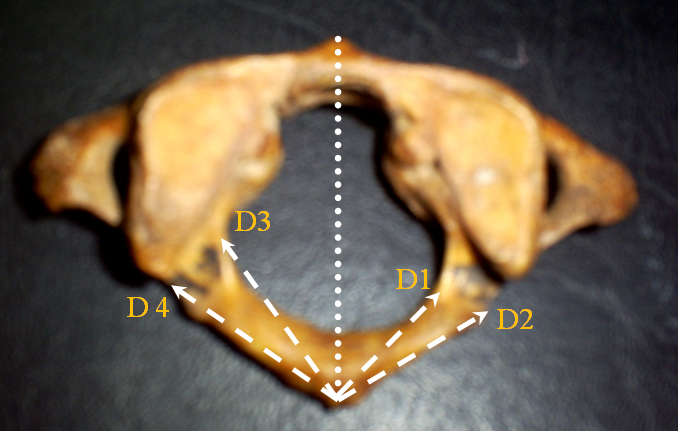
- The distances from posterior midline to the medial most edge of the VAG on the inner cortex (D1) was 11.90 ± 2.99 mm and on the outer cortex (D2) was 17.58 ± 3.75 mm. The distances from posterior midline to the lateral most edge of the VAG on the inner cortex (D3) was 16.30 ± 3.67 mm and on the outer cortex (D4) was 18.71 ± 3.64 mm. The higher values on the left side, based on t- test, were statistically non-significant (P ≥ 0.05) (Table 1).
|
|
4. Discussion
- The surgical importance of vertebral artery on the posterior arch of atlas vertebra during posterior cranio-vertebral procedures is well-known. Cacciola et al[4] described that the artery makes a loop after its exit from foramen transversarium of C1, then occupies a vertebral artery groove over the surface of the posterior arch of atlas and in this location it is vulnerable to injury during a posterior midline approach. Ebraheim et al[7], to define a safe zone from the posterior midline to avoid injuring the vertebral artery, described a mean distance of 10.4 ± 1.7 mm (males) and 8.9 ± 0.8 mm (females); with a minimum of 8 mm for both genders, from the posterior midline to the medial most edge of VAG on the inner cortex, and described a mean distance of 19.2 ± 3.2 mm (males) and 16.5 ± 1.0 (females) ; with a minimum of 12 mm for both genders, from the posterior midline to the medial most edge of VAG on the outer cortex. The previous authors suggested, according to their findings, that dissection on the posterior aspect of the posterior ring should remain within 12 mm lateral to the midline, and that dissection on the superior aspect of the posterior ring should remain within 8 mm of the midline. The current study, in contrast to Ebraheim et al[7], revealed lower values for distances from the midline to the medial-most edge of the vertebral artery groove on the inner and outer cortex respectively; 11.90 ± 2.97 mm, with a minimum of 5.96 mm and 17.58 ± 3.75 mm, with a minimum of 9.65 mm (Table 1). Accordingly it is suggested, to avoid injury of vertebral artery, that safe dissection of the posterior aspect of the posterior arch should remain within about 10 mm lateral to the midline and should remain within about 6 mm of the midline on the superior aspect. However, higher values for distances from the midline to the medial-most edge of the vertebral artery groove on the outer cortex were reported ; 15.03 ± 1.22 mm[3] , approximately 16 mm[8] and an average of 18.2 mm[4].Concerning the thickness of the lateral part of the posterior arch at position of VAG , Tan et al[11] regarded it as other vertebral pedicle through which the screw fixation could be achieved and described a thickness of 4.58±0.65 mm (left side) and 4.72 ± 0.68 mm (right side) at the thinnest part of the groove with only 8% (4 out of 50) were less than 4mm. On the other hand, Ma et al[12] described a mean a thickness of 3.88±0.52 mm on the medial one-third portion of the posterior arch under VAG and 4.25 mm±0.51 mm on its lateral one-third portion of the arch. The same authors reported that the lateral one-third portion of the posterior arch under VAG would be ideal for screws to minimize the risk of injury to the vertebral artery in the groove. In the current study, a mean thickness of 3.99±1.13 mm of the lateral part of posterior arch at the groove was revealed which is slightly greater than the findings of Lee et al[10] , but less than the findings of Ebraheim et al[7]; Ma et al[12]; and Tan et al[11] with the latter authors showing the largest thickness (Table 4 & figure 3).
|
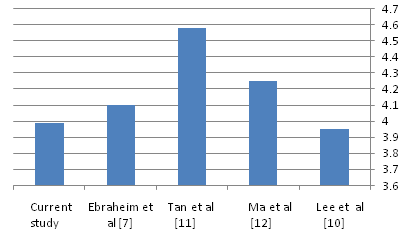 | Figure 3. Histogram of the thickness of the lateral part of the posterior arch of atlas vertebra at VAG in current study compared to previous studies |
5. Conclusions
- The bone thickness of the lateral part of the posterior arch of atlas (C1) vertebra is not suitable for screw insertion in most cases and to avoid vertebral artery injury, the dissection should remain within 10 mm and 6mm lateral to the midline on the posterior and superior aspects respectively.
References
| [1] | Foreman S.M., and Croft A.C., Whiplash Injuries. The cervical acceleration/deceleration syndrome, 3rd edition. Lippincott Williams & Wilkins: p316, 2002. |
| [2] | Pearl M.S., Vascular interventions: vascular anatomy of the upper extremity: Vertebral artery. In: Image-guided interventions, Volume I, 1st edition. Editors: Mauro et al. Saunders Elsevier: p 366, 2008. |
| [3] | Naderi S., Çakmakçi H., Acar F.,Arman C., Metrol T., Arda M.N., Anatomical and computed tomographic analysis of C1 vertebra. Clinical Neurology and Neurosurgery; 105 (4): 245- 248, 2003. |
| [4] | Cacciola F., Phalke U., Goel A. ,Vertebral artery in relationship to C1-C2 vertebrae: An anatomical study. Neurology India 52(2): 178 – 184, 2004. |
| [5] | Evans R.W. , Vascular injuries in spine surgery In: Neurology and Trauma, 2nd edition, Oxford university Press: p 757, 2006. |
| [6] | Gupta T. , Cadaveric morphometric anatomy of C-1 vertebra in relation to lateral mass screw placement. Surg Radiol Anat 30 : 589 – 593, 2008 |
| [7] | Ebraheim N.A., Xu R., Ahmad M., Heck B., The quantitative anatomy of the vertebral artery groove of the atlas and its relation to the posterior atlantoaxial approach. Spine 23(3): 320-323, 1998. |
| [8] | Gupta T., Quantitative anatomy of vertebral artery groove on the posterior arch of atlas in relation to spinal surgical procedures. Surg Radiol Anat 30: 239–242, 2008. |
| [9] | Carvalho M.F., Rocha R.T., Monteiro J.T.S., Pereira C.U., Leite R.F., Defino H.L.A., Vertebral artery groove anatomy. Acta Ortop Bras 17(1): 50-54, 2009. |
| [10] | Lee M.J., Cassinelli E., Riew D. , The feasibility of inserting atlas lateral mass screws via the posterior arch. Spine; 31 (24): 2798-2801, 2006. |
| [11] | Tan M., Wang H., Wang W., Zhang G., Yi P., Li Z., Wei H., Yang F., Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine 28 (9): 888-895, 2003. |
| [12] | Ma X-Y., Yin Q-S., Wu Z-H., Xia H, Lu J-F. , Zhong S-Z., Anatomic considerations for the pedicle screw placement in the first cervical vertebra. Spine 30 (13) : 1519-1523, 2005. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML